IJCRR - 8(4), February, 2016
Pages: 29-33
Date of Publication: 21-Feb-2016
Print Article
Download XML Download PDF
HISTOPATHOLOGICAL PATTERN AND RELATIVE FREQUENCY OF OVARIAN MASSES IN TERTIARY CARE HOSPITAL
Author: Shreedhan G. Prajapati, Smita A. Shah, Nirali S. Amin, Hansa M. Goswami
Category: Healthcare
Abstract:Introduction: Ovarian tumours are one of the major causes of gynaecological problems in females and present marked variation in their histological types. Relative frequency of these lesions is different for Western and Asian countries. This study was designed to find out frequency of various histological patterns of ovarian tumours in patients attending Pathology Department of Tertiary care Hospital.
Material and Methods: A retrospective case \? series study was conducted on 186 cases of ovarian masses, reported from august 2013 to July 2014.
Results: Mean age of the subjects was 35.6 years, ranging from 4 to 80 years. In a total of 186 cases of ovarian masses, 104(55.91%) were non-neoplastic and 82 (44.09%) were neoplastic. Among neoplastic lesions, 80.48% (66/82) were benign and 19.52% (16/82) were malignant. The commonest non-neoplastic lesion was Luteal cyst (43/104) followed by simple serous cyst (25/104). The commonest benign tumor was serous cystadenoma(40/66) followed by dermoid cyst(12/66). The commonest malignant tumour was serous cystadenocarcinoma (5/16) followed by mucinous cystadenocarcinomama (3/16).
Conclusion: Non-Neoplastic lesions were more common than neoplastic lesions, while benign tumours outnumbered the malignant ones. The commonest benign tumour was serous cystadenoma and malignant was serous cystadenocarcinoma. The commonest non-neoplastic lesion was Luteal cyst. Among histological types of ovarian tumours, surface epithelial tumours dominated the other types.
Keywords: Ovarian tumours, Luteal cyst, Serous cyst, Dermoid cyst, Cystadenocarcinoma
Full Text:
INTRODUCTION The incidence of cancer is increasing in developing countries.1,2 There are marked differences in distribution of different cancers in different regions of the world.2,3 Ovarian cancer is the most frequent cause of death from gynaecological cancers and the fourth most frequent cause of death from cancer in women in Europe, United States4 and Eastern India.5 Exact incidence in India is not known, but ovarian cancer is the 4th most common cancer among females of India and continues to present at an advanced age.6 The lifetime risk of ovarian cancer in women with no family history is 1.6%; with one affected first degree relative is 5%,7 and 7% with two or more affected first degree relatives.8 Ovarian tumours are insidious in onset and usually diagnosed at a late stage. They are rare in young age group.9 They commonly present with abdominal pain, a lump or menstrual irregularities.10 In addition to biopsy, various diagnostic modalities include transvaginal ultrasonography, MRI, positron emission tomography,11 and markers like serum CA 125.8 Diverse histopathologies are common in ovarian lesions. Relative frequency of different ovarian tumours is different for western world and Asian countries.
For example surface epithelial tumors account for 50.0 – 55.0% of all ovarian tumors and their malignant counterpart for approximately 90.0% of all ovarian cancers in Western world whereas this figure is 46.0 – 50.0% and 70.0 – 75.0% respectively in Japan. Similarly mucinous tumors account for 12.0 – 15.0% of all ovarian tumors in Western world. This figure is 20.0 – 23.0% for Japan. Germ cell tumors account for 30.0% of primary ovarian tumors and malignant germ cell tumors account for 3.0% of all ovarian cancers in Western world.12 Determination of these patterns is important for diagnosis, management and prognosis. This study was conducted to find out the histopathological patterns of ovarian lesions in patients attending a civil hospital, Ahmedabad.
MATERIALS AND METHODS A retrospective case – series study was carried out on 186 patients who had undergone surgical oophorectomy. Samples were analysed in the Pathology department of B.J.M.C., Civil Hospital, Ahmedabad. All Histopathological diagnosed cases of ovarian lesions referred to this department during August 2013 to July 2014 were included in this study. These were mostly referred from gynaecology and obstetrics department of our civil Hospital, Ahmedabad, but a few were referred from other hospitals in the vicinity. The data was retrieved from the record files of pathology department. Patients with abdominal– pelvic masses other than of ovarian tumours diagnosed on histopathology were excluded from the study. The histological characterisation of ovarian tumour was done according to the International Classification of Diseases, 9th ed. (ICD9) (WHO Classification, 1995).13 The acquired data was analysed using the descriptive statistics.
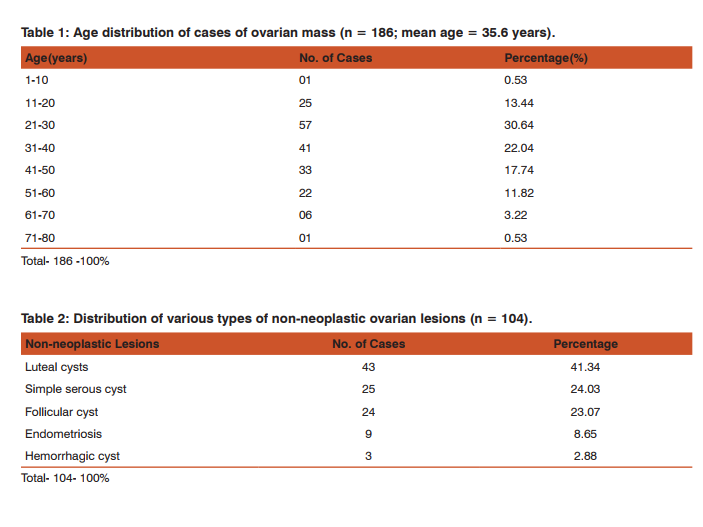
RESULTS During the study period from august 2013 to July 2014, one hundred and eighty six consecutive cases of ovarian lesions were selected. Ages of the patients and their histopathology diagnoses were recorded. Patients were divided into eight age groups, with a difference of 10 years in each group. The commonest age group affected was from 21 to 30 years followed by age group from 31 to 40 years. The youngest patient was 4 years old and the oldest was 80 years old. Mean age was 35.6 years (Table 1). In a total of 186 ovarian lesions, 104 (55.91%) were non-neoplastic and 82 (44.09%) were neoplastic. The neoplastic lesions comprised 66/82 (80.48%) benign and 16/82 (19.52%) malignant tumours (Fig. 1).
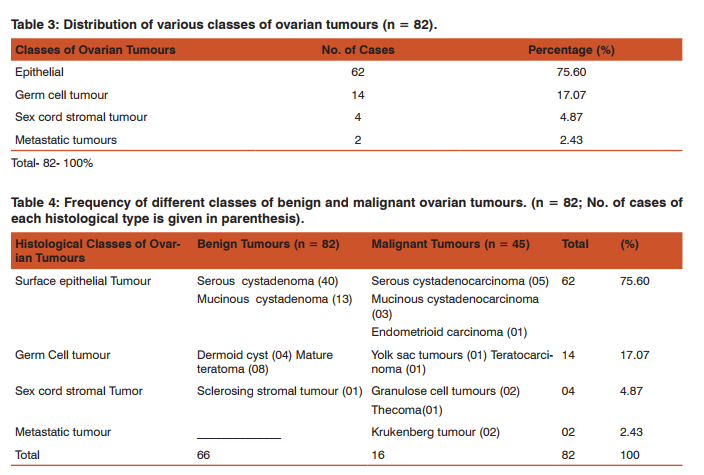
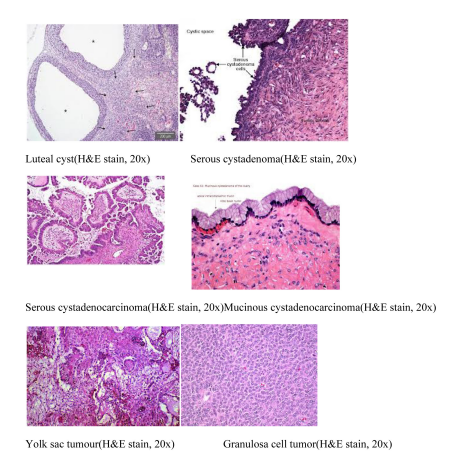
In non-neoplastic lesions, Luteal cyst was the predominant category (43/104) followed by simple serous cyst (25/104) (Table 2). The neoplastic tumours were divided in four groups, namely, epithelial tumours, germ cell tumours, sex cord stromal tumours and metastatic tumours. Epithelial tumours were maximum in number(62/ 82; 75.60%), followed by Germ cell tumours (14/82; 17.07%) (Table 3). Frequency pattern of different classes and subtypes of benign and malignant ovarian neoplasms (n = 82) is show in table 4. The commonest histological class is surface epithelial tumours (62/82; 75.60%) followed by germ cell tumours (14/82; 17.07%). Among all the benign lesions (n = 82), serous cyst adenoma is the commonest (40/82), while dermoid cyst is at the second number (14/82).
Frequency pattern of different classes and subtypes of benign and malignant ovarian neoplasms (n = 82) is show in table 4. The commonest histological class is surface epithelial tumours (62/82; 75.60%) followed by germ cell tumours (14/82; 17.07%). Among all the benign lesions (n = 82), serous cyst adenoma is the commonest (40/82), while dermoid cyst is at the second number (14/82). On the other hand, among all the malignant lesions (n = 16), serous cyst adenocarcinoma is at the top (05/45), followed with a little difference by mucinous cyst adenocarcinoma (03/45) and endometrioid carcinoma (01/45) respectively.
DISCUSSION Age range of our subjects was from 4 to 80 years and mean age was 35.6 years. Mean age observed in our study is lower than that observed in few other studies carried out in india. Our study shows the maximum incidence of ovarian masses between 21 and 40 years of age. This differs from the western data where it is between 50 and 70 years16 but correlates with other studies conducted in India. In our study non-neoplastic lesions were 55.91% (104/186) and neoplastic lesions were 44.09% (82/186). Neoplastic lesions contained (66/82) benign and (16/82) malignant. Tanwani19 documented 31.4% non-neoplastic lesions, 46.4% benign tumours and 22.2% malignant tumours. Among non-neoplastic lesion, Luteal cyst was most common (43/104) followed by simple serous cysts (25/104) in our study.
The pattern of distribution of non-neoplastic lesions is quite variable in other studies. Among the 82 neoplastic lesions in our study, 80.48%were benign and 19.82% were malignant. The higher incidence of benign tumours is also documented in various other studies,19,21,22 where it is 85%, 78%, 89.7% and 72.73% respectively and ratio of benign to malignant tumours is lower in these studies as compared to our study. No borderline tumor was found in our study. Among the major histological classes, the commonest type of ovarian neoplasm seen in our study was surface epithelial tumours, whether benign or malignant (62/82; 75.60%). Our finding is closer to the observations made in several other studies i.e. 64%, 66% and 70%7,24,25 respectively. However, Guppey et al26 documented a higher incidence of epithelial tumours than in our study i.e. 90%.
Germ cell tumours (GCT) in our study were 17.07%. This value is quite high as compared to Western data (370)4 and data collected from other parts of india (1470)16 and (27.13%).7 This difference may be due to variations in sample size but genetic, socioeconomical and environmental factors may also be involved. The frequency of sex – cord – stromal tumours (SCST) in our study was 4.87%. This value is comparable with that of studies carried out in the west (5%)27 and other parts of india (370).16 Our study showed that serous tumours (whether benign or malignant) were more common than mucinous tumours (40/67 vs 16/67 cases). This finding correlates with other studies.28,29 The studies carried out by Khanum and Rehman22 and Aziz et al17 also observed serous cyst-adenomas to be the commonest tumours.
The frequency of malignant tumours in our study was highest for serous cyst adenocarcinoma (5/16) followed by mucinous cyst adenocarcinoma (03/ 16). Similar pattern of distribution of malignant tumors are shown by many other studies.7,20 However, Study conducted by Yasmeen et al shows endometrioid carcinoma to be more prevalent.21 Germ cell tumours (GCTs) comprise the second largest group in our study in which benign tumours dominated the malignant ones (12/14 vs. 02/14 ). Among the benign GCTs our study showed the highest incidence of mature teratomas followed by dermoid cysts (08/14and 04/14 respectively). A study of Thanikasalanm et al 30 conducted in India shows teratomas to be the predominant GCT, whereas study conducted by Ahmad et al 7 in Pakistan documents dermoid cysts to be the commonest GCT.
Sex cord stromal tumours (SCSTs) were the least common in our study, next to metastatic tumours (4/82; 4.87%). The incidence of these tumours is variable in other studies. Zohra18 found only 1% SCSTs while Tanwani19 documents 10.1% cases of SCST. Granulosa cell tumours were the commonest SCSTs in our study (2/4) while studies carried out by Yasmeen et al21 and Ahmad et al31 mentioned a variable incidence of 28.5% and 5.62% respectively. In conclusion according to this study ovarian tumours are common in age group of 21 to 40 years. Neoplastic lesions are more common than non-neoplastic lesions. Luteal cyst is the commonest nonneoplastic lesion.
Among the histological classes of neoplastic lesions, surface epithelial tumours are predominant type, followed by germ cell tumors. The commonest benign tumour is serous cystadenoma and commonest malignant tumour is serous cystadenocarcinoma. This study is institutional – based, therefore the results obtained may or may not reflect the actual histological pattern of ovarian tumours in indian women. Therefore, multicentric study with larger sample size should be carried out.
CONCLUSION Non-Neoplastic lesions were more common than neoplastic lesions, while benign tumours outnumbered the malignant ones. The commonest benign tumour was serous cystadenoma and malignant was serous cystadenocarcinoma. The commonest non-neoplastic lesion was Luteal cyst. Among histological types of ovarian tumours, surface epithelial tumours dominated the other types.
ACKNOWLEDGEMENTS Acknowledgements are due for my colleagues and the paramedical staff of the department of pathology, B.J.M.C., Civil Hospital, Ahmedabad for their cooperation and continuous moral support. Thanks are also due for the staff of Gynec and Obstetric department of our hospital and all others who sent the biopsy specimens of ovarian masses to our department.
References:
1. Parkin DM, Muir CS, Whelan SL et al. eds. Cancer incidence in five countries. Lyon: IARC, 1997; 8: 1028-9.
2. Pisani P. Burden of cancer in developing countries. IARC Scientific Pub 1994; 129: 31-9.
3. Parkin DM, Pisani P, Farlay J. Estimates of worldwide incidence of 18 major cancers in 1985. Int J Cancer 1993; 54: 594-6.
4. Jacob IJ, Menon U. Progress and challenges in screening for early detection of ovarian cancer. Mol Cell Proteomics, 2004; 3: 355-66.
5. Sen U, Sankaranarayanan R, Mandal S, Romana AV, Parkin DM, Siddique M. Cancer pattern in eastern India: the first report of Kolkata cancer registry. Int J Cancer 2002; 100: 86-91.
6. Parveen S, Ilyas N, Asghar S. Patterns of care for ovarian cancer: patients at institute of Nuclear Medicine and Oncology (INMOL) india.
7. Ahmad Z, Kayani N, Hasan SH, Muzaffar S, Gill MS. Histopathological pattern of ovarian neoplasm. J Pak Med Assoc, 2000; 50: 416-9.
8. Kauff ND, Satagogan JM, Robson ME, Offit K. Risk reducing salpingo-oophorectomy in women with a BRCA1 or BRCA 2 mutation. N Engl J Med, 2002; 346: 1609-15.
9. Saadia Tariq, Rubina Sohail. Study of ovarian tumors in young girls. Professional Med J. 2011; 18 (1): 41-5.
10. Shahin R, Ghulam S, Abid A. A clinic – pathological study of ovarian cancer. Mother and Child 1998; 36: 117-25.
11. Rieber A, Nussle K. Preoperative diagnosis of ovarian tumors with MR imaging, comparison with transvaginal sonography, positron emission tomography and histological findings. AJR Am J Roentgenol 2001; 177: 123-9.
12. Tavassoli FA, Devilee P. WHO. Classification of Tumors. Pathology and Genetics. Tumors of breast and Female Genital Organs. IARC Press: Lyon 2003.
13. WHO Histologic Classification of Ovarian Tumors, Geneva, WHO, 1995.
14. Shahbaz Sarwar CM, Neelam Siddiqui, Rizwan Anwar Khokhar, Farhana Badar. Epithelial ovarian cancer at a cancer hospital in a developing country. Asian Pacific J Cancer Prevention, 2006; 7: 595-598.
15. Aria M, Utsunomiya, Miki Y. Familial breast and ovarian cancers. Int J Clin Oncol, 2004; 9: 270-82.
16. Mariam Malik, Farooq Aziz. Malignant ovarian tumors: a study of 75 patients. Pak J Obstetric Gynaecology May 1999; 12 (1,2): 83-6.
17. Aziz F., Mariam Malik, Nosheen Yousaf. The pattern of ovarian malignancies – a retrospective study over a period of three years. A retrospective study over a period of three years. Ann King Edward Coll Oct – Dec 1999; 5 (3,4): 276-8.
18. Zahra F. The pattern of ovarian masses. Ann King Edward med Coll Oct – Dec 2006; 12 (4): 480-2.
19. Tanwani A.K. Prevalence and pattern of ovarian lesions. Ann Pak Inst Med Sci Oct – Dec 2005; 1 (4): 211-4.
21. Yasmin S, Aiman yasmin, Mohammad Asif. Frequency of benign and malignant ovarian tumors in a tertiary care hospital. J postgrad Med Inst Oct – Dec 2006;20 (4): 393-7.
22. Khanum Z, Amanur Rehman. The prevalence and age distribution of ovarian cysts. Ann King Edward Med Coll Oct – Dec 2005; 11 (4): 392-3.
23. Naseem Junejo, Sheikh F, Mumtaz F. Clinical presentation and treatment outcome of ovarian tumors at gynaecology ward. J Liaquat Uni Med Health Sci. Jan – Apr 2010; 9 (1): 30-2.
24. Gatphol ED, Darnal HK. Pattern of ovarian neoplasm in Manipur. J Indian Med Assoc, 1990; 88: 338-9.
25. Tyagi SP, Maheswari V, Tyagi N, et al. Solid tumors of the ovary. J Indian.med assoc, 1993; 91: 227-30.
26. Guppy AE, Nathan PD, Rust n GJ. Epithelial Ovarian Cancer: A review of current management. Clin oncology (R coll Radiology), 2005; 17: 399-411.
27. Morrison J. Advances in the understanding and treatment of ovarian cancer. J Br Menopause Soc, 2005; 11: 66-71.
28. Yasmin S, Yasmin A, Asif M. Clinicopathological pattern of ovarian tumours in Punjab region. J Ayub Med Coll Abbottabaad 2008; 20 (4): 11-13.
29. Prabarker, Maingi K. ovarian tumors – prevalence in Punjab. Indian J Pathology Microbiology 1989; 32: 276-81.
30. Thanikasalam K, Ho CM, Adeed N, Shahida MN, Azizah WK. Links Pattern of ovarian tumors among Malaysian women at General Hospital, Kuala Lumpur. Med J Malaysia 1992; 47: 139-46.
31. Ahmad M, Malik TM, Afzal S, Mubarik A. Clinicopathological study of 762 ovarian neoplasms at Army Medical College india. ind J Pathology 2004; 15 (4): 147-52.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License