IJCRR - 13(1), January, 2021
Pages: 141-145
Date of Publication: 05-Jan-2021
Print Article
Download XML Download PDF
Malignant Ovarian Tumours \? A Clinicopathological Study for a Period of Five Years in a Tertiary Care Hospital
Author: G. Sudhakar, T. Rayapa Reddy, P. Geetha Vani, C. Padmavathi Devi
Category: Healthcare
Abstract:Introduction: Ovarian malignancy represents 5th most common cause of cancer death in females and they account for 2nd leading cause of death from cancer of the female genital tract. Though they are treatable and sensitive to anticancer therapies, they are usually detected when they have spread beyond the ovary.
Objective: To know the overall incidence of malignant ovarian tumours among all ovarian tumours. To report the age incidence, presentation, gross and microscopic features of various histomorphological types of malignant ovarian tumours which help the clinician in the anticipation of malignancy before its spread beyond the ovary. Methods: This is a clinicopathological retrospective study where clinical details of all ovarian tumours which were diagnosed as malignant were obtained. The regressed bits were subjected to histopathology processing and staining.
Results: In our study, we noted overall malignancy was14.70% among all ovarian tumours. Most commonly seen in the age group of 51-60 years and most commonly presented with either lump or pain in the abdomen. Grossly they are solid and 95.5 % are primary in origin. Among the primary ovarian malignant tumours, 69% were surface epithelial tumours.
Conclusion: The solid component in an ovarian tumour may represent the malignant nature of tumour with the increasing age of women. Surface epithelial malignancy was more common in the old age and germ cell tumours were seen in the younger group. Preoperative diagnosis of malignant tumours can be done by radiological, serological and clinicopathological findings which help in the reduction of mortality.
Keywords: Clinical nature, Histopathology, Malignant tumours, Ovary
Full Text:
Introduction
In recent times it has been observed that there is an increased incidence of cancers among women and ovarian cancer is one of the major contributors. Ovarian malignancy carries the highest fatality rate among all gynaecological cancer. The overall survival rate is less than 50%1-4. There is no screening test to detect in the early stage and also the cancer is not very symptomatic.3,4 The Ovarian tumours are complex and involving a variety of histological diagnosis ranging from epithelial tissues, connective tissues, specialized hormone-secreting to germinal and embryonal cells.5,6 Most of the ovarian tumours are benign and cystic. Majority of ovarian cancers are a solid or solid component in cystic tumours. Any solid ovarian tumours in older women first to rule out malignant nature of the tumour.5-8 A combined approach of radiological, clinical and cytopathological studies can help in early diagnosis of disease. So that with recently developed treatment modalities survival rate of the patient can be increased. Main risk factors for malignant ovarian tumours are increasing age, positive family history, increase the age of reproduction, and null parity.7,8 A clinicopathological study of malignant ovarian tumours is very helped full in understanding their nature, presentation, and behaviour in women of various ages.
MaterialS and Methods
A clinicopathological retrospective study to understand nature, behaviour and histology of malignant ovarian tumours were done at GGH and department of pathology, Guntur medical college, Guntur from January 2015 to December 2019 i.e. for five years. All ovarian tumours which were diagnosed as malignant were included. Benign and borderline ovarian tumours were excluded from our study. Among malignant tumours, inadequate samples were also not considered. Clinical details were obtained from previous data stored in the government general hospital and gross examination of specimens, the histopathological study of slides was done at the pathology department, Guntur Medical College. After a thorough study and gross examination, tissue sections were given where ever necessary. The regressed bits were subjected to histopathology processing and staining. In some cases where ever necessary special stains were done.
Results
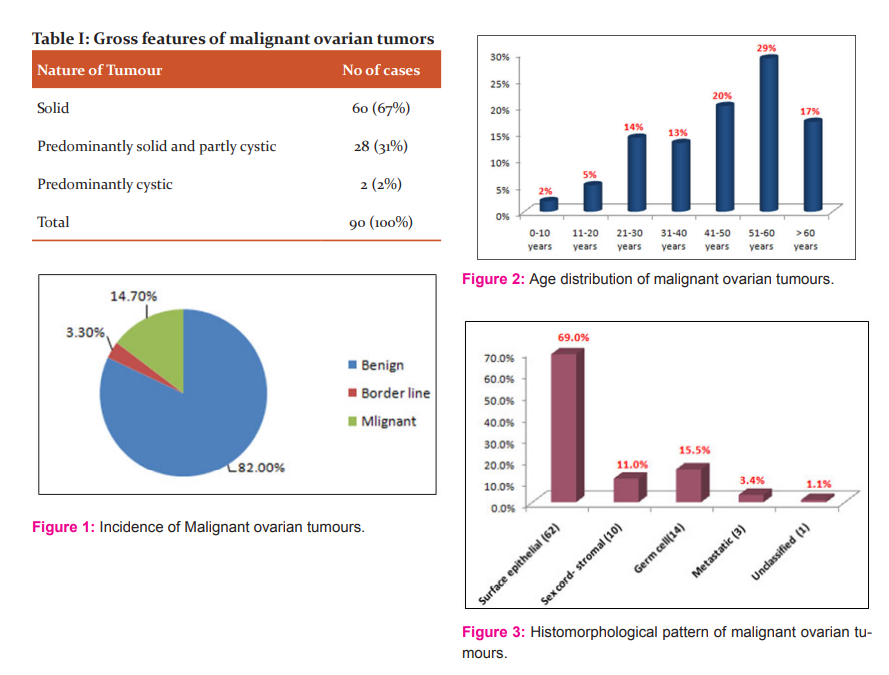
A total number of 610 ovarian tumours were received during the period between January 2015 to December 2019 out of which 500 were benign, 20 were borderline and 90 were malignant tumours. The overall incidence of malignant ovarian tumours was 14.70% among all ovarian tumours (Figure 1). Maximum incidence was seen in the age group of 51-60 with 26(29%) cases and followed by 41-50 with 18 (20%) cases of malignant ovarian tumours (Figure 2), Surface epithelial malignancy was more common in the old age and germ cell tumours were seen in the younger group.
Most cases were presented with a lump in the abdomen or pain in the abdomen to the gynaecological department. In the majority of cases, investigations revealed serum elevation of tumour markers like beta HCG, AFP, and CA-125. Radiologically most of the cases revealed solid or predominantly solid ovarian masses.
Macroscopically malignant ovarian tumours are predominantly solid, some are partly solid and partly cystic. Of 90 Malignant ovarian tumours, 60( 67%) were solid and 28(31%) were predominantly solid and partly cystic. 2% were predominantly cystic (Table I). Size of the tumour varies can be range from huge mass to small lesion. Majority of cases were unilateral and metastatic tumours were bilateral.
Histologically the primary ovarian tumours were 95.5 % (86 cases) of cases, secondary or metastatic tumours were 3.4 %( 3cases) and undiagnosed with routine H&E and immune stains was1.1 %( 1 case) which was grouped under unclassified category (Figure 3). .In this study among primary tumours, the maximum number of cases were surface epithelial tumours, followed by germ cell tumours and sex cord-stromal tumours. Surface epithelial tumours account for the highest number 62(69%) among all malignant ovarian tumours and serous cystadenocarcinoma (Figure 4,5) was the most common histological type among surface epithelial cancers followed by mucinous cystadenocarcinoma (Figure 4,5) and transitional carcinoma.
Malignant germ cell tumours constitute about 15.5 %( 14 cases) of all ovarian cancers. Out of fourteen cases of germ cell tumours, seven were dysgerminoma (Figure 4,5), two were yolk sac tumours, two cases were immature malignant teratoma of which one was initially thought mature teratoma with gliomatosis person, later after extensive sampling we found immature elements in the tumour (Figure 4,5), two embryonal cell carcinoma and one case was of mixed germ cell tumour.
Among ten (11%) sex cord-stromal tumours majority (9) were adult granulose cell tumours and one was Sertoli cell tumour. Two Kruken berg tumours (Figure 4,5), one was Mets from squamous cell carcinoma of cervix accounts for three metastatic tumours in our study. One tumour was grouped as unclassified as histological picture suggestive of small carcinoma/Lymphoma of the ovary but immunological results were also not conclusive.
Discussion
Among all ovarian tumours we have noted 14.70% of malignant ovarian tumours which was nearer to Kancherla et al. who has reported 18% in their study.9 But Reta Devi et al. in their study mentioned 5.1% which was very low and Urmila singh et al. reported very high incidence malignant ovarian tumours which was 41.9%.10,12
Malignant ovarian tumours exhibit a wide spectrum of clinical, morphological, and histological features and are the cause of considerable mortality in all age group women. They occur at any age, seen in children, adolescence, and old age. In our study, the most common age group for malignant ovarian tumours was 51–60 years with 29% (26 cases) followed by age group 41–50 years with 20% (18) cases. A maximum number of malignant ovarian tumours was seen between age 41to 60 years accounts for 49 % (44) cases. The oldest women with ovarian cancer in our study were 82 years old and the youngest was a 6 years old female child. Like our study, most of the other studies found 41-60 years was the most common age group with malignant ovarian tumours. Chandanwale et al. in their study stated that the most common age group for malignant ovarian tumours was 51–60 (26%) years followed by 21–30 (22%) and the youngest case was an 8 years old female child.12
In our study, we found 34% (31 cases) of malignant ovarian tumours before age 40 years with a maximum incidence between 21-40 years and the common histological group is germ cell tumours and the type is dysgerminoma. Some studies mentioned the rarity of malignant ovarian tumours rarely before the age of 40 years. Chandanwale et al. also found the significant number of ovarian malignancies before age 40 years.12 Okugawa et al. found that mean age of malignant tumour was 51.9 year.13 Chandanwale et al. study mentioned 45.4 years was the mean age.12 In our study, it was 50.2 which were near to Okugawa et al.13 Most common clinical symptom in our study was Pain and lump in the abdomen. Similar observations were made by Chandanwale et al., Bhuvanesh et al. and Kanthikar et al.12,14,15
In our study, the majority of malignant tumours were unilateral (95%) and most of the bilateral cases were metastatic tumours. Our findings are similar to the findings of Kancherla et al., Reta Devi et al. and Chandanwale SS et al. and others.9.10,12 We did not find any markedly increased incidence in the right or left side of the ovary.
In our study, we found huge mass to the small lesion of malignant ovarian tumours. Majority of the tumours 67% (60 cases) were solid and 31% (28) were predominantly solid and partly cystic. Okugawa K et al. were found similar observations.13 Chandanwale SS et al. in their study found maximum (44%) malignant tumors were solid/cystic in nature.12 In our study most of the malignant ovarian tumours are primary in origin and accounts for 95.5% among all tumours. Among primary malignant ovarian tumours surface epithelial tumours were the highest in number 62 (69%) and serous cystadenocarcinoma was the most common histological type among surface epithelial cancers followed by mucinous cystadenocarcinoma and transitional carcinoma. Chandanwale et al., Kar et al. and Gilani et al. were made similar findings in their studies.12,16,17
Malignant germ cell tumours constitute about 15.5% (14 cases) of all ovarian cancers in our study. Chandanwale et al., Kar et al., Gilani et al. has made the incidence of malignant germ cell tumours as 18%,19.23%,17.1% respectively, which were near to findings of present study.12,16,17 Mankar et al. noted 10% of malignant gem cell tumours contrary to our study.18 Among the various histological types, we noted seven cases of dysgerminoma, two cases of yolk sac tumors, and two were immature malignant teratoma, two embryonal cell carcinoma and one case of mixed germ cell tumour. Dysgerminoma was the most common malignant germ cell tumour found in our study and similar finding was made by Kar et al. and Lalrinpuii et al.16,19. But Chandanwale et al. in their study found immature teratoma was the most common tumour12. We have noted one case of immature teratoma with gliomatosis peritonei, Wang et al. has described two cases of gliomatosis peritonei in their study.20
Malignant sex cord-stromal tumours constitute about 11% (10 cases) of total tumours. The majority (9) were adult granulose cell tumours and one was Sertoli cell tumour. Chandanwale et al. in their study found 14% (7) sex cord-stromal tumours with the majority of adult granulosa cell tumours.12. But Kar K et al. recorded low incidence of sex cord-stromal tumours 3.84% and Garg R et al. noted not even a single case in their study.16,21
In our study metastatic tumours account for 3.4% and 1.1% were grouped under unclassified. Our findings show less incidence of metastatic tumours than Chandanwale et al., Kar et al., Gilani et al. who has shown the incidence of 6%,7.69% and 6.6% respectively.12,16,17 Mankar et al., Jha et al. noted a high incidence of metastatic tumours 20% and 15.38%, respectively contrary to other studies.18,22
Conclusion
Surface epithelial malignant tumours are the most common among all malignant ovarian tumours. Their incidence is highest between 41-60 years. Germ cell malignant tumours are more common in younger age group females. Though their incidence is less, sex cord-stromal tumours were relatively seen in all age groups. Metastatic ovarian tumours were more common in older women and increases with increasing age. Macroscopically most of the malignant ovarian tumours are solid or predominantly solid. Due to the high fatality rate and worst prognosis of malignant ovarian tumours, it is very important to diagnose ovarian malignancy very early in the disease process. Most of the cases have extensive spread by the time of diagnosis and is the cause of increased death rate in ovarian cancers. For early diagnosis, a combined radiological, pathological and clinical approach with high vigilance is needed if a female patient came to the hospital with distension or pain abdomen. So that survival rate can be increased in patients suffering from ovarian malignancies.
ACKNOWLEDGEMENTS:
The authors are thankful to authors, editors, publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed
Conflict of interest: Nil
Source of Funding: Nil

References:
1. Hirschowitz L. What is ovarian carcinoma? Southwest Cancer Intell Serv J 2000;8:10-5.
2 Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T. Cancer statistics, 2008. CA Cancer J Clin 2008;58:71-96.
3. Maheshwari A, Kumar N, Mahantshetty U. Gynecological cancers: A summary of published Indian data. South Asian J Cancer 2016;5:112-20.
4. Murthy NS, Shalini S, Suman G, Pruthvish S, Mathew A. Changing trends in the incidence of ovarian cancer – The Indian scenario. Asian Pac J Cancer Prev 2009;10:1025-30.
5. Prate J. Pathology of Ovarian Cancer. Barcelona: J Autonomous Uni Barcelona Dept Pathol 2000; 231.
6. Shraddha SO, Sridevi TA, Renukadein TK, Gowri R, Binayah D, Indra V. Ovarian masses: Changing histopathological trends. J Obstet Gynaecol Ind 2015;65:1:34–38.
7. Umakanthan S, Chattu VK, Kalloo S. Global epidemiology, risk factors, and histological types of ovarian cancers in Trinidad. J Family Med Prim Care 2019;8:1058-64.
8. Singh U, Solanki V, Prakash B, et al. Clinicopathological Spectrum of Ovarian Tumours in Northern India: Changing Trends Over 10 Years. Indian J Gynecol Oncolog 2020; 18(59): 210-14.
9. Kancherla J, Kalahasti R, Sekhar KPAC, Yarlagadda SB, Devi SP. Histomorphological Study of Ovarian Tumors: An Institutional Experience of 2 Years. Int J Sci Stud 2017;5(3):232-235.
10. Reeta Devi M, Keerthivasan V, Tikhak J. Histomorphological spectrum of ovarian tumours, 4 years experience in a regional institute. J Evid Based Med Health 2020; 7(4):173-176.
11. Singh U, Solanki V, Prakash B, Mehrotra S, Verma ML. Clinicopathological Spectrum of Ovarian Tumours in Northern India: Changing Trends Over 10 Years. Indian J Gynecol Oncol 2020;18(2):59.
12. Chandanwale SS, Jadhav R, Rao R, Naragude P, Bhamnikar S, Ansari JN. A clinicopathologic study of malignant ovarian tumours: A study of fifty cases. Med J DY Patil Uni 2017;10:430-7.
13. Okugawa K, Hirakawa T, Fukushima K, Kamura T, Amada S, Nakano H. Relationship between age, histological type, and size of ovarian tumours. Int J Gynaecol Obstet 2001;74:45-50.
14. Bhuvanesh U, Logambal A. Study of ovarian tumours. J Obstet Gynaecol 1978;28:271-7.
15. Kanthikar SN, Dravid NV, Deore PN, Nikumbh DB, Suryawanshi KH. Clinico-histopathological analysis of neoplastic and non-neoplastic lesions of the ovary: A 3-year prospective study in Dhule, North Maharashtra, India. J Clin Diagn Res 2014;8:4-7.
16. Kar K, Kar A, Mohapatra PC. Intra-operative cytology of ovarian tumours. J Obstet Gynecol 2005;55:345-9.
17. Gilani MM, Behnamfar F, Zamani F, Zamani N. Frequency of different types of ovarian cancer in Vali-e-Asr Hospital (Tehran University of Medical Sciences) 2001-2003. Pak J Biol Sci 2007;10:3026-8.
18. Mankar DV, Jain GK. Histopathological profile of ovarian tumours: A twelve-year institutional experience. Muller J Med Sci Res 2015;6:107-11.
19. Lalrinpuii E, Bhageerathy PS, Sebastian A, Jeyaseelan L, VinothaThomas, Thomas A, Chandy R, Peedicayil A. Ovarian Cancer in Young Women. Indian J Surg Oncol 2017 Dec;8(4) 540-547.
20. Wang J, Xu J, Zhang M, Li B. Gliomatosis peritonei with bilateral ovarian teratomas: A report of two cases. Oncol Lett 2016;12(3):2078–2080.
21. Garg R, Singh S, Rani R, Agrawal M, Rajvanshi R. A clinicopathological study of malignant ovarian tumours in India. J South Asian Fed Menopause Soc 2014;2:9-11.
22. Jha R, Karki S. Histological pattern of ovarian tumours and their age distribution. Nepal Med Coll J 2008;10:81-5.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License