IJCRR - 13(1), January, 2021
Pages: 125-130
Date of Publication: 05-Jan-2021
Print Article
Download XML Download PDF
Compare Constraint-Induced Movement Therapy and Bobath to improve Hand functions in Hemiplegic Patients
Author: Sugasri Suresh Kumar, K. Senthil Kumar
Category: Healthcare
Abstract:Introduction: With changes in techniques to treat hand functions in hemiplegic patients, both Constraint-Induced Movement Therapy (CIMT) where an unaffected hand is restrained from its use & Bobath where an unaffected hand is unrestrained are proved to be beneficial individually.
Objcetive: To compare both & to implement the better one for a speedy recovery.
Methods: Participants aged above 50, with Brainstorm stage of hand 2 and above were randomly divided into CIMT(n=10) and Bobath (n=10), the treatment being given for 30 min/day for the first 2 weeks, then 3 times/week for consecutive 10 weeks. Bobath includes Affected side weight-bearing, Bilateral Activity encouragement, Auto inhibition, Active wrist extension emphasizing MCP flexion, thumb abduction, Active finger extension by sweep tapping forearm dorsum, by withdrawing bottle brush from hand, transferring various shaped objects from sound to affected hand, Power grasps followed by prehension and repetition of tasks. CIMT includes the same as above but restraining the affected upper limb with a sling is worn 3 hours priorly avoiding bilateral activity. Fugl Meyer Assessment is used to measure hand functions, Functional Independence Measure (FIM) scale is used to measure ADL.
Results: Paired t-test showed an improvement, Independent t showed a difference in improvement between 2 groups. Percentage of difference between pretest (day1), posttest (day 60) showed increased improvement in hand functions and ADL in CIMT than Bobath.
Conclusion: Previous studies show CIMT & Bobath to be successful. The results of this study show CIMT is superior to Bobath in improving hand functions in Hemiplegics.
Keywords: CIMT, Bobath, Hand Functions, Fugl Meyer Assessment, MCP- Metacarpophalangeal joint, ADL-Activities of daily living
Full Text:
INTRODUCTION
In recent years frequency of Stroke which is found to be the leading cause of disability in Society has started to decline as more is known about the causative factors and by early detection. Hence certain measures of prophylaxis are possible. In the Rehabilitation point of view, therapists expect nearly 90-95% of the recovery in the lower limb, and in upper limbs especially the hands take a longer duration to recover.1-3 Hand functions that are very much essential during the patient's everyday activities need to be emphasized. Stroke is a disabling neurological condition resulting due to disruption of blood supply to the brain. It is classified according to pathology as Thrombotic, Embolic & Hemorrhagic.4,5 It is noted that 70% of strokes are due to ischemia, 20% due to haemorrhage and 10% have an unspecified origin. Post Stroke Functional recovery is prolonged than Motor recovery.3,6,7 Hands become discarded as useless tools, unlike lower extremity which has to be activated with every step the patient takes. It could be postulated that this is the reason why sensation in the leg tends to improve, while that in hand remains more impaired.8 Distributed CIMT is a promising intervention for improving motor function and quality of life in chronic stroke patients which involves training for 3 hours/ day for 20 days and restraint of another arm for 9 hours. This intervention provides the same amount of training as provided in conventional CIMT protocol (60 hours) but distributes training time over twice the no of days.9 From the above studies, CIMT that involves restraining unaffected hand during treatment, and Bobath which doesn’t involve restraining unaffected hand are found to be effective individually. Hence the purpose of the study is to measure and compare the functional changes when treated with both CIMT and Bobath concepts and to find which one is more effective to be applied in clinical practice for the speedy recovery of hand.10,11
MATERIALS AND METHODS
Twenty participants are recruited from Kovai Medical Centre Hospital, Coimbatore. Inclusion criteria being Age group above 50 years, Within 3 months from the onset of stroke, Involvement of middle cerebral artery, Independent in ADL before the stroke, Brunstorm stage of hand 2 (or) above. Exclusion criteria being Age group less than 50 years, Patients with subluxation of shoulder, Involvement of anterior cerebral artery, Dependent in ADL before the stroke, impaired cognition. The participants are randomly divided into 2 Experimental Groups. Group I consisting of 10 participants are treated with CIMT Technique. Group II consisting of 10 participants is treated with Bobath Technique. The techniques applied are as follows.
BOBATH
Normalization of tone
a) Weight bearing over affected side: sitting in a couch with the elbow extended, wrist extended and hand placed several inches away from hip.4
b) Auto inhibition: Sitting - keeping affected hand flat on the table, the position of the hand on the table is marked with chalk and allowing to do activities in unaffected hand like writing, painting, etc.,3
c) Placing in mixture of ice3
To improve extension of wrist
a) Positioning in bed: Lying on the affected side- the hand is placed below pillow.3
b) Grip used by therapist: Sitting in stool - Shoulder abducted, elbow extended, therapist holding fingers in extension with one hand and holding thumb with other hand assisting in the extension of wrist3. Sitting - forearm held by therapist, encouraging to do the extension of the wrist with an extended elbow, then with a flexed elbow.
c) Bilateral activity encouragement: Sitting with both hands clasped together placed on a table, pushing a ball or some other object.12,13
To improve extension of wrist with flexion of MCP and abduction of thumb
a). Supine with assistance from the therapist.
b). Standing near the edge of the table with the elbow extended (actively done)2,13
To improve finger extension
Sweep tapping on the dorsum of the forearm. Give a bottle brush to hold and then withdraw.
To improve sense of discrimination
Picking up objects with sound hand and transferring to the affected side (Various sized and shaped objects)
To encourage independence in ADL
a) Facilitation of slow controlled movements- When attempting with any task patient is encouraged to do slowly) (as quick movements increase the flexor synergy in hand).
b) Encouraging easy tasks to be performed like holding a tumbler, rod, ball, etc., which involves power grasp. Later, a task involving prehension activities are encouraged by the use of a spoon, coins, etc. (Repetition of the task is emphasized).
c) Dressing, brushing, eating, etc., is encouraged only by sitting in an upright chair. (Visual stimuli to make aware of the affected limb)14
CIMT
The unaffected limb is restrained from helping the affected limb for the reduction of "Learned nonuse". The sling used to restrain the unaffected limb is worn 3 hours before the treatment session.15
Normalization of tone:
By weight-bearing over the affected side
To improve extension of wrist
Positioning in bed, grip used by Therapist
To improve wrist extension with flexion of MCP and abduction of thumb: By assistance from the therapist & actively done
To improve wrist extension of fingers: Sweep tapping on the dorsum of the forearm, Give a bottle brush to hold, and then withdraw.
Encouraging independence in ADL: Only with the affected hand.16,17
DURATION OF TREATMENT
For the first 2 weeks, treatment is given for 30 minutes daily (1 session). For the consecutive 10 weeks treatment is given for 30 minutes, thrice in one week. (1 Session) - O.P basis.
EVALUATION TOOLS
1. FUGL MEYER Assessment- To determine improvement in functions.18,19 Mass flexion, Mass extension, Grasp A - Distal finger grasp
Grasp B - Thumb adduction grasp, Grasp C - Thumb to index finger grasp,
Grasp D - Cylindrical grasp, Grasp E - Spherical grasp.
SCORES: 0 - Cannot be performed, 1 - Detail partly performed, 2 - Detail performed faultlessly.
2) FIM SCALE - To Determine improvements in ADL20
SELF SCORE: Eating, Bathing, Dressing- upper and lower body Toileting TRANSFERS: Bed, Chair, Toilet, Tub / Shower
SCORES: 1- Total assistance, 2- Maximal assistance, 3- Moderate assistance,
4-Minimal assistance, 5- Supervision, 6- Modified independence, 7- Complete independence.
Pretest-Posttest Experimental Study Design is implemented. Pretest values and Posttest values are noted on Day1 and Day60 respectively by administering Fugl Meyer Assessment and FIM Scale.21,22
STATISTICAL ANALYSIS
The changes within both groups I &II for the variables Mass Flexion, Extension, Grasps & ADL were analyzed using an Independent –t-test at a 5% level of significance, the difference among the 2 groups for the same variables are analyzed using paired-test at 5% level of significance and Rate of progression between Day1 &60 are given by
X1 – X2 x 100 X2
Where X1 and X2 are pretest and posttest mean values respectively.
RESULTS
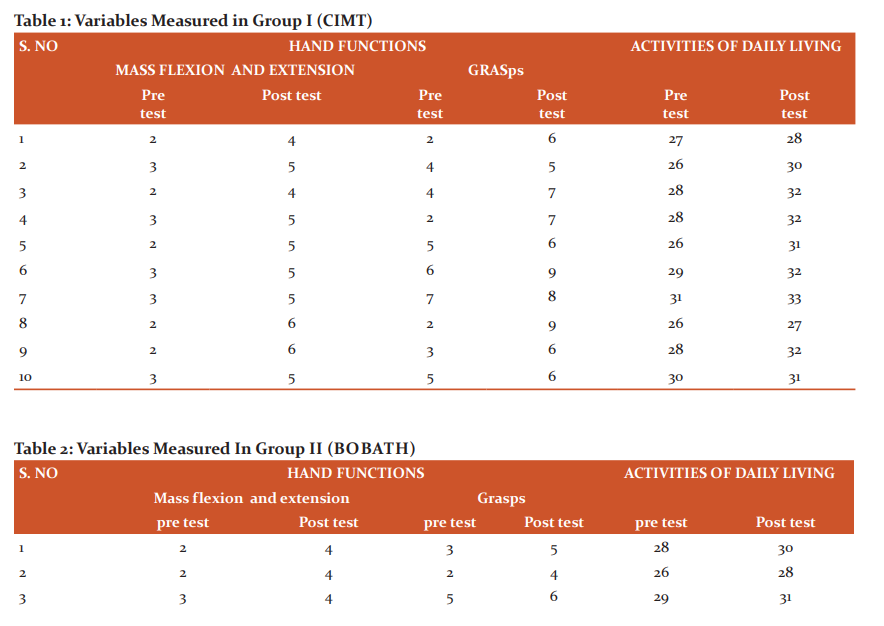
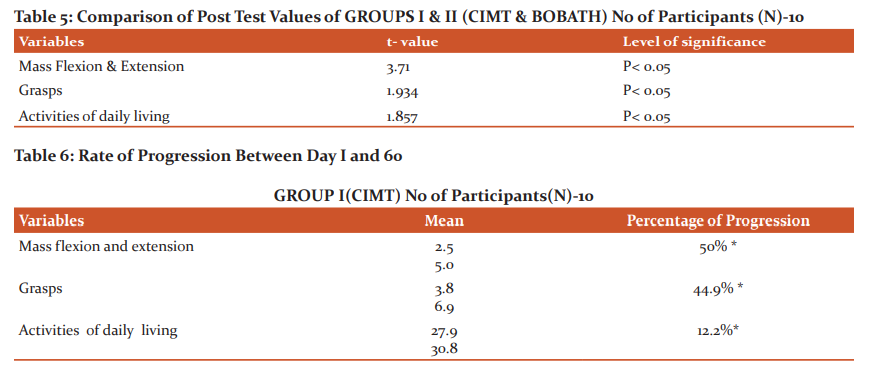
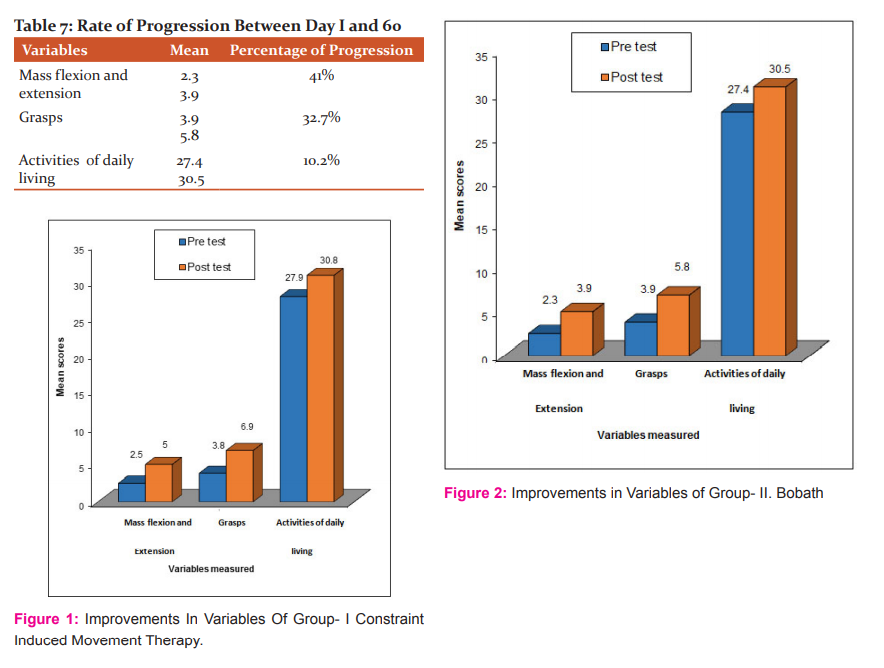
Pre-test & Post-test values of the variables Mass Flexion, Extension, Grasps & ADL measured in Group I is shown in Table 1 & the values of the same variables measured in Group II are shown in Table 2. Improvement in the variables is shown by Table 3 & is graphically depicted in Fig.1 for Group I, by Table 4 & is graphically depicted in Fig.2 for Group II. The significant difference between both the groups by Table 5. Group I ‘s progression is given in Table 6. These values are more when compared with Group II ‘s progression given by Table 7.
DISCUSSION
The results obtained show that there is a 9% increase in the rate of progression in mass flexion and extension, a 12.2% increase in grasps, and a 2% increase in activities of daily living in group I than in group II comparatively. Bobath is found to be useful since Affolter(1981) says that the only sensory modality that can activate directly in the tactile-kinesthetic system that builds up cognitive & emotional experiences.4,8,12 Improved sensory feedback creates a shift in the balance of intracortical networks towards that particular body part that is represented by relative enlargement of cortical sensory-motor representation which is the key concept in putting into use the affected limb as seen in CIMT.16-17
RECOMMENDATIONS
This study measures improvement in hand functions in terms of mass flexion, extension, and grasps, further studies measuring the improvement in individual ROM of finger joints can be done. Measuring specific subscales of FIM like Self score or transfers could be considered.
CONCLUSION
Improvements in ADL & hand functions are evident with both techniques by Statistical analysis and comparatively, CIMT is found to be more Superior to bobath which is shown by an increased percentage of progression. Hence it can be concluded that CIMT can be incorporated to treat hemiplegic patients & bring early recovery of hand functions & to reduce their disablement and handicap in the society.
ACKNOWLEDGEMENT:
The author acknowledges her project guide Mr. Senthil Kumar who has shared his energy, time, ideas & her Research Professor Mr.G.Venugopal for letting know the intricacies of Biostatistics.
CONFLICT OF INTEREST:
None.
FINANCIAL FUNDING:
None

References:
1. Asanuma C. Mapping movements within a moving motor map. Trends Neurosci 1991;14(6):217.
2. Bach-y-Rita P. Receptor plasticity and volume transmission in the brain: emerging concepts with relevance to neurologic rehabilitation. J Neurol Rehabil 1990;4(3):121-8.
3. Warlow CP. Epidemiology of stroke. Lancet 1998 Oct 1;352: S1-4.
4. Ryerson SD. Hemiplegia resulting from vascular insult or disease. Umphred DA (ed), Neurol Rehabil 1985;15:622-9.
5. Kakkad A, Rathod PV. Relationship & Comparison between Post-Stroke Motor Recovery and Functional Recovery–An Observational Study. Int J Cur Res Rev 2019; 11(01):6.
6. Black-Schaffer RM, Kirstein's AE, Harvey RL. Co-morbidities and complications. Arch Physical Rehabil 1999;80(5): S8-16.
7. Brock KA, Goldie PA, Greenwood KM. Evaluating the effectiveness of stroke rehabilitation: choosing a discriminative measure. Arch Phys Med Rehab 2002;83(1):92-9.
8. Taub E, Crago JE, Uswatte G. Constraint-induced movement therapy: A new approach to treatment in physical rehabilitation. Rehabil Psychol 1998;43(2):152.
9. Cai Y, Zhang CS, Ouyang W, Li J, Nong W, Zhang AL, Xue CC, Wen Z. Electroacupuncture for poststroke spasticity (EAPSS): protocol for a randomized controlled trial. BMJ Open 2018;8(2).
10. Dettmers C, Teske U, Hamzei F, Uswatte G, Taub E, Weiller C. Distributed form of constraint-induced movement therapy improves functional outcome and quality of life after stroke. Arch Phy Med Rehab 2005;86(2):204-9.
11. Dijkers MP, Yavuzer G. Short versions of the telephone motor Functional Independence Measure for use with persons with spinal cord injury. Arch Phy Med Rehab 1999;80(11):1477-84.
12. Meyer-Wahl R, Dettmers C. Outpatient rehabilitation—two years’ experience in the Neurological Rehabilitation Centre Hamburg. Neurol Rehabil 2002;8:128-37.
13. Goble DJ. The potential for utilizing inter-limb coupling in the rehabilitation of upper limb motor disability due to unilateral brain injury. Dis Rehab 2006;28(18):1103-8.
14. Hummelsheim H, Münch B, Bütefisch C, Neumann S. Influence of sustained stretch on late muscular responses to magnetic brain stimulation in patients with upper motor neuron lesions. Scandin J Rehabil Med 1994;26(1):3.
15. Taub E, Morris DM. Constraint-induced movement therapy to enhance recovery after stroke. Curr Ather Rep 2001;3(4):279-86.
16. Lister MJ. Contemporary management of motor control problems: proceedings of the II STEP conference. Found Physical; 1991.
17. Manning J. Facilitation of movement--the Bobath approach. Physiotherapy 1972;58(12):40.
18. Smith M. Neurological Rehabilitation: Optimising Motor Performance Physiother Can 2015 Spring; 67(2): 215–216.
19. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychological bull 1979 Mar;86(2):420.
20. Taub E, Miller NE, Novack TA, Cook EW, Fleming WC, Nepomuceno CS, et al. The technique to improve chronic motor deficit after stroke. Arch Phy Med Rehab 1993 Apr 1;74(4):347-54.
21. Winstein CJ, Miller JP, Blanton S, Taub E, Uswatte G, Morris D, et al. Methods for a multisite randomized trial to investigate the effect of constraint-induced movement therapy in improving upper extremity function among adults recovering from a cerebrovascular stroke. Neurorehabil Neur Repair 2003 Sep;17(3):137-52.
22. Wolf SL, Lecraw DE, Barton LA, Jann BB. Forced use of hemiplegic upper extremities to reverse the effect of learned nonuse among chronic stroke and head-injured patients. Expt Neur 1989;104(2):125-32.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License