IJCRR - 8(4), February, 2016
Pages: 25-28
Date of Publication: 21-Feb-2016
Print Article
Download XML Download PDF
REVIEW OF MESENCHYMAL HAMARTOMA OF CHEST WALL IN INFANCY- AN UNUSUAL TUMOUR
Author: Ravi G. Patel, Sanjay V. Dhotre, Hansa M. Goswami, Hitendra P. Barot, Manan P. Jadav
Category: Healthcare
Abstract:Mesenchymal hamartoma of the chest wall (MHCW) occurs as intraosseous expansile mass involving the ribs typically present at birth or in early infancy[1]. The incidence is about 0.03% among primary bone tumors with male predominance, and appropriately 100 cases have been reported. We present a case of 3-month-old female baby with slowly growing left sided chest wall swelling since birth. Computerized tomography (CT) revealed a Approx. 58x55x64mm3 sized expansile heterogeneous soft tissue density lesion (calcific, fluid and soft tissue) arising from posterior aspect of left fourth and fifth ribs with large intrathoracic component resulting in compression of left parenchyma. The lesion causes mass effect in form of widening of 4th and 5th intercostal spaces and shift of mediastinum towards left side. Rest of both lung fields appear normal. Thoracotomy with en bloc excision of the tumor was performed and tissue was sent for histopathological examination. Microscopy revealed structure of well circumscribed lesion chiefly consisting of fascicles of spindled shaped fibroblast admixed with cartilaginous and bony tissue with evidence of endochondral ossification. A final diagnosis of mesenchymal hamartoma of the chest wall was made. Oncologist deferred the chemotherapy The 80% of cases occur prenatally or within first 6 months of life and are usually solitary, but bilaterality or multicentricity also rarely occur[3,4]. Mesenchymal hamartoma is not a true neoplasm, but rather they are hamartomas with focal overgrowth of normal skeletal elements with no propensity for invasion or metastasis. Malignant transformation in MHCW is very rare[6]. The definitive diagnosis is established only by histopathological examination[5]. We hereby conclude that these tumors are very rare and they look aggressive both radiologically and microscopically, so it is essential to be aware of this condition, so that unnecessary over diagnosis and aggressive treatment with chemotherapy and radiotherapy can be avoided considering the fast recovery of the patient when managed with surgery alone.
Keywords: Mesenchymal hamartoma, Cartilagenous hamartoma
Full Text:
INTRODUCTION
Mesenchymal hamartoma of the chest wall (MHCW) occurs as intraosseous expansile mass involving the ribs typically present at birth or in early infancy[1]. The incidence is about 0.03% among primary bone tumors with male predominance, and appropriately 100 cases have been reported. The distinction between this benign tumor and malignant tumors like well differentiated chondrosarcoma is seldom clear cut[1]. The aggressive clinical presentation, radiological features, and histological features like actively proliferating fibroblastic and chondroid elements can be mistaken for malignant process [1].
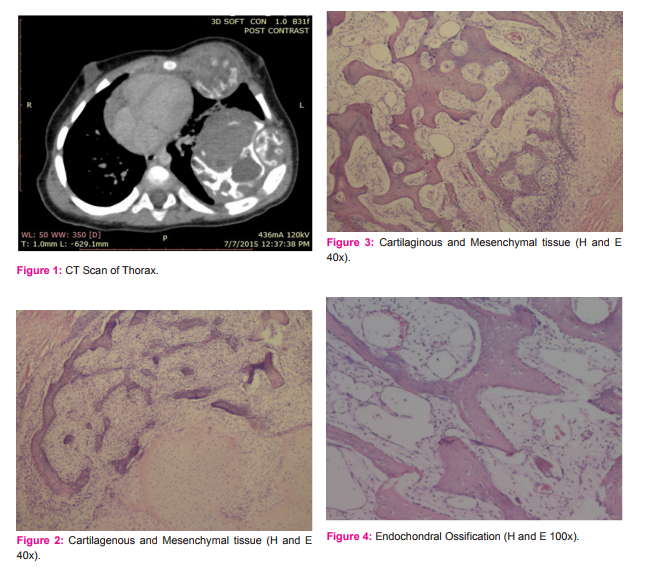
MATERIAL AND METHODS We present a case of 3-month-old female baby with slowly growing left sided chest wall swelling since birth. The patient was treated with thoracotomy and en bloc excision. A 3-month-old female baby presented with history of gradually progressive left sided chest wall swelling since birth with recent onset of breathlessness. Obstetric and developmental history was uneventful. On examination, baby had a firm, nontender, nonmobile, nonfluctuant swelling measuring 4x5 cm2 on the left chest wall. All hematological and biochemical parameters were within normal limits. Computerized tomography (CT) revealed a Approx. 58x55x64mm3 sized expansile heterogeneous soft tissue density lesion (calcific, fluid and soft tissue) arising from posterior aspect of left fourth and fifth ribs with large intrathoracic component resulting in compression of left parenchyma.
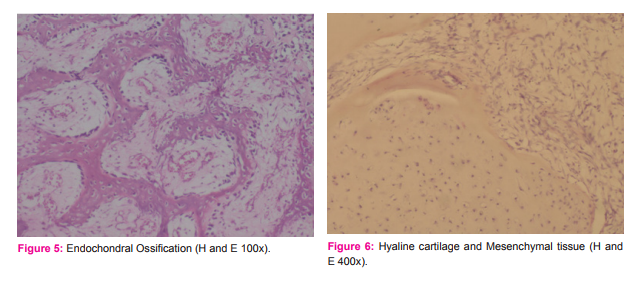
The lesion causes mass effect in form of widening of 4th and 5th intercostal spaces and shift of mediastinum towards left side. Rest of both lung fields appear normal. Thoracotomy with en bloc excision of the tumor was performed and tissue was sent for histopathological examination. On Gross examination, encapsulated greyish brown nodular hard tissue structure attached to ribs (3 ribs) noted measuring 7x6x5 cm3 with cut surface showing partly solid partly cystic, whitish areas (cartilage) with hemorrhagic areas. Microscopy revealed structure of well circumscribed lesion chiefly consisting of fascicles of spindled shaped fibroblast admixed with cartilaginous and bony tissue with evidence of endochondral ossification. A final diagnosis of mesenchymal hamartoma of the chest wall was made. Oncologist deferred the chemotherapy treatment. Diaphragm and pericardium were free from tumour.
DISCUSSION MHCW is a very rare benign tumor of bone which was first described by Nash and Stout in 1961[2]. McLeod and Dahlin coined the term hamartoma of the chest wall; however, many authors coined in different names like mesenchymal, vascular, cartilaginous, and chondromatous hamartoma, whereas the preferred term is mesenchymal hamartoma of the chest wall[2,3]. Almost 80% of cases usually occur in prenatal age or within first 6 months of life. Lesions are usually solitary, but bilaterality or multicentricity also occur in rare cases[3,4,7]. Typically, the lesion appears as a hard, immobile, subcutaneous, and extrapleural chest wall mass with deformed ribs. Respiratory distress and ventilator dependence may occur even in term or near-term newborns[2]. Mesenchymal hamartoma is not a true neoplasm, but rather they are hamartomas with focal overgrowth of normal skeletal elements with no propensity for invasion or metastasis[7]. Malignant transformation in MHCW is very rare[6].
Plain X-ray shows expansile mass with well-defined sclerotic margins with secondary aneurysmal bone cysts and popcorn-like speckled calcifications[2,3,5]. CT scan is a better modality which helps to determine the site of origin, tumor density, enlargement, and effect on adjacent structures[5]. Prenatal diagnosis is possible by ultrasonography, but most are diagnosed postnatally. Radiologically, MHCW can be confused with malignant tumors like congenital neuroblastoma, Ewing’s sarcoma, and malignant teratoma[5]. The definitive diagnosis is established only by histopathological examination[5]. Grossly, they are well circumscribed comprising both cystic and solid areas. Microscopically they have immature spindle shaped mesenchymal cells, osteoclastic giant cells, fragments of hyaline cartilage, areas of woven bone formation, areas of endochondral ossification and aneurysmal bone cyst-like changes[2].
Immunohistochemically, chondrocytes stain for S-100 protein and factor VIII highlighting the blood vessels. The differential diagnosis includes well-differentiated chondrosarcoma, aneurysmal bone cyst (ABC), chondroma, osteosarcoma, langerhans cell histiocytosis (LCH), and osteochondromas[2,3]. Chondrosarcomas occur at the periphery of the ribs and grow rapidly with presence of atypical mitosis, hence differentiated from MHCW. In the series of Ayala et al.,[5] one case of MHCW was misdiagnosed as chondrosarcoma[3]. Presence of cartilaginous tissue with mesenchymal cells ruled out the possibility of primary ABC. Tumors with such huge size, cystic change, and hypercellularity with presence of mesenchymal cells are usually not seen in chondromas.
Osteosarcoma, LCH, and osteochondromas can be ruled out by the absence of pleomorphic spindle cells with malignant osteoid, atypical histiocytes with longitudinal grooves in the background of eosinophils and osteocartilagenous cap with marrow tissue, respectively. Symptomatic patients have compromised cardiorespiratory function and it can cause deformity as well. They are best treated by complete resection and prognosis is very good[3].
However, MHCW stops growing within the first year of life and some patients may have an excellent outcome with conservative treatment alone[2,3]. Spontaneous regression has been observed in children even with bilateral involvement supporting the concept that conservative management is appropriate for asymptomatic children. Chemotherapy as well as radiation is not indicated in the treatment of MHCW. The most important postsurgical complication is scoliosis seen in 20% of patients[2].
CONCLUSION We hereby conclude that these tumors are very rare and they look aggressive both radiologically and microscopically, so it is essential to be aware of this condition, so that unnecessary over diagnosis and aggressive treatment with chemotherapy and radiotherapy can be avoided considering the fast recovery of the patient when managed with surgery alone. Abbreviations MHCW- Mesenchymal hamartoma of chest wall, ABC- aneurysmal bone cyst, LCH- Langerhans cell histiocytosis.
References:
1. Conlan AA, Hurwitz SS, Gritzman MC. Giant chondromatous hamartoma of the first rib. A case report. S Afr Med J 1982; 62:703-4.
2. Haase R, Merkel N, Milzsch M, Lieser U, Sauer H, Hinz L, et al. Mesenchymal chest wall hamartoma-surgery is preferred. Arch Perinat Med 2007; 13:56-61.
3. Amstalden EM, Carvalho RB, Pacheco EM, Oliveira-Filho A, Stragea- Neto L, Rosenberg AE. Chondromatous hamartoma of the chest wall: Description of 3 new cases and literature review. Int J SurgPathol 2006;14:119-26.
4. Ozolek JA, Carrau R, Barnes EL, Hunt JL. Nasal chondromesenchymal hamartoma in older children and adults: Series and immunohistochemical analysis. Arch Pathol Lab Med 2005; 129:1444-50.
5. Kabra NS, Bowen JR, Christie J, Glasson M. Mesenchymal hamartoma of chest wall in a new born. Indian Pediatr2000; 37:1010-3.
6. Okutan O, Ilvan A, Kartaloglu Z, Tunc H. Giant hamartoma originating from the chest wall in an adult. Saudi Med J 2006; 27:1054-6.
7. Mesenchymal hamartoma of the chest wall- mimicker of malignancy. Yeshvanth SK, Shivamurthy V, Patil C, Rai S, Lakshminarayana KP, Makannavar JH. J Cancer Res Ther. 2011 OctDec;7(4):496-8.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License