IJCRR - 13(1), January, 2021
Pages: 63-67
Date of Publication: 05-Jan-2021
Print Article
Download XML Download PDF
Prospective Evaluation of Factors Affecting the Outcome in Cirrhotic Patients Requiring Intensive Care
Author: Rohit N. Maidur, Sukanya B, Raghavendra Y, Ajitkumar S
Category: Healthcare
Abstract:Introduction: The short-term prognosis of acutely ill patients with cirrhosis is influenced by the degree of hepatic and extrahepatic organ dysfunction.
Objective: This study intends to find the parameters that influence the outcome in cirrhotics requiring critical care.
Methods: This was a single-centre, prospective, observational study. Prognostic scores were calculated on the day of admission and day 7. The appearance of new events and length of hospital stay was documented. Follow up was done at day 30 in person or by telephone for those who had left the hospital.
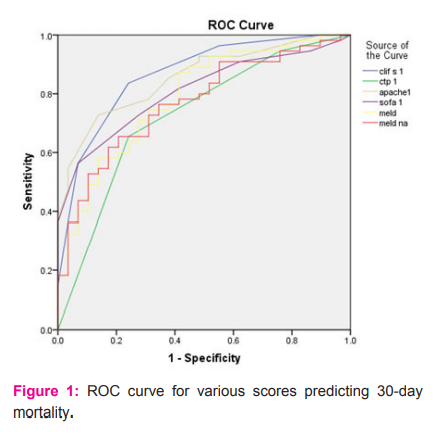
Results: Out of 96 subjects 12 were lost to follow up, 84 subjects followed of which 55 expired within 30 days of admission. On multivariate analysis older age, presence of Malena, oliguria, presence of infective foci, hepatic encephalopathy, low platelet count and pH, high lactate, creatinine, bilirubin, serum ferritin were predictors of mortality. Mean serum ferritin levels were significantly higher (p< 0.001) in non-survivors (922.95 \? 319.85) as compared to survivors (368.17\? 113.87). Lower ROC was observed for liver-specific scores CTP (0.727), MELD (0.79) and MELD Na (0.77) as compared to general ICU scores SOFA (0.808), APACHE II (0.855) on the day of admission.
Conclusions: CLIF SOFA score which is a combination of liver-specific scores and ICU scores should replace CTP and MELD to predict short term mortality in critically ill liver cirrhotics. Serum ferritin as a biomarker has good ability in anticipating the outcome. An ideal score should include ferritin along with the assessment of multi-organ functioning.
Keywords: Cirrhosis, MELD, CLIF- SOFA, Serum Ferritin
Full Text:
Introduction
Patients with advanced liver cirrhosis frequently require admission to the intensive care unit as they have a poor prognosis, with mortality rates ranging from 36% to 86%.1-3 The short-term prognosis of acutely ill patients with cirrhosis is influenced by the degree of hepatic insufficiency and by dysfunction of extrahepatic organ systems. Sepsis is the presence of cirrhosis is associated with poor prognosis; mortality rates increase with the increasing number of failing organs.5,6 Among the extrahepatic organ failures often encountered in end-stage liver disease, renal failure or dysfunction in cirrhotic patients has been the subject of extensive investigation7. Stratifying patients help differentiate those who could achieve a better outcome with aggressive treatment from those who would not benefit from admission to the intensive care unit.8
The Child-Turcott score and its subsequent modifications by Pugh are old empirical methods used to assess the degree of liver failure in candidate patients for Portosystemic shunt.9 The discriminatory power of this score relative to mortality in cirrhotic patients admitted to the ICU is inferior to that of general ICU scores like Sequential Organ Failure Assessment (SOFA) or Acute Physiology and Chronic Health Evaluation (APACHE)( 10). Model for End-Stage Liver Disease (MELD) score, initially developed for cirrhotic patients treated with Transjugular Intrahepatic Portosystemic Shunt (TIPS), has been applied widely to predict mortality across a broad spectrum of liver diseases (11). MELD score has its limitations one such is its inaccuracy in predicting survival in 15–20% critically ill patients.12
A modification of SOFA, the Chronic Liver Failure-SOFA (CLIF-SOFA) score, has been proposed for patients with cirrhosis hospitalized for acute decompensation.13-15 Cirrhotic patients with other organ dysfunction showed increased mortality, increasing with the number of organs affected,14 reaching 90% in patients with three or more organ dysfunctions. Based on reliable prognostic factors, interventions like liver assist devices or plasmapheresis can be initiated for critically ill cirrhotics. Whenever patients with cirrhosis are critically ill the question of utility and/or futility of placing them in ICU arise, especially in resource-constrained settings.16,17 This is a challenging situation and needs good scoring systems which can predict the utility of ICU. The present study is intended to find the parameters that influence the outcome in cirrhotics requiring critical care so that available resources can be put to best use.
Materials and methods
The study was a single-centre, prospective, observational study conducted between January 2015 and January 2016 at Department of Medical Gastroenterology, Nizam’s Institute of Medical Sciences (NIMS), Hyderabad after obtaining approval from Institutional Ethics Committee. Consecutive patients of liver cirrhosis requiring intensive care were recruited. The primary endpoint was a reassessment of scores at day 7 and mortality up to day 30.
Inclusion Criteria:
Consecutive patients more than 18 years of age with liver cirrhosis of any aetiology requiring intensive care were recruited.
Exclusion Criteria
-
Acute liver failure
-
Post-liver transplantation
-
HIV infection
-
Established case of hepatocellular carcinoma
-
Presence of severe comorbidities in the form of cerebrovascular accident, chronic kidney disease, severe cardiopulmonary insufficiency, ischemic heart disease, chronic obstructive pulmonary disease.
-
Post - hepatobiliary surgery
-
Procedure
The diagnosis of cirrhosis was based on clinical, radiological and laboratory parameters. History, physical examination, haematological and biochemical parameters, and imaging studies were done. Patient demographics and an indication of ICU admission were noted. Presence of co-morbid disease was documented. Prognostic scores were calculated on the day of admission and day 7. The appearance of new events and complications during the hospital course was noted. Length of ICU and hospital stay were documented. Standard of care was provided to all patients. Follow up was done at day 30 in person or by telephone for those discharged.
Results
Total of 96 patients was enrolled, 12 were lost to follow up. 84 patients (M/F: 77/7 completed the study. Alcohol was the most common aetiology (76.1%) followed by Hepatitis B (8.3%), Hepatitis C (4.7%) and alcohol with viral hepatitis (10.7%). 55 patients expired within 30 days of admission. Mean age amongst survivors was significantly lower than non-survivors (45 ± 9.32) vs. (50±8.067) (p <0.001).
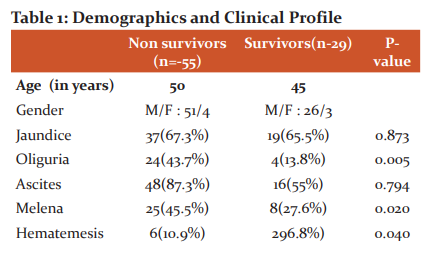
Ascites was the commonest symptom among both non-survivors (87.3%) and survivors (55%) with p =0.794. Jaundice was seen in both the groups of non-survivors (67.3%) and survivors (65.5%) with no statistical significance p=0.873 in predicting the outcome. Oliguria was seen in 24 (43.7%) of non-survivors and 4 (13.8%) of survivors with a p-value of 0.005. Malena was commoner than hematemesis at presentation in both non survivors (45.5% vs. 10.5%) and survivors (27.6% vs. 6.8%) with significant difference (p=0.02) [Table 1].
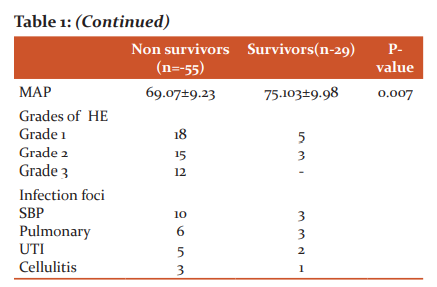
Mean arterial pressure was significantly different (p=0.007) among both the groups with lower values among non-survivors (69.07 ± 9.2388) than survivors (75.103 ± 9.982)[Table 1]. The requirement of inotrope support for maintenance of pressure was more frequently required in non-survivors (9/55) group than in survivors (3/29).
Among the blood indices haemoglobin (9 ± 1.11 vs 8.85 ± 2.73), and platelet counts (1.286 ± 0.4372 vs 0.9989 ± 0.467 lakhs /cum) were higher and total leucocyte count (13442.41 ± 4569.87 vs 15193 ± 5099.98 / cum) was lower among survivors than non-survivors, however only the platelet count showed statistical significance between both the groups (p=0.007).
Assessment of liver function tests showed SGOT (126 ± 76.36 vs 96 ± 102.29), SGPT (96 ± 102.29 vs 42 ± 65.43 ), INR (2.227 ± 0.6665 vs 2.051 ± 0.6593) were higher and albumin was lower in non survivors but significant difference (p=0.000) was noted only for bilirubin (24.265 ± 4.818 vs 17.075 ± 5.587 )[Table 2].
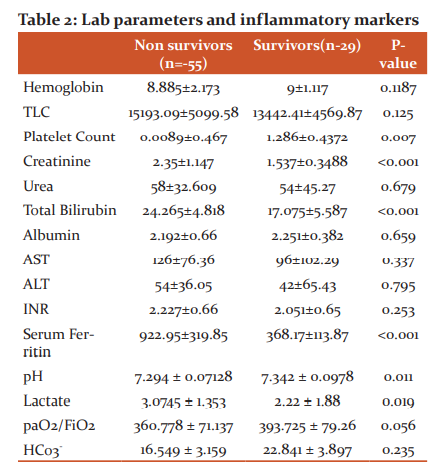
Blood urea and serum creatinine were higher among non-survivors (58 ± 32.609 and 2.35 ± 1.147) than survivors (54 ± 45.27 and 1.537 ± 0.348) but statistical significance was seen for serum creatinine (p<0.001) [Table 2]. Significantly higher (p=0.000) mean serum ferritin levels were noted in non-survivors (922.95 ± 319.858) when compared to survivors (368.17 ± 113.873) with a range of 102 to1746 and 270 to 717 [Table 2].
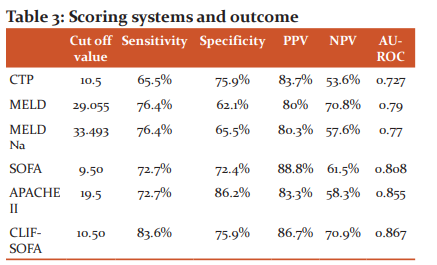
Among the scoring systems that were compared CLIF-SOFA had the highest sensitivity and APACHE II had the highest specificity with the highest AUROC noted with CLIF- SOFA [Figure 1, Table 3].
Discussion
Alcohol was the commonest aetiology seen in 76.1% of our subjects which can be explained by the male preponderance (M:F = 3.2:1) in our study because alcohol consumption is less common among women in this part of the world. In our series, the 30-day mortality was 66.7%. The mean age at presentation was higher among non-survivors compared to survivors. Older subjects had higher mortality possibly due to decreased functional reserves resulting in organ dysfunction with any additional insult.
Amongst the presenting complaints, oliguria and GI bleeding were statistically significant in predicting poor outcome. Mean arterial pressures and inotrope requirement was significantly different between the two groups reflecting the impact of GI bleed on hemodynamic stability and renal function and thereby the outcome. Similar findings were seen in a study by Chariff et al.14,19 SBP was the most common infection followed by pulmonary infections both in non-survivors and survivors. Urinary tract infection, cellulitis, hepatitis A and hepatitis E were other infections that precipitated downhill course. In comparison to previous studies17,23 we had a lower incidence of UTI, cellulitis and acute viral hepatitis; however, the mortality was comparable.
The platelet count showed a statistically significant difference between the two groups (p=0.007) indicative of advanced liver disease and portal hypertension in non-survivors. On blood gas analysis the mean levels of pH and lactate were significantly different between survivors and non-survivors [Table 2] indicative of severe ongoing inflammation. Bilirubin and creatinine were significantly different between the two groups again suggestive of decreased hepatic and renal reserves.
In our study mean serum ferritin levels were significantly higher (p<0.001) in non-survivors. Serum Ferritin, an indicator of body iron reserves is also an acute phase reactant and a surrogate marker of the necroinflammatory activity in liver parenchymal cells. Increased levels are known to predict poor outcome in decompensated liver cirrhosis.23 Similar results have also been observed in a study by Maiwall et al.20
Although initially derived for predicting post-procedure outcome, CTP and MELD scores have been extrapolated to predict survival in cirrhotic patients.21,22 These scores have been used in prioritizing organ allocation in cirrhotics waitlisted for liver transplantation. However when there is the rapid deterioration of the cirrhotic patients due to precipitating factors, prediction of outcome is challenging and CTP, MELD has not fared well in this. We observed lower ROC for liver-specific scores like CTP (0.727), MELD (0.79) and MELD Na (0.77) as compared to general ICU scores. In the present study general ICU scores SOFA (0.808), APACHE II (0.855) fared better in predicting outcome than liver-specific scores in critically ill liver cirrhotics. Zauner et al. retrospectively compared the prognostic abilities of liver-specific and general scoring systems and found that the APACHE system was the most accurate prognostic system.21 However, this study was done before the emergence of SOFA score hence not compared with it. Our study findings resemble a study by Alsherif et al. stating that SOFA is a better predictor than MELD.17 However, there are some limitations to the SOFA. Serum bilirubin, which is one of the parameters in the SOFA does not reflect the full spectrum of liver dysfunction in critical illness and cannot differentiate acute liver dysfunction from the effects of pre-existing chronic disease.22 Also, the Glasgow Coma Scale as the variable reflecting neurologic dysfunction has shortcomings. In our study CLIF – SOFA was the best predictor of outcome in critically ill cirrhotics (ROC=0.867) [Figure 1]. This score is a modification of SOFA score and includes additional liver specific parameters like prothrombin time as well as West Haven score to reflect neurologic impairment due to cirrhosis rather than a general neurologic dysfunction score like GCS.
Conclusions
Critically ill cirrhotics have a high mortality rate. Oliguria, GI bleeding, low mean arterial pressures can predict early mortality. Platelet count, bilirubin, lactate, pH and serum creatinine are good predictors of 30-day mortality. The general ICU scores SOFA, APACHE II are better than CTP and MELD in predicting outcome. The CLIF SOFA score which is a combination of liver-specific scores and ICU scores should replace CTP and MELD to predict short term mortality in critically ill liver cirrhotics. Serum ferritin as a biomarker has good ability in predicting the outcome. We hypothesize that the inclusion of ferritin in these scoring systems may improve the predicting power. An ideal score may be the one which includes ferritin along with organ dysfunction scores.
Source of funding – None to disclose
Conflicts of interest – None to disclose
Acknowledgement: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references to this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
-
Ruiz-del-Arbol L, Monescillo A, Arocena C, Valer P, Gines P, Moreira V, et al. Circulatory function and hepatorenal syndrome in cirrhosis. Hepatology (Baltimore, Md) 2005;42(2):439-47.
-
Aggarwal A, Ong JP, Younossi ZM, Nelson DR, Hoffman-Hogg L, Arroliga AC. Predictors of mortality and resource utilization in cirrhotic patients admitted to the medical ICU. Chest 2001;119(5):1489-9.
-
Chen YC, Tsai MH, Ho YP, Hsu CW, Lin HH, Fang JT, et al. Comparison of the severity of illness scoring systems for critically ill cirrhotic patients with renal failure. Clin Nephrol 2004 Feb;61(2):111-8.
-
Wehler M, Kokoska J, Reulbach U, Hahn EG, Strauss R. Short-term prognosis in critically ill patients with cirrhosis assessed by prognostic scoring systems. Hepatology (Baltimore, Md) 2001;34(2):255-61.
-
O'Brien AJ, Welch CA, Singer M, Harrison DA. Prevalence and outcome of cirrhosis patients admitted to UK intensive care: a comparison against dialysis-dependent chronic renal failure patients. Inten Care Med 2012 Jun;38(6):991-1000.
-
Arvaniti V, D'Amico G, Fede G, Manousou P, Tsochatzis E, Pleguezuelo M, et al. Infections in patients with cirrhosis increase mortality four-fold and should be used in determining prognosis. Gastroenterology 2010;139(4):1246-56.
-
Cárdenas A, Ginès P, Uriz J, Bessa X, Salmerón JM, Mas A, et al. Renal failure after upper gastrointestinal bleeding in cirrhosis: incidence, clinical course, predictive factors, and short-term prognosis. Hepatology 2001;34(4, Part 1):671-6.
-
Feltracco P, Brezzi M, Barbieri S, Milevoj M, Galligioni H, Cillo U, et al. Intensive care unit admission of decompensated cirrhotic patients: prognostic scoring systems. Transpl Proceedings 2011;43(4):1079-84.
-
Cholongitas E, Senzolo M, Patch D, Shaw S, Hui C, Burroughs AK. Review article: scoring systems for assessing prognosis in critically ill adult cirrhotics. Aliment Pharmacol Therap 2006;24(3):453-64.
-
Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology (Baltimore, Md) 2000;31(4):864-71.
-
Singal AK, Kamath PS. Model for End-stage Liver Disease. J Clin Exp Hepatol 2013;3(1):50-60.
-
Cholongitas E, Betrosian A, Senzolo M, Shaw S, Patch D, Manousou P, et al. Prognostic models in cirrhotics admitted to intensive care units better predict outcome when assessed at 48 h after admission. J Gastroenterol Hepatol 2008;23(8pt1):1223-7.
-
Austin MJ, Shawcross DL. Outcome of patients with cirrhosis admitted to intensive care. Curr Opin Crit Care 2008;14(2):202-7.
-
Iliass Charif, Kaoutar Saada, Ihssane Mellouki, Mounia El Yousfi, D.Benajah, Mohamed El Abkari, et al. Predictors of Intra-Hospital Mortality in patients with Cirrhosis. J Gastroenterol 2014;4:141-148.
-
Wong F, Bernardi M, Balk R, Christman B, Moreau R, Garcia-Tsao G, et al. Sepsis in cirrhosis: report on the 7th meeting of the International Ascites Club. Gut 2005;54(5):718-25.
-
Viasus D, Garcia-Vidal C, Castellote J, Adamuz J, Verdaguer R, Dorca J, et al. Community-acquired pneumonia in patients with liver cirrhosis: clinical features, outcomes, and usefulness of severity scores. Medicine 2011;90(2):110-8.
-
Alsherif A, Darwesh H, Badr M, Eldamarawy M, Shawky A, Emam A. SOFA Score as a Predictor of Mortality in Critically Ill Cirrhotic Patients. Life Sci J 2013;10(2).
-
Hamza RE, Villyoth MP, Peter G, Joseph D, Govindaraju C, Tank DC, et al. Risk factors of cellulitis in cirrhosis and antibiotic prophylaxis in preventing recurrence. Anna Gastroenterol 2014;2:28.
-
Jalan R, Fernandez J, Wiest R, Schnabl B, Moreau R, Angeli P, et al. Bacterial infections in cirrhosis: a position statement based on the EASL Special Conference 2013. J Hepatol 2014;60(6):1310-24.
-
Maiwall R, Kumar S, Chaudhary AK, Maras J, Wani Z, Kumar C, et al. Serum ferritin predicts early mortality in patients with decompensated cirrhosis. J Hepatol 2014 Jul;61(1):43-50.
-
Zauner CA, Apsner RC, Kranz A, Kramer L, Madl C, Schneider B, et al. Outcome prediction for patients with cirrhosis of the liver in a medical ICU: a comparison of the APACHE scores and liver-specific scoring systems. Inten Care Med 1996;22:559-56.
-
Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction scores: a reliable descriptor of a complex
clinical outcome. Crit Care Med 1995;23:1638-1652.
-
Oikonomou T, Goulis I, Soulaidopoulos S, Karasmani A, Doumtsis P, Tsioni K, et al. High serum ferritin is associated with a worse outcome of patients with decompensated cirrhosis. Ann Gastroenterol 2017; 30:217-224.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License