IJCRR - 13(1), January, 2021
Pages: 19-21
Date of Publication: 05-Jan-2021
Print Article
Download XML Download PDF
Comparative Analysis of Midazolam with Fentanyl Versus Midazolam with Propofol for Their Haemodynamic Stability During Regional Anesthesia
Author: Aditya Khot, Aparna Girish Benare
Category: Healthcare
Abstract:Introduction: Many methods have been recommended for the prevention of hemodynamic instability during induction of anaesthesia.
Objectives: To study Midazolam plus Fentanyl versus Midazolam plus Propofol concerning Hemodynamic stability during regional Anaesthesia.
Methods: We have conducted a comparative study of conscious sedation using midazolam with fentanyl in group-I Vs. midazolam with propofol in group-II. This study was conducted at a tertiary care centre for one year. 120 patients of ASA Grade I, II and III, were randomly divided into two groups, 60 in each group, of between 15 to 60 years.
Results: Systolic blood pressure changes in both the groups are comparable with each other at 30 minutes after sedation but fall in blood pressure was more in group II from the baseline. Statistically p< 0.001 is highly significant in both groups.
Conclusion: It can be concluded from our study that Systolic blood pressure changes in both the groups are comparable with each other at 30 minutes after sedation, but blood pressure fall was more in Midazolam plus Propofol group from the baseline.
Keywords: Midazolam plus Fentanyl, Midazolam plus Propofol, Hemodynamic stability, Propofol, Hypnotic agent
Full Text:
INTRODUCTION
Propofol is very commonly given hypnotic agent of choice but having its advantages & disadvantages. Anaesthesia induction with propofol is having some effects on hemodynamics in patients more than 50 years of age in the form of fall in blood pressure.1,2 In cases with the previous history of hypotension & in those cases with American society of anesthesiologists’ physical status (ASAPS) >II, this fall in blood pressure is extremely profound. Day by day, regional analgesia is getting very important in anaesthetic practice.1,2 Its most common advantages are like avoidance of risks due to general anaesthesia. They are like aspiration pneumonia due to reflux of gastric contents, laryngeal spasm or obstruction of airways, also it gives better postoperative experience.3,4 It has also got advantages in cases with pre-existing pulmonary embolism. Midazolam is a very commonly used agent for conscious sedation for short endoscopic or dental procedures & acts as an adjunct to local as well as regional anaesthesia. Propofol is a sedative-hypnotic agent & is getting very popular for local aesthetic procedures. Its high clearance rates & extremely favourable recovery profile has added advantage over other IV sedatives & analgesics. Also, one more advantage is that sedation due to propofol can be well adjusted by manual intermittent bolus injection technique.5 Fentanyl is a very potent synthetic opiate agonist (around many folds potent than morphine).
Fentanyl is extremely lipid soluble & it enters the Central Nervous system (CNS) very rapidly which in turn leads to the rapid onset of action. Due to its higher potency for controlling pain, it is becoming the narcotic drug of choice for a range of painful procedures. But comparatively, it has got a shorter duration of action.6-8
MATERIALS AND METHODS
We have conducted a comparative study of conscious sedation using midazolam with fentanyl in group-I Vs. midazolam with propofol in group-II. This study was conducted at a tertiary care centre for one year. 120 patients of the American Society of anaesthesiologists (ASA) Grade I, II and III, were randomly divided into two groups, 60 in each group, of between 15 to 60 years of either sex, undergoing any surgery under regional anaesthesia (spinal, epidural anaesthesia or peripheral nerve blocks). Patients having any history of allergy to any of the anaesthetic agents, or any chronic opioid use or obesity are excluded. Also, those cases who are having clinically significant cardiac, hepatic, renal or pulmonary dysfunction were excluded from our study. The institutional ethics committee approved the study.
Assessment of Sedation
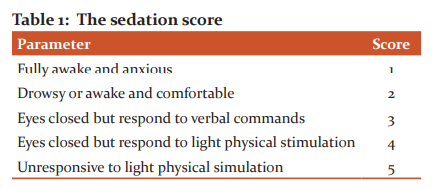
Table no 1 shows the sedation score of Fully awake and anxious, Drowsy or awake and comfortable, Eyes closed but responds to verbal commands, Eyes closed but responds to light physical stimulation and Unresponsive to light physical simulation
Patients were specifically asked regarding their awareness during the surgical procedure and whether they will be happy to have the same aesthetic technique again. The hemodynamic parameters like Blood pressure, Heart Rate etc. were recorded. The statistical analysis was done by SPSS 19 software.
RESULTS
Hemodynamic changes (systolic blood pressure)
Systolic blood pressure changes in both the groups are comparable with each other at 30 minutes after sedation, but blood pressure fall was more in group II from the baseline (Table 2)
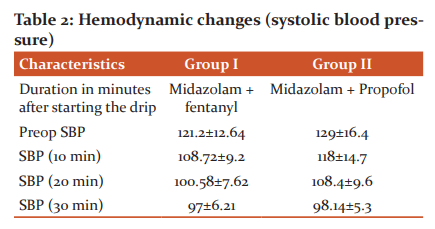
Table 2b and chart II shows heart rate (HR) changes in both the groups applying the test of significant changes in heart rate seen after sedation in group-I (Midazolam + Fentanyl) compare to group II (Midazolam+ propofol) ( Table 3).

DISCUSSION
The drop in propofol-induced systemic blood pressure is greater than that evoked by a comparable dose of thiopental. These decreases in blood pressure are also accompanied by related improvements in cardiac performance and systemic vascular resistance. Propofol-induced relaxation of the smooth vascular muscles is mostly due to the inhibition of propofol, which can result from a reduction in the influx of intracellular calcium. The effect of propofol on blood pressure is reversed by stimulation provided by direct laryngoscopy and trachea intubation, although the drug is more effective than thiopental in blunting the magnitude of the pressure response. Propofol also effectively blunts the hypertensive reaction to laryngeal mask airway positioning.6-8
The blood pressure effect of propofol can be underestimated in hypovolemic patients, elderly patients, and patients with reduced left ventricular function due to coronary artery disease. Adequate hydration before rapid IV administration of propofol is advised to minimise the blood pressure effects of this drug. Adding a dose of nitrous oxide would not affect the cardiovascular effects of propofol. After a decrease in systemic blood pressure, the heart rate still stays steady. Bradycardia and asystole were identified following induction of propofol anaesthesia, resulting in the occasional suggestion that anticholinergic drugs should be administered when the vagal stimulation is likely to occur in combination with propofol administration. High doses of fentanyl are also available at 50ug / kg IV. It does not elicit the release of histamine.9-11 As a result, it is doubtful that venous capacitance vessel dilation leading to hypotension may occur. Heart rate reflex control of the carotid sinus baroreceptor is significantly depressed with fentanyl (10 ug/kg, IV) administered to neonates. Bradycardia is more common with fentanyl than with morphine and can lead to periodic drops in blood pressure and heart output. Sedation was achieved after the bolus doses and this persisted throughout the procedure in both groups. Patients were instantly sedated following bolus in the propofol category without any hypotension or bradycardia. But it took 9 to 10 minutes for sufficient sedation in the opioid group to be achieved.11,12 In 5 patients from the opioid community, there was bradycardia and in 2 patients there was hypotension, so we decreased the doses by adjusting the micro drip and by prescribing IV fluids and atropine.13-15 And they avoided further blood pressure and heart rate declines. In our study, we found that, at 30 minutes after sedation, systolic increases in blood pressure in both groups were comparable to each other, but there was a greater drop in blood pressure from the baseline in group II. Significant improvements in the heart rate observed after sedation in group I (Midazolam+ Fentanyl) compared with group II (Midazolam+ propofol) were observed in the heart rate improvements in both test groups. Statistically, p<0.001 is extremely relevant in both groups.8,15
CONCLUSION
From our analysis, it can be concluded that systolic blood pressure changes in both groups were comparable to each other at 30 minutes after sedation, but there was a greater decrease in blood pressure in the Midazolam plus Propofol group from the baseline, even in heart rate.
Acknowledgement
Ethical clearance- Taken from the institutional ethics committee.
Conflict of Interest: Nil
Source of Funding: Nil
References:
-
Golzari S. Contributions of medieval Islamic physicians to the history of tracheostomy. Anesth Analg 2013; 116:1123–32.
-
Soleimanpour H. Effectiveness of intravenous Dexamethasone versus Propofol for pain relief in the migraine headache: A prospective double-blind randomized clinical trial. BMC Neurol 2012;12:114.
-
Dhungana Y. Prevention of hypotension during propofol induction: A comparison of preloading with 3.5% polymers of degraded gelatine and intravenous ephedrine. Nepal Med Coll J 2008; 10:16–9.
-
Taware M, Sonkusale M, Deshpande R. Ultra-Fast-Tracking in Cardiac Anesthesia ‘Our Experience’ in a Rural Setup. J Datta Meghe Inst Med Sci Uni 2017;12 (2); 110–14.
-
Yamaura K. Changes in left ventricular end-diastolic area, end-systolic wall stress, and fractional area change during anaesthetic induction with propofol or thiamylal. J Anesth 2000;14:138–42.
-
Modig J. Thromboembolism after total hip replacement: role of epidural and general anaesthesia. Anesth Anal 1983; 62: 174-80.
-
Freund F. ventilator reserve and level of the motor block during high spinal and epidural. Anaesthesia. Anesthesia 1967; 28: 834-7.
-
Rajan R, Gosavi S, Dhakate V, Ninave S. A Comparative Study of Equipotent Doses of Intrathecal Clonidine and Dexmedetomidine on Characteristics of Bupivacaine Spinal Anesthesia. J Datta Meghe Inst Med Sci Uni 2018;13(1); 4–8.
-
Jogren S. Respiratory changes during the continuous epidural blockade. Acta Anaesth Scandinavica 1972; 16: 27-49.
-
Wahba W. The cardiorespiratory effects of thoracic epidural anaesthesia. Canadian Anesth Soc J 1972:19: 8-19.
-
Aitkenhead A. Interaction with concurrent disease and medication. In: Henderson JJ, Nimmo WS, eds. Practical regional anaesthesia, oxford: Blackwell scientific publication, 1983, 143-62.
-
While P. sedative infusion during local and regional anaesthesia a comparison of midazolam and propofol. J Clin Anaesth 1991:3:32-9.
-
Taylor E. Midazolam in combination with propofol for sedation during local anaesthesia. J Clin Anesth 1992:4:213-6.
-
Seibs S. The treatment of pain the emergency department. Pediatr Clin North Am 1989:36,965-78.
-
Cafe CJ. Sedation for pediatric patients: A review. Pediatr Clin North Am 1994: 41; 31-58.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License