IJCRR - 8(6), March, 2016
Pages: 47-52
Date of Publication: 22-Mar-2016
Print Article
Download XML Download PDF
CHALLENGES IN THE MANAGEMENT OF SUBHEPATIC ACUTE APPENDICITIS IN THE EMERGENCY SETTING
Author: Bader Hamza Shirah, Hamza Assad Shirah, Wael Awad Alhaidari, Omer Elhag Abdulbagi
Category: Healthcare
Abstract:Introduction: Subhepatic acute appendicitis is a very rare variety of appendicitis that has rarely been reported and is difficult to diagnose. In our study, we aim to evaluate the clinical, diagnostic, and surgical approach done to 43 patients in the emergency setting to overcome the challenge. Patients and Methods: A retrospective cohort database analysis of 43 patients who were proven to have had subhepatic appendicitiswas done. 32 were male, and 11 were female (age range, 14\?23). All patients presented with an acute onset of the disease to the emergency department after regular working hours.Preoperative workup was the same to all patients (blood count, chemistry, chest and abdominal X-ray and ultrasound). All patients had emergency open appendectomy procedureand treated with cefazolin and metronidazole intravenously. Results: Preoperative proven diagnosis was achieved in 14 patients, and clinical suspicion dominated in 29 patients. The chief complaint was a sudden abdominal pain.Fever was reported in 43 patients, leukocytosis in 39 patients. Ultrasound detected 14 cases, suspected 9, and was inconclusive in 20 patients. 39 patients were treated through a laterally extended gridiron incision while 4 had a conversion to midline laparotomy. Postoperative morbidity and mortality rates were 0%. Conclusion: When subhepatic anatomical location of the appendix makes it difficult to diagnose acute appendicitis in the emergency setting, then a high level of clinical suspicion, prompt decision to operate, and skillful surgical approach could make a difference in the outcome of managing subhepatic acute appendicitis, and help to achieve zero postoperative morbidity and mortality.
Keywords: Acute appendicitis, Subhepatic appendicitis, Open appendectomy
Full Text:
INTRODUCTION Acute appendicitis is considered one of the most common abdominal emergencies, responsible for 1% of all surgical operations. As a result, appendectomy continues to be one of the commonest procedures in general surgery1 . The varying anatomical positions of the appendix are well established scientifically, which include a retrocecal position (65.28%), a pelvic (31%), a subcecal (2.26%), a preileal (1%) and a postileal (0.4%). The Subhepatic and lateral pouch are very rare variants. The subhepatic position of the appendix is the direct result of a developmental anomaly and was explained as a failure of descent of the caecum during the embryonic development2 . Diagnostic uncertainty due to the non-classical evolution of acute appendicitis may occur when the appendix is anatomically mal-located. At any age of presentation, variation in the location of the appendix due to adhesions or developmental anomalies could lead to a non-typical presentation, delays in the diagnosis and increased adverse outcomes3 .
In 1955, King described subhepatic appendicitis for the first time4 , but had rarely been reported since5 , with most cases being documented in case reports. Its incidence is 0.08% of all cases of appendicitis in one study from India6 . A research paper from Kenya reported 4.2% frequency of subhepatic appendix7 . A third paper reported 4% among Pakistani’s8 . Unfortunately, no statistical reports or papers were generated from Saudi Arabia. Subhepatic appendicitis usually presents with right upper abdominal pain. It is clinically indistinguishable from acute cholecystitis, and may mimic liver abscess, ureteric colic, or acute pyelonephritis. A delay in the diagnosis results in a ruptured appendix which is very rare9 . Preoperative diagnosis of subhepatic appendicitis is clinically difficultand usually diagnosed at laparoscopy for undiagnosed abdominal pain. Subhepatic appendicular abscess is the most common reported presentation. Abdomen ultrasound is usually used in suspected cases but computedtomography scan of the abdomen has been reported to be more sensitive in diagnosing acute appendicitis especially in young females.
In situations where abdominal computed tomography is inconclusive and clinical diagnosis of appendicitis is doubtful then diagnostic laparoscopy is recommended10. Magnetic resonance imaging was reported to be of value in visualizing the appendix in an atypical location. However, in the absence of the availability of emergency laparoscopic surgery or advanced imaging, the surgical management of these patients can be challenging. A delay in the diagnosis of subhepatic appendicitis may then lead to complications such as perforation and peritonitis11. In the emergency presentation where advanced diagnostic tools are not available, the clinical judgment and surgical experience should help in the early and safe management of subhepatic appendicitis. In our study, we aim to evaluate the clinical, diagnostic, and surgical approach done to 43 patients in the emergency setting to overcome the challenge.
MATERIALS AND METHODS A retrospective cohortdatabase analysis of themanagement method and outcome for patients who were confirmed to have had acute subhepatic appendicitis and subsequent open appendectomy as an emergency treatment in a public health general hospital in Medina, Saudi Arabia between January 2005 and December 2014 was done to evaluate the effectiveness of our response to patients with rare and abnormal position of the appendix among acute appendicitis patients presenting to our hospital emergency department which averages between 500-700 per year.
43 patients who were confirmed to have had open appendectomy for subhepatic acute appendicitis were included. All patients presented as an acute onset of the disease to the emergency department after regular working hours.Preoperative workup was the same to all patients (blood count, chemistry, abdominal X-ray and ultrasound). All patients had emergency open appendectomy procedure, and treated with cefazolin and metronidazole intravenously. Postoperative care was the same for all patients.
Retrospective database analysis was done concerning symptoms, duration of the disease, clinical presentation, laboratory and radiology investigations, the length of work up until decision to operate, operative method and findings, histopathology findings, and the outcome of treatment.All results were saved in a computerized database file for follow up and the statistical analysis was performed using the Statistical Package for Social Science (SPSS) program (Release 22).
RESULTS Between January 2005 and December 2014, the results of the 43 patients who were confirmed to have had open appendectomy for subhepatic acute appendicitis were analyzed. At the same period, the overall total number of patients treated in our hospital for various diseases was 79364 patients, and the total number of operated acute appendicitis cases in our hospital during the study period was 4279, while the number of operated subhepatic acute appendicitiscases was 43 patients.The incidence rate of subhepatic appendicitisamong all acute appendicitis in our hospital cases was 1 %. The incidence rate of subhepatic acute appendicitis in our hospital total Saudi Arabian population was 0.054 %.32(74.4%) patients were male and 11(25.6%) were female, ratio 2.9:1.
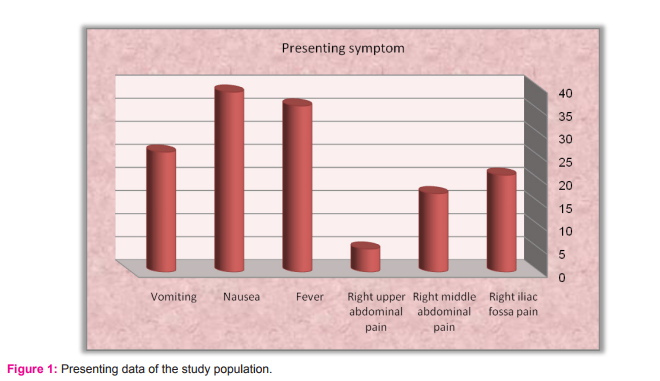
The age range was 14–23 years, (median = 18.5). All patients presented with a sudden acute onset of abdominal pain, 21(48.83%) had right iliac fossa pain, 17 (39.53%) had right middle abdominal pain, and 5 (11.62%) had right upper abdominal pain. The range of pain duration was 6-12hours before presentation (median = 9). Fever was reported by 36 (83.7%) patients, nausea by 39 (90.7%), vomiting by 26 (60.5%). (Figure 1) 41 (95.35%) reported first time attackwhile 2 (4.65%) reported similar attack within two weeks earlier treated conservatively. None of the patients had co-morbid diseases or previous surgery. Leukocytosis was reported in 39 (90.7%) patients.
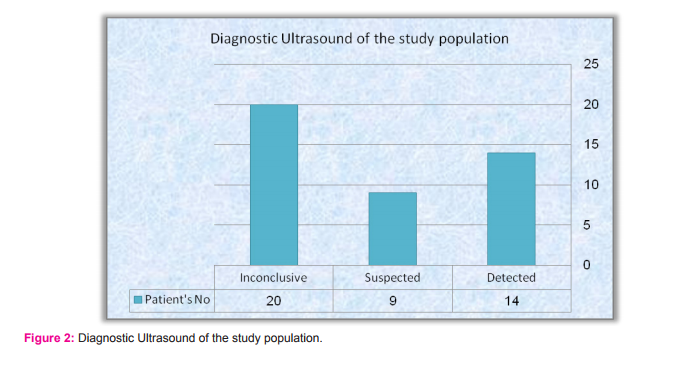
The rest of laboratory values were normal. Chest and abdominal X-ray were normal in all patients. Ultrasound detected 14 (32.55%) cases in which thickened wall appendix with free fluid around it was the main comment reported, suspected 9 (20.93%) in which free subhepatic fluid was the main positive finding, and was inconclusive in 20 (46.5%) patients. Sensitivity of ultrasound = True positive rate (TPR) = Diseased with positive test/Alldiseased = 23/43 = 0.5348 x100 = 53.5 %. (Figure 2)
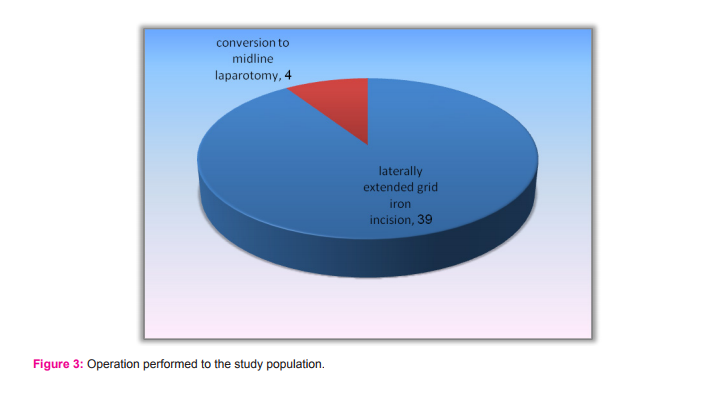
All patients were operated within 6 hours of presentation to the emergency departmentand treated with a single dose of cefazolin and metronidazole intravenously preoperatively. All patients had emergency open appendectomy procedure through grid iron right lower abdominal incision, 39 (90.7%) patients were managed through laterally extended gridiron incision while 4 (9.3%) had a conversion to midline laparotomy.No drains were used in any patient. The mean operative time was 105 ±5 minutes. (Figure 3) Postoperative care was the same to all patients.
All patients had 3 doses of cefazolin and metronidazole intravenously every 8 hours. Postoperative pain was managed similarly to other cases of appendectomy and laparotomy, and no significant difference was found in regard to laterally extended gridiron or converted laparotomy in our patients.No postoperative complications were recorded.The average hospital stay was 4-7 days (median = 5.5). Morbidity and mortality rates were 0%.Histopathology confirmed acutely inflamed appendix in all patients (100%). Negative appendectomy rate was 0%.
DISCUSSION Appendectomy remains the most frequently performed emergency abdominal surgical procedure. The reported lifetime risk of developing acute appendicitis in males and females is about 8.6% and 6.7% while the lifetime risk of having an appendectomy is 12% for men and 25% for women. The correct diagnosis of appendicitis is not straightforward in all cases. Approximately 20-33% of the patients suspected of having acute appendicitis present with atypical findings. The indication for surgical intervention is usually based on a combination of clinical and laboratory findings.
The significance of this diagnostic dilemma is the increased risk of developing a perforated appendicitis which could lead to an increased morbidity and a prolonged hospital stay. Logically, the most effective method to lower the rate of perforation is to adopt a lower threshold for the decision to take the patient to the operating room at the expense of increasing the negative appendectomy rate12. The clinical findings and experience remain of great significance in appendicitis diagnosis. When acute appendicitis appears with atypical presentations, it represents a clinical challenge. In such circumstances, laboratory and imaging investigation may be useful in establishing a correct diagnosis13. Subhepatic appendicitis is a rarely reported variant of a common surgical emergency that leads to delayed diagnosis and subjects to higher complication rates, including suppuration and perforation4 .
Appendicitis in unusual locations or situations always poses a diagnostic dilemma and surgery is never straightforward. Few reports in the literature described the surgical approach for these rare types of appendicitis.In the open technique, an extension of the incision would be required after finding that the appendix is in an abnormal position. Laparoscopy is reported to be of value in certain situations where doubt of the diagnosis is encountered. The location of the appendix could be visualized, and the other intraabdominal organs could be inspected6 . In the emergency sitting, where advanced diagnostic and operative modalities are not accessible, a high level of clinical suspicion contributes positively in the management of subhepatic acute appendicitis. And if combined with good surgeons experience in dealing with different and difficult presentations of acute appendicitis, could constitute a safe approachto subhepatic acute appendicitis patients, and effectively achieve a level of no postoperative morbidity and mortality.
The simple and easy to use emergency room ultrasound modality is helpful in bringing the clinical suspicion to high levels, either by accurately diagnosing the presence of subhepatic appendicitis, raising the probability by detecting signs of inflammation, or excluding other conditions that could mimic subhepatic appendicitis (acute cholecystitis,ureteric stones, or liver abscess). In our study, ultrasound detected 14 cases, suspected 9, and was inconclusive in 20 patients, but accurately excluded other conditions in all patients, especially acute calcular cholecystitis, which played an important role in the decision to operate. Recent studies have convincingly shown that ultrasound in experienced hands improve diagnostic accuracy14. Despite that all 43 patients presented to the emergency room at late day time (after regular working hours), all patient were operated within3 hours of emergency admission. The prompt decision to operate, even at night hours, contributed well to decrease the morbidity and mortality rates.
There was no perforation, no abscess formation, and no peritonitis, and thus 0% morbidity, and 0% mortality. In our emergency setting, laparoscopic instruments and technicians are not available after regular working hours according to the hospital’s policy. Therefore, all 43 patients had open appendectomy. The grid iron incision was favored due to the possibility of lateral extension. The appendix was not found in the normal position in all 43 patients. Lateral extension of the wound was done to all patients, and it successfully enabled visualization and resection of the subhepatic appendix in 39 patients (90.7%).
In 4 patients (9.3%), neither visualization nor resection were possible due to adhesions of the caecum to the lower liver edge, therefore, a midline laparotomy incision was done, followed by the release of ad-hesions, and appendectomy. The type and extent of incision did not adversely affect any patient in our study, except for the length and shape of the scar. In our study, 39 (90.7%) patients had high caecum and appendix fixed at the subhepatic level which could be considered as anatomical anomaly or congenital arrest of descend while in the other 4 (9.3%) patients, the caecum and appendix were loose, looping upward and attached by adhesions to the lower liver edge. In our study, we noticed that there was a delay in restoration of bowel motility postoperatively, 22 (51.2%) patients needed 48 hours to open their bowl and start an oral diet, and 21 (48.8%) patients required 72 hours to do so. We attributed that to the mobilization of the intestine during the search for the appendix, and to the adhesions found in the 4 laparotomy patients.
Fortunately, no bowel trauma was recorded. Careful and skillful approach to locate the subhepatic appendix is advised. Despite the difficulty in the diagnosis of subhepatic appendicitis, and the fact that in patients clinically diagnosed of acute appendicitis the reported overall negative appendectomy rate is about 15–20%; 10% in men and 25–45% in women of childbearing age15, in our study, histopathology confirmed the diagnosis of acutely inflamed appendix in all 43 patients. High clinical suspicion, and mild to moderate investigative probabilities in the management of subhepatic acute appendicitis should not be confronted by doubt or fear of negative appendectomy. Prompt decision to operate is a key stone in the successful management.
CONCLUSIONS We conclude that when subhepatic anatomical location of the appendix makes it difficult to diagnose acute appendicitis in the emergency setting, then a high level of clinical suspicion, prompt decision to operate, and skillful surgical approach could make a difference in the outcome of managing subhepatic acute appendicitis, and help to achieve zero postoperative morbidity and mortality.
Authors’ contributions All authors have contributed substantially to the paper. BHS wrote, edited the manuscript, and analyzed the clinical data. HAS conducted the clinical part of the study. WAA and OEA participated in the clinical part of the study and the data collection. All authors read and approved the final manuscript.
Competing interests The authors declare that they have no competing interests.
ACKNOWLEDGEMENT Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Ethical Clearance The study was approved by the quality control subcommittee for management guidelines and clinical pathway in Al Ansar general hospital. Informed Consent Not needed as it is a retrospective cohort database study. Source of Funding None received.
References:
1. Ball CG, Kortbeek JB, Kirkpatrick AW, Mitchell P. Laparoscopic appendectomy for complicated appendicitis: an evaluation of postoperative factors. SurgEndosc. 2004;18(6):969-73.
2. Rappaport WD, Warneke JA. Subhepatic appendicitis. Am Fam Physician. 1989;39(6):146-8.
3. Schumpelick V, Dreuw B, Ophoff K, Prescher A. Appendix and cecum. Embryology, anatomy, and surgical applications. SurgClin North Am. 2000;80(1):295-318.
4. King A. Subhepatic appendicitis. AMA Arch Surg. 1955;71(2):265-7.
5. Kulvatunyou N, Schein M. Perforated subhepatic appendicitis in the laparoscopic era. SurgEndosc. 2001;15(7):769.
6. Palanivelu C, Rangarajan M, John SJ, Senthilkumar R, Madhankumar MV. Laparoscopic appendectomy for appendicitis in uncommon situations: the advantages of a tailored approach. Singapore Med J. 2007;48(8):737-40.
7. Mwachaka P, El-busaidy H, Sinkeet S, Ogeng’o J. Variations in the position and length of the vermiform appendix in a black kenyan population. ISRN Anat. 2014;2014:871048.
8. Iqbal T, Amanullah A, Nawaz R. Pattern and positions of vermiform appendix in people of Bannu district. Gomal Journal of Medical Sciences. 2012; 10(2): 100–103.
9. Kraemer M, Franke C, Ohmann C, Yang Q. Acute appendicitis in late adulthood: incidence, presentation, and outcome. Results of a prospective multicenter acute abdominal pain study and a review of the literature. Langenbecks Arch Surg. 2000;385(7):470-81.
10. Kumar N, Rehmani B, Kumar A, Chug B. Subhepatic Appendicitis: A Diagnostic Dilemma. The Internet Journal of Surgery. Volume 32. Number 1.
11. Singh S, Jha AK, Sharma N, Mishra TS. A case of right upper abdominal pain misdiagnosed on computerized tomography. Malays J Med Sci. 2014;21(4):66-8.
12. Khairy G. Acute appendicitis: is removal of a normal appendix still existing and can we reduce its rate?. Saudi J Gastroenterol. 2009;15(3):167-70.
13. Althoubaity FK. Suspected acute appendicitis in female patients. Trends in diagnosis in emergency department in a University Hospital in Western region of Saudi Arabia. Saudi Med J. 2006;27(11):1667-73.
14. Zielke A, Hasse C, Sitter H, Rothmund M. Influence of ultrasound on clinical decision making in acute appendicitis: a prospective study. Eur J Surg. 1998;164(3):201-9.
15. Balthazar EJ, Rofsky NM, Zucker R. Appendicitis: the impact of computed tomography imaging on negative appendectomy and perforation rates. Am J Gastroenterol. 1998;93(5):768-71.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License