IJCRR - 8(6), March, 2016
Pages: 01-04
Date of Publication: 22-Mar-2016
Print Article
Download XML Download PDF
ASTIGMATIC CHANGES FOLLOWING PTOSIS CORRECTION SURGERY IN 30 CONSECUTIVE CHILDREN SEEN IN A REGIONAL INSTITUTE OF OPHTHALMOLOGY
Author: Garima Agrawal, Swati Ravani
Category: Healthcare
Abstract:Introduction: Astigmatic changes induced by upper lid repositioning may be a cause of blurred vision after upper eyelid procedures. We designed a study to document the astigmatic changes after ptosis correction surgery in children. Aim: The study aims at documenting the changes in astigmatism after ptosis correction surgery in 30 consecutive children seen in a Regional Institute of Ophthalmology. Material and Methods: 30 consecutive paediatric patients (4-12 years of age) of blepharoptosis were enrolled. The patients were subjected to a complete ophthalmic examination and ptosis evaluation. Keratometry and cycloplegic refraction were done pre and post- ptosis correction surgery. Observations and Results: The average pre-operative astigmatism was 1.28 while the average observed post- operative astigmatism was 1.71. The average post- operative change in astigmatism was 0.43 which was statistically significant. Conclusion: There is a significant astigmatic change following ptosis surgery in children. Mandatory visual acuity testing, refraction and post mydriatic correction are recommended in all paediatric patients with ptosis at the time of presentation and three months post surgery.
Keywords: Astigmatism, Paediatric patients, Ptosis correction surgery
Full Text:
INTRODUCTION Astigmatic changes induced by upper eyelid repositioning may be a cause of blurred vision after upper eyelid procedures. Procedures that reposition the upper eyelid alter pressure exerted on the opposing cornea and change pre-existing corneal curvature. Such changes potentially alter the corneal refraction and may be responsible for persistent blurred vision after upper lid blepharoplasty , ptosis repair and gold weight implantation. We designed a study to document the astigmatic changes after ptosis correction surgery in children.
AIM The study aims at documenting the changes in astigmatism after ptosis correction surgery in 30 consecutive children seen in a regional institute of ophthalmology.
MATERIAL AND METHODS 30 consecutive paediatric patients of blepharoptosis presenting to our regional institute of Ophthalmology were enrolled. Children less than 4 years of age who may not co-operate for full ophthalmic examination were excluded from the study. Children upto 12 years of age were included in our study. Other exclusion criteria includedcases of complicated ptosis, any corneal pathology, glaucoma, prior intraocular surgery and prior eyelid surgery. All patients were subjected to a complete ophthalmic examination visual acuity testing, ptosis evaluation, levator function, bell’s phenomenon and ocular movements. Ptosis was classified as mild, moderate or severe. Full cycloplegic refraction after dilation with homatropine eye drops, fundus examination and standardized keratometry with Bausch and Lomb keratometer were carried out. Surgical techniques for ptosis correction were fasanellaservat surgery, levator resection and frontalis sling surgery as per protocol. After surgery keratometry and cycloplegic refraction were repeated at one week, six weeks and three months post- operatively.
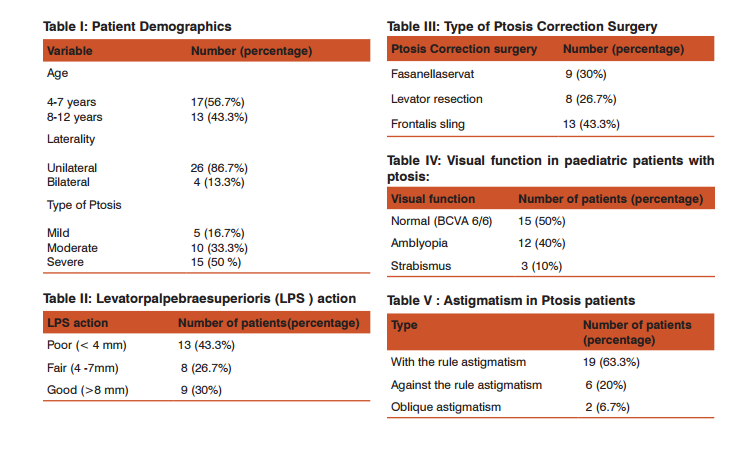
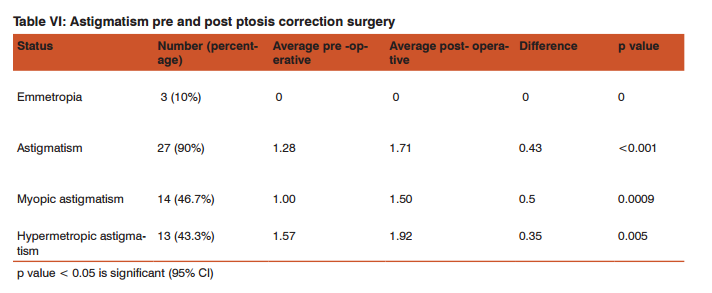
Observations and Results Table I shows the patient demographics. 17 (56.7%) children were between 4 to 7 years. 13(43.3%) children were between 8- 12 years of age. Ptosis was unilateral in 26 (86.7%) children and bilateral in 4(13.3%). Mild ptosis was seen in 5 (16.7%) cases, moderate in 10 (33.3%) and severe in 15(50%). Table II shows the levatorpalpebraesuperioris (LPS action). 13 (43.3%) patients had poor (8mm) LPS action. Table III documents the type of ptosis correction surgery performed as per the case. Fasanellaservat procedure was done in 9 (30%) cases, levator resection in 8 (26.7%) and frontalis sling surgery in 13 (43.3%) cases. Table IV shows visual function in paediatric patients with ptosis. Visual function was normal (best corrected visual acuity 6/6) in 15 (50%) patients. 12 (40%) patients were amblyopic while 3 (10%) children had strabismus. Table V documents the astigmatism in ptosis patients. With the rule astigmatism was documented in 19 (63.3%) patients, against the rule astigmatism was present in 6 (20%) patients and oblique astigmatism was seen in 2 (6.7%) patients. Table VI shows the astigmatism pre and post ptosis correction surgery. 3(10%) cases remained emmetropic. 27(90%) cases showed an astigmatic shift.Myopic astigmatism was seen in 14(46.7%) and hypermetropic astigmatism in 13(43.3%).
Average pre-operative astigmatism was 1.28. The average post- operative astigmatism was 1.71. The difference between the two was 0.43 which was statistically significant. 14 cases had an average pre-operative myopicastigmatic correction of 1.00 while the average post- operative myopic astigmatic correction was 1.50. The difference was 0.50 which again was statistically significant. 13 cases had a pre -operative hypermetropic astigmatic correction of 1.57 and an average post-operative hypermetropic astigmatic correction of 1.92. The difference between the two was 0.35. The results were statistically significant as evidenced by a p value of < 0.05.
DISCUSSION Our study documents the astigmatic changes seen following ptosis correction surgery in children. The study also documents the demography and clinical presentation of the recruited cases. Children between 4- 12 years of age were recruited. Majority of patients had unilateral(86.7%), moderate- severe (83.3%) ptosis. Most children had poor (43.3%) to fair (26.7%) levator action. Accordingly majority of the patients were subjected to either levator resection(26.7%) or frontalis sling surgery (43.3%). The documented visual function in paediatric ptosis patients was 6/6 with correction in 50% patients. Amblyopia (40%) and strabismus (10%) were observed in the remaining half. The observed astigmatism in ptosis patients was with the rule in most patients (63.3%). In paediatric patients with ptosis almost all (90%) showed association with astigmatism. The astigmatism was myopic in 46.7% and hyperopic in 43.3%. We documented the pre- operative astigmatism and final threemonth post -operative astigmatism. The average pre- operative astigmatism was 1.28 D while the average post- operative astigmatism was 1.71 D.
The difference 0.43 D had a p value of <0.001 which was statistically significant. The average pre- operative myopic astigmatism was 1.00 while the average post -operative value of myopic astigmatism was 1.50. the difference was 0.5 with a p value of 0.0009 which was again statistically significant. The average pre- operative hyperopic astigmatism was 1.57 and the corresponding post- operative value was 1.92. The difference was 0.35 with a p value of 0.005 which was statistically significant. Brown MS et al in a prospective analysis of changes in corneal topography after upper eyelid surgery reported that after ptosis repair, the average dioptric change as measured by keratometry and corneal videokeratography was approximately 0.60 Dioptres.1 Cadera W, Orton RB et al in their study on changes in astigmatism after surgery for congenital ptosis reported there was an overall increase in average astigmatic refractive error of the study group by 0.30 dioptres, while the control group decreased by 0.15 D.
Results were similar for both fascia lata slings and levator resections. 2 Klimek DL et al in their study on the change in refractive error after unilateral levator resection for congenital ptosis reported that the mean refractive change in the operated eye was 1.23 D sphere (p = 0.061) and 0.83 D cylinder (p=0.002) .The latter was statistically significant. Within the group of control eyes, no significant mean spherical or cylindrical changes were found at the last post operative visit.3 Kao SC, Tsai CC et al in their study on astigmatic change following congenital ptosis surgery reported an average decrease of 0.18D in astigmatism with no statistical difference between the study and control group for astigmatic change.
In 63 cases of congenital ptosis ,30.2% were associated with anisometropia and 39.7% with amblyopia .11.15 were combined with strabismus. The incidence of high astigmatism >2.5 D in congenital ptosis was 25.3%.4 The results of most of these studies were similar to those observed in our study group.
CONCLUSION We conclude that there is a significant astigmatic change following ptosis surgery in children. On documenting the demography and clinical presentation of paediatric patients with ptosis we observed that astigmatism was associated with paediatric ptosis in 90% cases while amblyopia was documented in 40% cases. We conclude that paediatric patients with ptosis must undergo careful visual acuity, cycloplegic refraction and post mydriatic correction at time of presentation. Three month cycloplegic refraction and post mydriatic correction after ptosis repair surgery are also recommended.
ACKNOWLEDGEMENT Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/ editors/publishers of all those articles journals and books from where the literature for this article has been reviewed and discussed. Ethical Clearance: Taken Informed Consent: Taken Source of funding : none Conflict of Interest: none
References:
1. Brown MS, Siegel IM, Lisman RD. Prospective analysis of changes in corneal topography after upper eyelid surgery. Ophthal Plast Reconstr surg. 1999;15(6): 378-83.
2. Cadera W, Orton RB. Hakim O. Changes in astigmatism after surgery for congenital ptosis. J Paediatr Ophthalmol Strabismus. 1992; 29(2):85-88.
3. Klimek DL, Summers CG, Letson RD, Davitt BV. Change in refractive error after unilateral levator resection for congenital ptosis. J AAPOS. 2001;5(5) :297-300.
4. Kao SC, Tsai CC, Lee SM, Liu JH. Astigmatic change following congenital ptosis surgery. Zhonghera Yi XueZaZhi. 1998;61(12):689-693.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License