IJCRR - 8(7), April, 2016
Pages: 04-07
Date of Publication: 12-Apr-2016
Print Article
Download XML Download PDF
DOES BODY MASS INDEX EFFECT NERVE CONDUCTION? A CROSS SECTIONAL STUDY
Author: Vineeta Chadha, Surendra S. Shivalkar
Category: Healthcare
Abstract:Aim: Body mass index (BMI) is an important parameter in gauging adiposity and obesity. Many studies have shown higher incidence of cardiovascular diseases especially coronary artery diseases in population with BMI greater than 25. (1) Studies also reveal median and ulnar nerve compression associated with an increasing incidence of higher BMI. (2) This study is an attempt to establish a relationship between median nerve conduction parameters and BMI in a population group from a metropolitan city in urban India. Methodology: In the present study the effect of Body Mass Index (BMI) on Median nerve motor and sensory conduction latency, amplitude and velocity was analysed in 90 healthy people in the age group of 18-30 years. Standardized protocol was followed while performing nerve conduction study in all the subjects. Results: This study shows that sensory nerve conduction amplitude decreases significantly with increase in BMI whereas the effect on other parameters is non-significant. Conclusion: This could be attributed to attenuation in conduction current by thicker subcutaneous tissue in persons with higher BMI. Median nerve latency and conduction velocity do not show significant decrease. This could be due to the fact that speed of conduction is same in the fastest conducting fibres irrespective of the adiposity..
Keywords: Nerve conduction velocity, Nerve conduction latency, Nerve conduction amplitude, Body mass index, Median nerve
Full Text:
INTRODUCTION
Nerve conduction study is used in the diagnosis of focal or diffuse peripheral neuropathies. Various study parameters are used to differentiate between the types of neuropathies and to know the extent and distribution of lesion. (3) Nerve conduction studies (NCS) are in turn affected by gender, age, height, weight and temperature. (4) Past studies have shown that high BMI is a risk factor for carpel tunnel syndrome and variation of body mass index (BMI) from normal is a risk factor for ulnar neuropathy at elbow. (2) Negative correlation has been shown between BMI and sensory nerve action potential amplitude (5).
BMI is an important factor taken into consideration while assessing peripheral neuropathy in diabetic patients. (6) Influence of BMI on nerve conduction velocity has been evaluated, however, majority of these studies are based on Caucasian subjects. (7) This study is aimed at deriving normative reference data on Indian population that closely relates to the demographic profile of the patients being studied. It has been hypothesized in this study that high BMI leads to decrease in nerve conduction velocity, increase in latency and decrease in amplitude of nerve conduction.
MATERIALS AND METHODS
The study was conducted in a teaching college and hospital in Mumbai with prior permission of the ethical committee on 90 healthy volunteers in the age group of 18-30yrs. Through relevant history and neurological examination, subjects with medical conditions (Diabetes Mellitus, Thyroid Disorders, Neuromuscular disorders, Drug Abuse and Chronic Alcohol Abuse) or on drugs (Antiretroviral, Antitubercular) that could affect nerve conduction were excluded. A brief explanation of the procedure was given to the subjects and voluntary informed consent was taken. Height and weight of each subject was recorded and BMI was calculated as weight (kg) divided by height (m) squared.
The study group was divided into 3 depending upon the value of BMI (BMI25). The amplitude, latency and conduction velocity were measured for Compound Muscle Action Potential (CMAP) as well as Sensory Nerve Action Potential (SNAP) component of median nerve prospectively using NEURO – MEP – NET EMG/NCV/EP (NEUROSOFT) equipment according to standard protocol and settings at a room temperature of between 24-30o C. (8, 9) For motor nerve conduction study the low frequency filter was set at 2 Hz and high frequency filter at 10 kHz. For sensory nerve conduction study the low frequency filter was set at 5 Hz and high frequency filter at 3 kHz.
The sweep speed was set at 2 milliseconds/division. (8, 9) Motor NCS requires stimulation of a nerve while recording from a muscle innervated by that nerve, whereas sensory NCS require stimulating a mixed nerve while recording from a mixed or cutaneous nerve. (10) Median motor and sensory nerve conduction velocity were recorded as described by Mishra and Kalitha. (8) Recording electrode was placed on the motor point of Abductor Pollicis Brevis, reference electrode 3cm distal to recording electrode and ground electrode was placed on dorsum of the hand for Median motor nerve conduction parameters.
Similarly median sensory conduction was performed orthodromically with respective electrodes placed on appropriate sites. (8) Conduction velocity, latency and amplitude of the median nerve were taken for analysis. ANOVA was used to analyse the effect of BMI on nerve conduction velocity, latency and amplitude. Pearson’s correlation coefficient (r) was used for finding correlation between BMI and Nerve conduction velocity, latency and amplitude.
Observations and Results
Data was statistically analyzed using appropriate tests after adjusting for age and sex. With increasing BMI, there was a decrease in amplitude of sensory median nerve which was statistically significant. No correlation was noted between BMI and nerve conduction velocity and latency. Motor and sensory nerve conduction amplitudes correlated significantly (P < or = 0.05) with BMI.
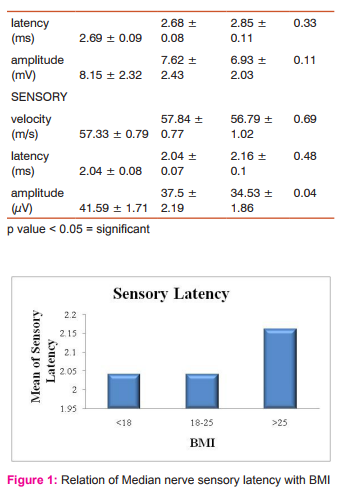
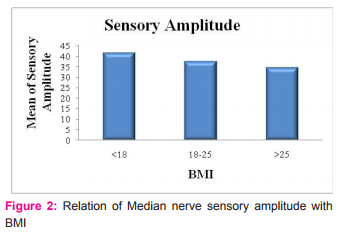
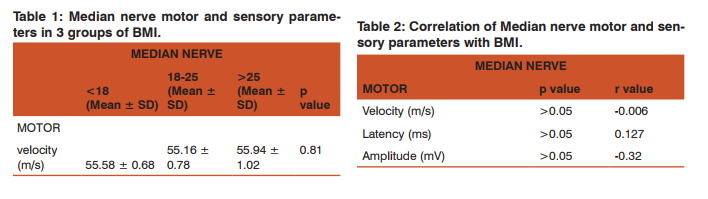
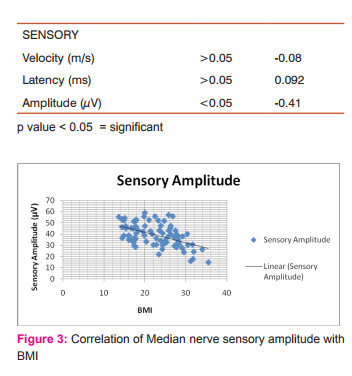
DISCUSSION In this study, effect of body mass index (BMI) on nerve conduction parameters for median nerve was evaluated. Results were statistically analyzed and normal values for median nerve conduction in healthy Indian population calculated. The findings of this study are similar to, Buschbacher RM et al (7) who showed that sensory and mixed nerve amplitudes correlated significantly (p < or = 0.01) with BMI for all the tested nerves. This study shows correlation between sensory amplitudes but not with mixed nerve amplitudes. Mean of amplitudes in subjects with higher BMI (obese) was less than in thin subjects.
This could be attributed to the fact that thicker subcutaneous tissue in persons with higher BMI causes amplitude attenuation. Hasanzadeh P et al. also showed that sensory amplitudes decrease but motor amplitudes are spared with increasing BMI. (5) This could be due to the thousand times rise in motor amplitude voltage (millivolts) as compared to sensory amplitude (microvolt). Also, Buschbacher RM et al (7) did not observe significant association of decrease in latency with higher BMI for median nerve which was similar to the findings in our study.
This observation might be due to the fact that median nerve being deeper is not much dependent on subcutaneous fat thermal insulation to maintain perineural temperature and thus individuals with various height and weights or BMI have almost similar temperatures around this nerve causing similar latent periods of conduction. They also reported no correlation between BMI and nerve conduction velocity, latency or most of the other motor and sensory parameters. This could be attributed to the fact that the speed of conduction is equal in fastest fibres in obese and thin individuals. The findings of this study are in contrast with Awang MS et al (10) who showed decrease in conduction velocity in median nerve with increasing BMI. In this study no significant increase or decrease in sensory and motor median nerve conduction velocity was found. The findings of this study are also in contrast with Baqai HZ et al (11) where no effect of BMI on nerve conduction parameters was reported. The present study also found greater influence of BMI on sensory nerve conduction as compared to motor nerve conduction studies. This was similar to the findings reported by Buschbacher RM (7) and Pawar et al (12).
Vessey et al. described an increasing risk of developing Carpel tunnel syndrome in women with higher BMI.(13) Kouyoumdjian et al. demonstrated in Brazilian population, that increasing BMI is correlated with a higher relative risk for developing compressive neuropathy. (14) Werner et al. found that the likelihood of developing median mononeuropathy at the wrist was 2.5 times higher in obese individuals (BMI > 29) than the slender ones (BMI < 20). (15) Thus there is a causal relationship between changed median nerve conduction parameters and increased BMI causing neuropathies which could be due to increased hydrostatic pressure or fatty tissue within the carpal tunnel in obese individuals. (15) Therefore the correlation between increased BMI and lower median sensory nerve amplitudes should be taken into account in clinical practice.
Another aspect is the increase in production of adipokines like plasminogen activator inhibitor-1 (PAI-1), tumor necrosis factor-alpha (TNF-α), resistin, leptin, and adiponectin in subjects with high BMI. (16) Adipocytes induce production of reactive oxygen species initiating the process of oxidative stress. (17) Diminished activity of antioxidant enzymes such as catalase, superoxide dismutase, and glutathione peroxidase due to increasing adiposity could be implicated in causing free radical injury. Hence it is highly recommended that studies be conducted on molecular level to establish a relationship between nerve conduction parameters, increasing level of adipokines and oxidative stress.
CONCLUSION In conclusion this study demonstrates that most of the parameters of nerve conduction study are not significantly associated with BMI. However the correlation between increased BMI and decreasing sensory nerve action potential amplitudes should be considered while testing for carpel tunnel syndrome and neuropathies in obese subjects.
ACKNOWLEDGEMENT Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. Source of Funding: None Conflict of interest: None stated
References:
1. Romero-Corral A, Montori V M, Somers V K, Korinek J, Thomas R J, Allison T G, Mookadam F, Lopez-Jimenez F. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: A systematic review of cohort studies. Lancet. 2006 Aug 19;368(9536):666-78.
2. Landau ME, Barher KC, Campbell WW. Effect of body mass index on ulnar nerve conduction velocity, ulnar neuropathy at elbow and carpal tunnel syndrome. Muscle Nerve 2005; 32(3): 360–363.
3. Kimura J. Principles and pitfalls of nerve conduction studies. Ann Neurol 1984; 16: 415-429.
4. Chi-Ren Huang, Wen-Neng Chang, Hsueh-Wen Chang, NaiWen Tsai, and Cheng-Hsien; Effects of Age, Gender, Height, and Weight on Late Responses and Nerve Conduction Study Parameters; Lu Acta Neurol Taiwan 2009;18:242-249
5. Hasanzadeh P, Oveisgharan S, Sedighi N, Nafissi S. Effect of skin thickness on sensory nerve action potential amplitude. Clin Neurophysiol 2008; 119(8): 1824–1828.
6. Xuan Kong, Eugene A. Lesser, Frisso A. Potts, Shai N. Gozani. Utilization of Nerve Conduction Studies for the Diagnosis of Polyneuropathy in Patients with Diabetes: A Retrospective Analysis of a Large Patient Series. J Diabetes Sci Technol. 2008 March; 2(2): 268–274.
7. Buschbacher RM. Body mass index effect on common nerve conduction study measurements.Muscla Nerve, 1998 Nov; 21(11):1398-404
8. Misra U K, Kalita J. Clinical Neurophysiology, 2nd Edition: 1-128.
9. Misulis KE, Head TC. Nerve conduction study and electromyography. In: Pioli SF, editors. Essentials of Clinical Neurophysiology. 3rd Ed. Burlington: Butterworth-Heinemann; 2003. p.129-144.
10. Awang MS, Abdul lah JM, Abdul lah MR, Tharakan J, Prasad A, Husin ZA, Hussin AM, Tahir A, Razak SA. Nerve conduction study among healthy Malays . The influence of age, height, and body mass index on Median, ulnar , common peroneal and sural nerves. Malaysian Journal of Medical Sciences 2006; 13(2): 19–23.
11. Baqai HZ, Tariq M, Din AMU, Khawaja I, Irshad M. Sural nerve conduction; Age related variation studies in our normal population. The Professional 2001; 08(04): 439–444.
12. Sachin M. Pawar, Avinash B. Taksande and Ramji Singh. Effect of body mass index on parameters of nerve conduction study in Indian population. Indian J Physiol Pharmacol 2012; 56(1) : 88–93
13. Vessey MP, Villard-Mackintosh L, Yeates D. Epidemiology of carpal tunnel syndrome in women of childbearing age:findings in a large cohort study. Int J Epidemiol 1990;19:655-659.
14. Joao Aris Kouyoumdjian, Maria Da Penha Ananias Morita, Paulo Ricardo Fernando Rocha, Rafael Carlos Miranda, Gustavo Maciel Gouveia. Body Mass Index And Carpal Tunnel Syndrome. Arq Neuropsiquiatr 2000;58(2-A):252-256
15. Werner RA, Albers JW, Franzblau A, Armstrong TJ. The relationship between body mass index and the diagnosis of carpal tunnel syndrome. Muscle Nerve 1994;17:632-636.
16. Fonseca-Alaniz, M.H.; Takada, J.; Alonso-Vale, M.I.; Lima, F.B. Adipose tissue as an endocrine organ: From theory to practice. J. Pediatr. 2007, 83 (Suppl. 5), S192–S203.
17. Alba Fernandez-Sanchez, Eduardo Madrigal-Santillan, Mirandeli Bautista, Jaime Esquivel-Soto, Angel Morales-Gonzalez, Cesar Esquivel-Chirino, Irene Durante-Montiel, Graciela Sanchez-Rivera, Carmen Valadez-Vega and Jose A. MoralesGonzalez. Inflammation, Oxidative Stress, and Obesity. Int. J. Mol. Sci. 2011, 12, 3117-3132.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License