IJCRR - 8(8), April, 2016
Pages: 27-31
Date of Publication: 20-Apr-2016
Print Article
Download XML Download PDF
TO STUDY THE PREVALENCE OF ATTENTION DEFICIT HYPERACTIVITY DISORDER (ADHD) AMONGST ADOLESCENT CHILDREN REFERRED FOR BEHAVIOURAL PROBLEMS TO TERTIARY CARE RURAL MEDICAL INSTITUTE IN CENTRAL INDIA
Author: Vaidya A., Dua H., Mujawar N., Edbor A.
Category: Healthcare
Abstract:Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, disorganization, and/or hyperactivity/impulsivity. Aims and Objectives: To study the prevalence of ADHD in adolescents referred for behavioral problems to rural tertiary health care center, to identify the gender difference andco-morbid factors associated with ADHD. Materials and Methods: Present study was a hospital based cross sectional study done at rural tertiary health care centre in central India. Multi Health Systems (MHS) CONNERS-3 questionnaire was used for assessment. Adolescent boys/girls referred by school or brought by their parents for behavioral problems at Child Guidance Clinic, Department of Pediatrics, were included in the study. Results: Amongst 148 study subjects, 21 subjects (14.18%) were diagnosed with ADHD, 73 (49.32%) were diagnosed with inattention, 58 (39.18%) with impulsivity/hyperactivity, 112 (75.67%) with learning problems, 62 (41.89%) with aggression, and 103 (69.58%) with family relation problems. There was statistically significant gender difference in the prevalence of ADHD, with male preponderant; male: female ratio was 3.2:1. Conclusion: The present study revealed that prevalence of ADHD is high amongst adolescents in rural health care setting. It is needed to formulate policies in rural India for effective combating ADHD at early age.
Keywords: ADHD, Hyperactivity, Impulsivity, MHS Conner’s -3 questionnaire
Full Text:
INTRODUCTION
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, disorganization, and/or hyperactivity/impulsivity.[1] Inattention and disorganization entail inability to stay on task, seeming not to listen, and losing materials, at levels that are inconsistent with age or developmental level. Hyperactivity/impulsivity involves over activity, fidgeting, inability to stay seated, intruding into other people’s activities, and inability to wait, symptoms that are excessive for age or developmental level. [2] In childhood, ADHD frequently overlaps with disorders that are often considered to be “externalizing disorders,” such as oppositional defiant disorder and conduct disorder.[3]
ADHD often persists into adulthood, with resultant impairments of social, academic and occupational functioning.First reliable description of ADHD, came from England in early 20th century. Population surveys suggest that ADHD occurs in most cultures in about 5% of children and about 2.5% of adults.[4]Around 60% of ADHD children will carry some of their behavior into adulthood. According to Diagnostic and Statistical Manual for diagnosis of mental disorders (DSMV), ADHD symptoms includes: difficulty staying focused and paying attention, difficulty controlling behavior ,very high levels of activity.[5] WHO identifies adolescence as the period in human growth and development that occurs after childhood and before adulthood, from ages 10 to19 years.[6] It is high time we reach out to 99% of the child population that is being unattended by any agency,114 million children have no facilities even in the urban areas.
There is only a limited source of information regarding the prevalence Of ADHD in the Indian context. The effect of ADHD/behaviour problem occurs at home, school, workplace, relations, physical and educational aspects of life. Currently, early diagnosis of ADHD has gained importance in pursuit of treating them at the earliest, so as to avoid/reduce its complications in various aspects of life.[4]After exhaustive literature search, we could not find any study on prevalence of ADHD in rural health care setting in India. So, the present study is first of its kind to find prevalence of ADHD in rural health care setting in central India.
AIMS AND OBJECTIVES
(i) To study the prevalence of ADHD in adolescents referred for behavioral Problems to rural tertiary health care center. (ii) To identify the gender difference, if any, in the prevalence of ADHD.
(iii) To identify the presence of any co-morbid factors associated with ADHD.
MATERIALS AND METHODS
• Study Design: Cross sectional study (hospital based)
• Place of Study : This study was conducted at NKP Salve Institute of Medical Sciences and Research Centre and Lata Mangeshkar Hospital, Nagpur, (M.S.)
• Period of Study : January 2014 to October 2014 (10months )
• Sample size: A total of 148 participants were enrolled into the present study.
• Study population: Adolescents boys/girls, referred by school or brought by their parents for behavioral problems at Child Guidance Clinic, Department of Pediatrics, NKPSIMS and LMH, Nagpur were included in the study.
• Ethical clearance: Taken prior to start of study from Institutional Ethics Committee (IEC).
• Inclusion Criteria: All school going adolescent boys and girls (age group of 11-16 years) referred by school or brought by parents for behavioral problems.
Exclusion Criteria:
(i) Adolescent whose parents were not willing to sign consent form,
(ii) Adolescents having behavioral issues less than 6 months duration.
DATA COLLECTION:
The informed written consent was taken from the parents/guardian of the adolescent subjects. All subjects were assessed with validated
CONNERS Questionnaire by Multi Health Systems (MHS) and socio-economic status was assessed with modified Kuppuswami scale. A questionnaire developed by MHS- CONNERS-3 was used, which included41 Questions related to following areas: a. Inattention b. Hyperactivity/ Impulsivity c. Learning Problems d. Defiance/ Aggression e. Family Relations • Statistical Analysis and Results: All the data was entered in Microsoft Excel 2013and further Statistical Analysis was done with the help of SPSS statistical software (version 17).
RESULTS
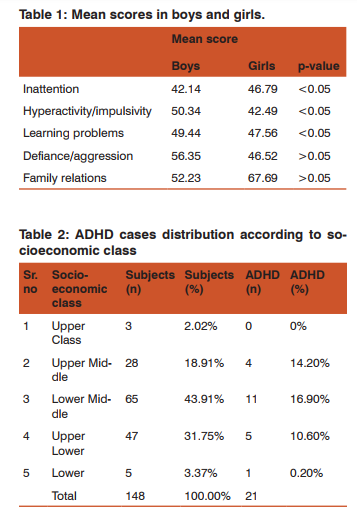
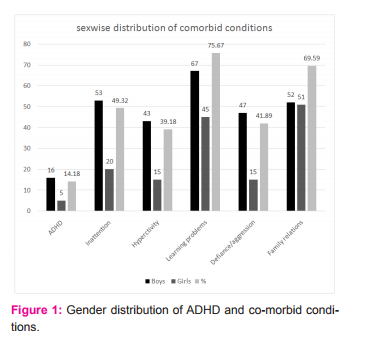
Out of total 148 study participants, 80 were boys and 68 were girls. Amongst study population, 21 participants (14.18%) were diagnosed with ADHD, 73 (49.32%) were diagnosed with inattention, 58 (39.18%) with impulsivity/hyperactivity, 112 (75.67%) with learning problems, 62 (41.89%) with aggression, and 103 (69.58%) with family relation problems. There was significant gender difference in occurrence of ADHD; 16 boys and 5 girls had ADHD, 53 boys and 20 girls had inattention, 43 boys and 15 girls had hyperkinetic/ impulsivity, 67 boys and 45 girls had learning problems, 47 boys and 15 girls had aggression, 52 boys and 51 girls had family relation problems (Figure 1). Amongst MHSConner’s score, mean score in ADHD group was 42.14 for boys and 46.79 for girls, 50.34 for boys and 42.49 for girls in inattention group, 49.44 for boys and 47.56 for girls in learning problem group, 53.35 for boys and 46.53 for girls in defiance/aggression group, 52.23 for boys and 57.69 for girls in family problem group (Table 1).
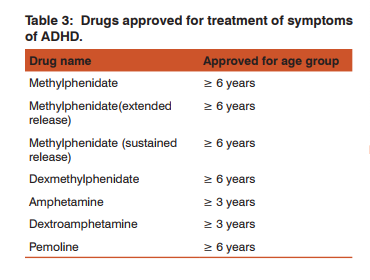
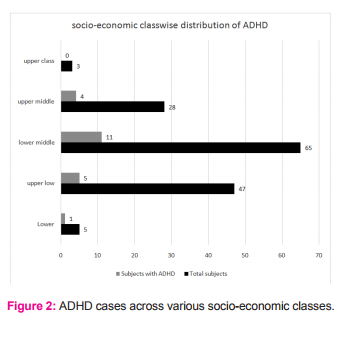
Sex-wise difference in responses were statistically significant in inattention, hyperkinetic/impulsivity, learning difficulty groups (p<0.05). Amongst socio-economic class according to modified Kuppuswami classification, 5 (3.3%) participants were of lower socio-economic class, out of which 1 (0.2%) was diagnosed with ADHD; 47 (31.7%) belonged to upper low class, out of which 5 (10.6%) were diagnosed with ADHD; 65 (43.9%) were of lower middle class, out of which 11 (16.9%) were diagnosed with ADHD; 28 (18.9%) belonged to upper middle class, out of which 4 (14.2%) were diagnosed with ADHD; 3 (2%) belonged to upper socio-economic class and no participant in this class was diagnosed with ADHD (Table 2, Figure 2).
DISCUSSION
Oppositional Defiant Disorder (ODD) is associated with aggression and anxiety/depression symptom. There is a need to regard child with symptom of ADHD, ODD and aggression as a child with heavy genetic loading and predictor of disruptive behaviour disorder. Heidi Aase in their study suggested that children with ADHD have problems with learning, behaviour, particularly related to response location.[7] Problems with learning long behavioural sequences may ultimately lead to deficient development of verbally governed behaviour and self-control. In our study prevalence of ADHD was high (14.18%) amongst students referred to us for behaviour issues. Other studies reported prevalence rates in the range of 3-7%.[8, 9, 10] There was statistically significant gender difference in the prevalence of ADHD, with more prevalence in males; male: female ratio was 3.2:1. This is in accordance with findings of other such study.[8]The learning problems were the most common co-morbid condition followed by family issues associated with ADHD.
ADHD is escorted with many conditions like learning difficulties, ODD, disorder of conduct, bipolar disease, depression, anxiety and Tourette syndrome.[3] Skogan found out that early symptoms of ADHD were linked to parent reported difficulties primarily with inhibition and working memory, suggesting that deficiencies within these two domains characterize early forms of ADHD.[11]It should also be stressed that ADHD like symptoms may be associated with many causes like a brisk change in child’s life like sudden death of parent, undiagnosed temporal lobe seizures, anxiety, depression, hearing difficulties owing to middle ear infections, brain function affection by disorders, learning difficulties, etc. It is also documented that occurrence of ADHD in child is related to smoking and alcohol intake by their mothers during pregnancy.[3] Similarly, high exposure of preschool children to lead is also related with increased peril of ADHD. Weak evidence also suggests that additive sugars also increases the risk of ADHD like behavior.[12]
But this correlation failed to corroborate with findings of other such studies.[13]Traumatic injury to prefrontal cortex is also shown to be associated with ADHD like behavior, but only small chunk of ADHD patients had a history of traumatic brain injury. Also many studies suggest genetic role in causation of ADHD.[14] The prevalence of ADHD in present study was found out to be 14%. In a review of 233 studies on ADHD, conducted worldwide, it was documented that prevalence of ADHD was 5%.[15] In the present study maximum cases of ADHD were found in lower middle class. This was supported by findings in a review study which showed that prevalence of ADHD was maximum in lower socio-economic class as compared to higher class. However, it should also be noted that access to treatment and getting treated is more likely in children of high socio-economic class than that of low socio-economic class.[15]Many treatment options have been tried and tested for treatment of ADHD, but no treatment is fully effective.
Certain evidence based recommendations have been laid down in treating ADHD, according to age group (Figure 3): 1. For ADHD children <6 years age• Methylphenidate is usually safe and effective, • School based interpolations have been found to be useful. 2. For ADHD children ≥6 years age• Evidence of methylphenidate effectiveness upto 14 months treatment • Atomoxetine over a period of 12 months • Guanfacine has evidence of reduction in ADHD symptoms but no evidence till present regarding its long term efficacy. • Non-pharmacological options: inadequate evidence about effectiveness of behavioral or psychosocial intervention alone in reduction of symptoms of ADHD. • Combined therapy: strong evidence in favor of effectiveness of combined therapy of psychostimulants like methylphenidate and behavioral and psycho-socialtherapy in reduction of symptoms of ADHD and ODD exists. These effects are pronounced in school age boys with ADHD. However, psychostimulants have adverse effects which lead to discontinuation of therapy. Atomoxetine is known to cause insomnia, loss of appetite, lethargy, abdominal pain, rise in blood pressure, suicidal tendency. These adverse effects are more common in preschool age children. Mood disturbances and irritability are reported as most common causes of discontinuation of methylphenidate therapy.
Guanfacine is associated with fatigue, sedation, headache, electrocardiographic changes.[4]Prevalence of ADHD is governed by many factors like socio-cultural differences, sex (more prevalent in boys),age (highest prevalence found in age group 5 to 10 years, elementary school children).Some children with ADHD have increased of developing ODD, anti-social attitudes, low self-esteem and depression in adulthood. Also, a minor chunk of them develop bipolar disorders like maniadepression. Amongst those developing anti-social attitudes, about 1/5th develop some sort of substance abuse.[8] Thus, this study helps in estimating amount of ADHD in the area so that necessary screening and intervention policies can be implemented to diagnose and treat ADHD early, in order to avoid aftermaths.
CONCLUSION The present study carries weightage, since no such study has been done in rural health care setting in India, given that it has been documented in some foreign country studies that highest prevalence of ADHD is found in low socio-economic class. Such studies should be conducted elsewhere in the country, so that findings of present study can be compared, in view of projecting exact figures on prevalence of ADHD, to formulate policies for effectively combating ADHD at early age.
Conflicts of interest/s: None declared. Source of funding: None. Ethical clearance: Taken prior to the start of study from Institutional Ethics Committee (IEC).
ACKNOWLEDGEMENTS Authors acknowledge the immense help received from scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/ editors/ publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. The authors wish to acknowledge the valuable support and help offered by Dr. P. Singh, who is clinical psychologist.
References:
1. Identifying and treating Attention Deficit Hyperkinetic Disorder: A resource for learning for school and home, ED Pubs, Washington DC., 2006.
2. Teaching children with Attention Deficit Hyperkinetic Disorder: Instructional strategies and practices, ED Pubs, Washington DC., 2008.
3. National Institute of Mental Health: Attention Deficit Hyperkinetic Disorder. Bethesda (MD), US Department of Health and Human Services, 2004. Available from http://www.nimh.nih. gov/publicat/index.cfm. [Last assessed on Dec. 28, 2015].
4. Attention Deficit Hyperkinetic Disorder in children and adolescents. Available from http://www.effectivehealthcare.ahrq.gov/ ehc/products/191/1149/adhd_clin_fin_to_post.pdf. [Last assessed on Jan 4, 2016].
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-V). Washington DC, American Psychiatric Association, 2013.
6. Attention Deficit Hyperkinetic Disorderin adolescents. Available from http://www.who.int/maternal_child_adolescent/topics/ adolescence/dev/en [last assessed on Dec 29 2015].
7. Heidi Aase and Terje Sagvolden.Moment-to-moment dynamics of ADHD behaviour, Behavioral and Brain Functions 2005, 1:12 doi: 10.1186/1744-9081-1-12, Published: 1 August 2005, Available from http://www.behavioralandbrainfunctions.com/content/1/1/12/abstract
8. Barkley RA, Murphy KR. Attention Deficit Hyperkinetic Disorder: A clinical workbook. 2006, 3rd ed Guilford Publications, New York, 1-10.
9. Visser SN, Zablotsky B, Holbrook JR, et al. Diagnostic experiences of children with attention-deficit/hyperactivity disorder. National health statistics reports; no 81. Hyattsville, MD: National Center for Health Statistics. 2015.
10. Hinshaw SP, Arnold LE. Attention-deficit hyperactivity disorder, multimodal treatment, and longitudinal outcome: evidence, paradox, and challenge. WIREs Cogn Sci 2015, 6:39–52.
11. Skogan AH, Zeiner P. Parent ratings of executive function in young preschool children with symptoms of attentiondeficit/-hyperactivity disorder, Behavioral and Brain Functions 2015, 11:16 doi:10.1186/s12993-015-0060- 1.Available from http://www.behavioralandbrainfunctions.com/ content/11/1/16.
12. Hoover DW, Milich R. Effects of sugar ingestion expectancies on mother-child interaction. Journal of Abnormal Child Psychology, 1994; 22; 501-515.
13. Consensus Development Panel. Defined Diets and Childhood Hyperactivity. National Institutes of Health Consensus Development Conference Summary, Volume 4, Number 3, 1982.
14. Faraone SV, Biederman J. Neurobiology of Attention- Deficit Hyperactivity Disorder. Biological Psychiatry, 1998; 44: 951- 958.
15. DSM-IV-TR workgroup. The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License