IJCRR - 8(8), April, 2016
Pages: 23-26
Date of Publication: 20-Apr-2016
Print Article
Download XML Download PDF
ESTIMATION OF SERUM LIPID LEVELS IN CHRONIC PERIODONTITIS PATIENTS: A CASE-CONTROL STUDY
Author: Deepu Mathews Panickal, Prashanth Evuru, Jeethu John Jerry, Little Mahendra, Sandhya Cherukuri, Jaideep Mahendra
Category: Healthcare
Abstract:Aims and Objectives: Hyperlipidemia refers to abnormally elevated levels of lipids and/or lipoproteins in the blood. Elevated serum cholesterol is a modifiable risk factor that is associated with a cardiovascular disease (CVD) with an estimated 4.4 million deaths each year. A positive association between serum triglyceride concentration and risk of coronary heart disease has been observed in many case-control studies. Infection such as periodontitis causes bacteremia and/or endotoxemia producing a cytokine cascade that leads to increased levels of serum pro-inflammatory cytokines. These molecules promote enhanced lipogenesis, increased lipolysis, and reduced lipid clearance resulting in hyperlipidemia. Hence the aim of the study is to estimate the serum lipid levels in chronic periodontitis patients. Materials and Methods: 100 subjects were screened for the study and were grouped as experimental (50 subjects with chronic periodontitis) and control (50 systemically healthy subjects). To assess the periodontal condition all the subjects underwent the estimation of Clinical Attachment Loss (CAL). Blood samples were obtained and analyzed for serum lipid levels of Low Density Lipoprotein (LDL), High Density Lipoprotein (HDL), Triglyceride (TG) and Total Cholesterol (CHOL). Results: The mean values of LDL, HDL, TG and CHOL were significantly higher in chronic periodontitis subjects than healthy controls. Conclusion: The study concludes that patients with chronic periodontitis exhibited higher serum lipid levels. Hence these patients may be at a higher risk for further coronary events.
Keywords: Chronic Periodontitis, Low Density Lipoprotein, High Density Lipoprotein, Triglyceride, Total Cholesterol
Full Text:
INTRODUCTION Periodontitis is a chronic inflammatory disease primarily caused by gram – negative anaerobic microorganisms that lead to destruction of periodontal tissues and alveolar bone. [1] These microorganisms, particularly Porphyromonas gingivalis produce endotoxins in the form of lipopolysaccharides (LPS) that are instrumental in generating a host-mediated immune response. [2] Hyperlipidemia refers to increased levels of any or all lipids and/or lipoproteins in the blood.
It is well known that a causal relationship exists between serum lipid levels and systemic health, particularly cardiovascular disease, diabetes, tissue repair capacity, immune cell function, and serum levels of pro-inflammatory cytokines. It is hypothesized that periodontitis causes bacteremia and/or endotoxemia producing a cytokine cascade that leads to increased levels of proinflammatory cytokines. These molecules promote enhanced lipogenesis, increased lipolysis and reduced lipid clearance. [3] Though various studies have shown association with periodontitis and hyperlipidemia, however the results are still conflicting. Hence the present study was aimed at estimating the serum lipid levels of LDL, HDL, TG and CHOL in chronic periodontitis patients and compared with the healthy subjects.
MATERIALS AND METHODS One hundred and fifty subjects were recruited from the outpatient pool of Department of Periodontology, Vinayaka Dental College, with approval from ethical review board [VMSDC/IEC/019], following the Declarations of Helsinki for the study. [4] Twenty-five subjects did not meet the inclusion criteria and twenty-five subjects declined to participate. Finally, hundred subjects met the eligibility criteria and were selected for the present investigation. The selected subjects were informed about the study, and informed consent was obtained from them. Periodontal status was assessed by measuring the CAL.
They were then categorized as the experimental and control group with 50 subjects in each group based on the following inclusion and exclusion criteria. (Figure-1) Inclusion criteria of the experimental group included subjects between 25 to 70 years of age with generalized chronic periodontitis having ≥ 10 natural teeth. [5] Subjects with history of systemic diseases that affect lipid metabolism, history of drug treatment for hyperlipidemia, previous periodontal treatment and pregnancy were excluded from the study. Control group included subjects with systemically healthy and intact periodontium. Age and Body Mass Index (BMI) was calculated as body weight (kg) divided by height (m2 ).
MEASUREMENT OF CLINICAL ATTACHMENT LOSS It is the distance between base of the pocket and a fixed point on the crown, such as cemento-enamel junction. In this study, Clinical attachment loss (CAL) is measured with a periodontal probe from the cemento-enamel junction to the base of the pocket (mm).
SAMPLE COLLECTION COLLECTION OF BLOOD After clinical examination approximately 3cc of blood was drawn from the antecubital vein of each subject and analyzed for serum lipid levels of Low Density Lipoprotein (LDL), High Density Lipoprotein (HDL), Triglyceride (TG) and Total Cholesterol (CHOL) using Lipid panel test. Lipid panel test is a panel of blood tests that serves as an initial broad medical screening tool fort for quantitative determination of High-Density Lipoprotein, Low- Density Lipoprotein, Total Cholesterol and Triglycerides. Measuring a Lipid Panel/Cholesterol is recommended by NCEP (National Cholesterol Education Program) every five years in healthy adults and every year in high risk patients. [6] STATISTICAL ANALYSIS Data was analyzed using IBM SPSS 16 statistical software. Statistical comparisons were performed using student’s t-test for lipid levels between the groups. p value of <0.05 was considered statistically significant.
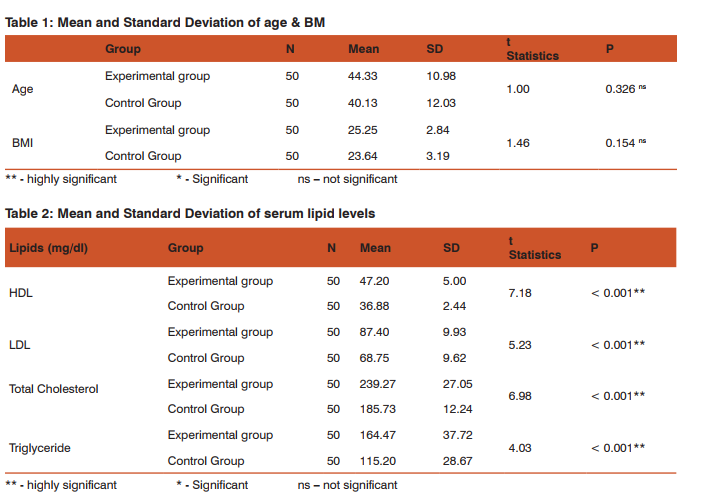
RESULTS Demographic Variables The mean age and BMI of the experimental and control group were similar and hence were non-significant. (Table-1) Serum lipid levels in chronic periodontitis and healthy subjects Table 2 shows the distribution of mean and Standard Deviation of the HDL, LDL, CHOL and TG in experimental and control group. The Independent t test is used to find whether the difference between the mean score level of HDL, LDL, CHOL and TG among control and experimental group. The analysis showed that the p value for HDL, LDL, CHOL and TG was less than 0.01 which was highly significant between both the groups.
DISCUSSION It is known that hyperlipidemia is a risk factor for cardiovascular disease. Association between periodontitis and cardiovascular disease can be due to the elevated levels of plasma lipids. In periodontal disease, increase in cytokine secretion results in fat metabolism and hyperlipidemia. [7,8] In our study the mean age and BMI was more or less the same in both experimental and control group, hence statistically non significant. Hamissi et al, carried out a similar study on serum lipid profile of periodontitis subjects and compared them with the healthy controls in which the case and control groups were matched by, age, gender, diet, weight, height, health condition and number of teeth. [9]
According to the results of our study, significantly higher levels of serum High Density Lipoprotein (HDL), Low Density Lipoprotein (LDL), Total Cholesterol (CHOL) and Triglyceride (TG) were observed in subjects with chronic periodontitis when compared with the healthy controls. (Table-2) This is in accordance with the study by Lösche et al, who estimated higher levels of plasma lipids in 39 subjects with moderate periodontal disease when compared with the healthy subjects. [10] Cutler et al, found a significant relationship between periodontitis, hyperlipidemia, and serum antibodies against P. gingivalis LPS and also indicated that elevated triglycerides are able to modulate interleukin (IL)- 1β production by PMNs stimulated by P. gingivalis LPS. [3] Katz et al, investigated the association between hypercholesterolemia, cardiovascular disease and severe periodontal disease in 1094 subjects. He concluded that the generation of higher cholesterol blood levels is a possible link between chronic periodontal inflammation and atherosclerosis. [11] A recent case-control study by Zhou et al, demonstrated the elevated levels of lipoprotein-associated phospholipase A2 and lipid profile markers in subjects with chronic periodontitis. [12]
Periodontitis is a microbial infection caused by gram-negative bacteria. Acute infections are known to interfere with lipid metabolism, and elevation of plasma triglycerides has been observed, especially in infection with gram-negative bacteria. [13] These changes are known to be mediated by cytokines such as IL-1 or TNF which is produced in the inflamed periodontal tissues. [14,15] These biological signaling molecules from local inflammation into the circulation have multiple physiological effects promoting enhanced lipogenesis, increased lipolysis and reduced lipid clearance.
CONCLUSION Higher levels of HDL, LDL, CHOL and TG were expressed in chronic periodontitis subjects than the controls. Hence the study states that subjects with periodontal disease having high serum lipid levels are at a higher risk for atherosclerosis than the healthy subjects. Further, longitudinal studies are needed to explore the role of the inflammatory mediators on the serum lipid levels as the age progresses in order to visualize the risk of periodontitis on CVD events.
ACKNOWLEDGEMENT The authors acknowledge Dr. Issac Emerson for assisting in the molecular analysis carried out in the study. CONFLICT OF RESULT: None declared
References:
1. Socransky SS, Haffajee AD. The bacterial etiology and progression of destructive periodontal disease: current concepts. J Periodontol 1992; 63: 322-31.
2. Offenbacher S. Periodontal diseases: pathogenesis. Ann Periodontol 1996; 1: 821-78.
3. Cutler CW, Shinedeling EA, Nunn M. Association between periodontitis and hyperlipidemia: Cause or effect? J Periodontol 1999; 70: 1429–34.
4. World Medical Association Declaration of Helsinky. Ethical Principles for Medical Research Involving Human Subjects. 18th WMA General Assembly, Helsinky; 1964.
5. Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol 1999; 4: 1-6.
6. Rick Daniels. Delmar’s guide to laboratory and diagnostic tests. 3rd ed. Cengage Publishers. p. 495-500.
7. Lowe GD. pathogenesis of cardiovascular disease. Ann Periodontol 1998; 3(2): 12–5.
8. Sridhar R, Byakod G, Pudakalkatti P, Patil R. A study to evaluate the relationship between periodontitis, cardiovascular disease and serum lipid levels. Int J Dent Hyg 2009; 7(2): 144–50.
9. Hamissi J, Shahsavarani MT, Hamissi H. A Comparison of Serum Lipid Profile between Periodontitis Patients and Healthy Individuals. Iran Red Crescent Med J 2011; 13(4): 283-4.
10. Lösche W, Karapetow F, Pohl A, Pohl C, Kocher T. Plasma lipid and blood glucose levels in patients with destructive periodontal disease. J Clin Periodontol 2000; 27(8): 537-41.
11. Katz J, Chaushu G, Sharabi Y. On the association between hypercholesterolemia, cardiovascular disease and severe periodontal disease. J Clin Periodontol 2001; 28(9): 865-8.
12. Zhou SY, Xiao WM, Ouyang XY. Lipoprotein-associated phospholipase A2 and serum lipid levels in subjects with chronic periodontitis and hyperlipidemia. Chin J Dent Res 2012; 15(1): 25-9.
13. Alvares C, Ramos A. Lipids, Lipoproteins and apoproteins in serum during infection. Clin Chem 1986; 32: 142-5.
14. Beck JD, Offenbacher S, Williams R, Gibbs P, Garcia R. Periodontitis: a risk factor for coronary heart disease? Ann Periodontol 1998; 3: 127-41.
15. Valtonen VV. Infection as a risk factor for infarction and atherosclerosis. Ann Med 1991; 23 (5): 539-43.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License