IJCRR - 12(18), September, 2020
Pages: 149-153
Date of Publication: 22-Sep-2020
Print Article
Download XML Download PDF
Fungal Infection in the Oral Cavity: A Review
Author: Smarita Lenka, Santosh Kumar Swain, Ruchi Bhuyan, Mahesh Chandra Sahu
Category: Healthcare
Abstract:Fungal infection in the oral cavity is a completely microbes-oriented disease most probably caused due to biofilm formation on the floor of the mouth and its surrounding. Most of the studies revealed that Candida and Asparigellus spp. are frequently isolated fungus. Smoking, alcohol consumption, high intake of carbohydrate diet, loss of salivary function and immunosuppression are colonizing factors and predisposing factors for fungal infection in the oral cavity and may lead to the chronic stage at its severity. Oral candidiasis is an opportunistic infection of the oral cavity and the incidence depends on the age of the patient and certain predisposing factors. There are three varieties of oral candidiasis such as acute candidiasis, chronic candidiasis and angular cheilitis.CD4 T lymphocyte and CD8 T lymphocyte provides primary as well as secondary immunity towards oral fungal infection. Denture wearers, HIV patients, children and elders are mostly infected by an oral fungal infection. This systematic review tends to focus on etiological factor, salivary action, and immunity behind fungal infection in the oral cavity with management and treatment of oral fungal infection.
Keywords: Oral cavity, Fungal infection, Fungal biofilm, Candida spp, Antifungal agent
Full Text:
Introduction
Fungal infection in oral cavity emerges due to both chemical as well as biological reasons and stands before us as a worldwide problem varies according to age groups but seems to be very common among old ages particularly in those who do not take care of their mouth. Fungal infection arises in the oral cavity due to the colonizing character of microbes, especially by food debris. The biofilm formation through pathogenic organisms alternately converted into white fungal patches. Initially, the biofilm formed in the oral cavity promotes contamination and attracts fungal infection. Systemic oral fungal infection is seen approximately 50% to 60% of cases that depend upon dentures in old age2,3. Persons having diabetes mellitus, high carbohydrate on their diet and smoking like habits could disturb the normal microflora of the oral cavity and that can initiate fungal infection4,5. Patients suffering from fungal infection in oral cavity increases eventually due to many reasons and arise the number of difficulties particularly for immunocompromised patients such as those receiving chemotherapy during cancer treatment and fighting with human immunodeficiency virus (HIV)2. Those having poor immunologic response this fungal contamination remains a significant problem throughout their life6. Fungal infection frequently occurs those have an immunosuppressive illness or going through organ transplant surgery7. The oral fungal infection seems to be very opportunistic in HIV patients that are more than 90% people showing developmental oral fungal infection8
Methods for Literature search
For searching the published articles, we conducted an electronic search of the Google Scholar, Scopus, Medline, Scopus and PubMed databases. The search term in the database included oral cavity, fungal infections, Candida infection and oral thrush. The abstracts of the published articles are identified by this search method and other articles identified manually from the citations. This review article reviews the oral cavity fungal infection. This review article sets out a framework on which more prospective trials can be formulated and support as a spur for further research in this commonly observed clinical entity where not many studies are done.
Etiological factors
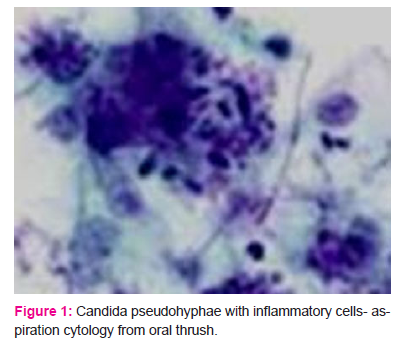
Factors that are responsible for oral fungal infection mainly arise due to our unconsciousness about oral health care. Acid formation in the oral cavity occurs due to both smoking and alcohol consumption and high intake of sugar and carbohydrate in the food. The high rate of drinking alcohol can disrupt the oral microflora and can persist acetaldehyde formation that leads to adherence of oral fungal colonisation 9,10. Some of the other challenging predisposing factors that induce oral fungal infection are hormonal disorders, epithelial changes, physiological disorders, poor oral hygiene, endocrine disorders, immunologic disorders, poorly fitting dentures and empirical drug therapy11. The most common colonising isolated fungi from the oral cavity is Candida albicans(Fig.1) 5,12,13, derived from Latin word candid means white.
It is a spore-forming fungus that remains harmless until there are no disturbances occurred in host microflora balance of oral cavity 14. With the addition to candida spp, Aspergillus spp, Fusarium spp., and Acremonium spp. are some of the isolated contaminated factors causing fungal infection in the oral cavity. Somehow infections also caused by non-Candida and non-Cryptococcus isolates and infections caused by Trichosporon spp., Malassezia spp., and Rhodotorula spp. are mainly notable but in many cases, it is observed that Candida and Cryptococcus are factors that initiate fungal colonisation specifically candida spp. When the oral cavity comes in contact with several microbes especially spore containing fungal pathogens forms a biofilm on the upper part of epithelial cell and create the environment for the survival of them15. Except for C. albicans, C. glabrata, C. lusitaniae and C. guilliermondii. C. albicans, C. glabrata, C. parapsilosis, C. krusei, are some non-albicans found in oral cavity causing colonisation but less life threatening than C.albicans6,8.
Etiology of fungus
According to mycological study fungi are found in both form; unicelluar and multicellular depending on their stage of life style. They cannot make their own food as they are heterotrophs hence they obtain their nutrients from other source using their pseudohyphae, along with network formation of hyphae called mycelium. When nutritional, environmental as well as immunological variation occurs, a saprophytic fungus associated with oral cavity reproduces and giving rise to more compact colonies of new fungus forming a row of elongated cells found in white patches and lesions.
Role of saliva in fungal infection
The oral cavity is a wide field for the variety of microorganisms and acts as a host to survive on it. It needs a natural microflora for normal development and physiology16. The oral cavity is lined by mucosal epithelial cells and continuously filled with saliva secreted by various salivary glands and activate the mechanism of many beneficial microbes. Any disturbances occur in the secretion or function of saliva, epithelial cell damage can lead to making physiological differences in the oral cavity. Some certain microbes can affect or change the normal microflora. C. Albicans is a mutualistic fungus which can form fungal colonisation in the oral cavity causing oropharyngeal candidacies. In other words, we can say that saliva has a defence mechanism which stands as a barrier against the fungal attack17,10. Because of the flushing action of saliva, microbial infection in the oral cavity can be diluted and appears to show minimum emergence but fungi have that capacity to multiply under these types of adverse circumstances and reflects infection18. It brings nutrients, peptides, and partially dissolved carbohydrates and delivers to oral biofilm. Addition to this it helps in lubrication for digestion, temperature regulation, including host defence by saliva flow19. Immunoglobulin action of saliva can identify protective function against fungal pathogen concerning innate immunity and contribute to first-line oral defence20.
The immune system of the oral cavity
The innate immunity of our body always tends to ready for fighting any adverse condition during necessity but in case of oral fungal infection mouth act as an entry point of the outer harmful components. In the oral cavity whenever there becomes an interaction between host immunity and the foreign pathogen that leads to either mutualism and confirms salivary defend mechanism against that pathogen or break the epithelial barrier 10. In the epithelial cells, there is a polysaccharide receptor named Toll-like receptor (TLR4) expresses the immune recognition against pathogenic microbes and by the action of macrophages and dendritic cell it prevents the colonisation of fungal flora like C.albicans21,22. The cell-mediated immune system and humoral immunity play a crucial role in protecting oral mucosa from fungal colonisation8. Also with the epithelial barrier, primary immunity is provided by type 1 CD4 T lymphocyte that is activated by the help of interleukin (IL)-4, IL-6, and IL-12, secondary immunity provided by CD8T lymphocyte through several immunological mechanisms6 using T cell receptor (TCR) on their cell surface where MHC I or MHC II helps to display fungal pathogen 23. Activated T-cells produces lymphokines that regulate the functions of macrophages and other leukocytes like interferon-gamma (IFN-γ), which is the only lymphokine that helps to enhance the microbicidal action of macrophages. T lymphocyte also activates TNF (tumour necrosis factor) synthesis by them. In the presence of suboptimal levels of IFN-γ, fungus killing by neutrophils is developed by tumor necrosis factor-α (TNF-α)24,25. Whenever the CD4 T lymphocyte count fallen down (approximately 200 cells/mm3) recurrence rate of the disease could be possible26. Reduction of antibodies such as IgA, IgM and IgG defects in lymphocyte transformation and stimulate most severe types of oral fungal infection27. There is a confusing relationship between inflammation and immunity that what comes first, whether the change in the integrity of the biofilm or the host immune response19.
Clinical presentation of oral fungal infection
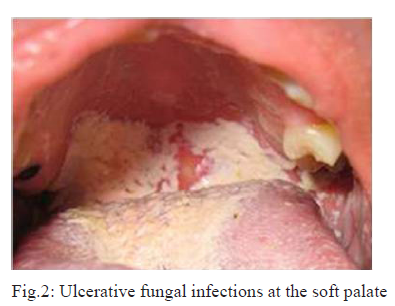
The primary stage of oral fungal infection is initiated by the primary colonisers found in the surface of the oral cavity; later on, that is proliferated into superficial colonisation with a large number of migratory fungal colonisers forming a multi-layered biofilm. According to the differential environmental mechanism of the oral cavity such as temperature, atmospheric conditions, pH, salinity, redox potential, and liquid activity from saliva can alter the microbial composition and trigger the shelter to fungal biofilm19. Artificial equipment like dentures can restrict the arrival of oxygen and flow of saliva to the appropriate tissue area; that’s why low PH and scarcity of oxygen level promote the storage of dense fungal film on the floor of the oral cavity. The microbial film deposited on the surface of the oral cavity nothing but infected scales of epithelial cells with fungal hyphae looks like curd deposits with superficial patches8. Oral fungal infection often remains asymptomatic mostly at the initial stage, but periodically symptoms have seen like irritation in the mouth, burning during eating, difficult to talk and alteration in sense of tasting. Candida albicans remain all-time common isolated microorganism in oral fungal infection. Oral candidiasis classified into primary and secondary oral candidiasis. Primary candidiasis affects oral and perioral tissue only but during secondary candidiasis, superficial candida association may lead to keratinised lesions 28,29. Deep fungal infection in the oral cavity with high efficiency may alter to the ulcerative lesion(Fig.2)30.
Diagnostic method
Oral fungal infection can be clinically diagnosed by biopsy and there is another way that is microbiological diagnosis through oral sample culture on laboratory8,31. Like another disease, a fungal infection in the oral cavity can also be diagnosed clinically and pathologically. About 90% region of the oral cavity can get infected including the tongue, lip surface and complete floor of mouth with curd-like white patches. Mostly in older adults when excessive deposition of plaque occurred on the oral cavity then mixed white and red lesions are seen with heavily keratinised surface32. The clinical diagnosis followed by biopsy can reveal hyphae or pseudohyphae of identified fungi. The cytological study can reveal microscopic evaluation and another way that is sample culture reveals the actual and exact process of diagnosis of fungal era28. Diagnosis of oral fungal infection can be carried out by morphologically, biochemically, immunologically and genetically. Identification, as well as isolation of fungal infection in oral cavity, have several approaches of diagnostic method like direct microscopy of smear, staining and microbiological culture. New advanced optical devices allow the direct microscopic examination to clinicians. Cytological identification is made possible through direct microscopy by simply transformation of the sample in a glass slide collected from the infected site. Potassium hydroxide, gram stain and periodic acid–Schiff (PAS) are three diagnostic agents help to clear background, making fungi clearly visible and easily identified 29,33, 34. In the case of the failing procedure to cytological smear identification, Sabouraud’s dextrose agar (SDA) is recommended as media for fungal culture. After an incubation period of 24-28 hours at approximately 370C, fungal colonies appeared on the plate containing SDA5. There is another staining diagnostic process named Gridley’s or Grocott’s methenamine silver (GMS) stains are ideal for confirming fungal elements in tissues, deeply dying from those stains. In further techniques, with the availability of chronic or periodic acid, the hydroxyl groups of complex polysaccharides of the yeast cell wall are oxidized to aldehydes35. The genetical diagnostic method involves enzyme-linked immunosorbent assay(ELISA) and polymerase chain reaction PCR in which the strain persistence has been investigated by DNA fingerprinting during chronic or repeated infection and clear all hesitation to follow antifungal therapy, microevolution in infecting populations, and the cause of oral fungal infection31,36.
Management and treatment
Disease and host immunity are interlinked with some agents that help to keep balance on the physiology of the human body that are vitamins and nutritional supplement. Therefore, deficiency states of iron, folic acid, vitamins B12, vitamin C and vitamin A; able to weaken our immune system. As saliva has defended mechanism, salivary gland function and salivary hydration testing should be performed. Dentures should be avoided, if not, should clean those things properly soaking with white vinegar. Nutritional factors should be implemented on the treatment of fungal infection with the prohibition of carbohydrate-rich diet5. Smoking, alcohol and tobacco consumption should be avoided as C.albicans come in the very active form with cigarette smoke getting it as a nutritional factor and cigarette smoke contain aromatic hydrocarbon that can convert the enzyme system of candida species to carcinogen37. Some study reveals that fluconazole and amphotericin B remain sensitive toward most of the fungal isolates in antifungal susceptibility test and very few were resistant to them6.
An oral fungal infection could be managed by following the required guidelines like:
-
Diagnosis by accurate medical and dental records, clinical demonstration verified with morphological, biochemical, immunological and genetical laboratory tests.
-
Predisposing factors that are responsible for the initiation of oral fungal infection should be rectified wherever required.
-
Maintaining good oral cavity hygiene and oral prostheses like dentures.
-
Adoption of antifungal therapy based on the intensity of the infection and susceptibility of the fungal species.
-
For proper maintenance of oral cavity natural remedies like grapefruit seed extract; garlic; tea tree oil, clove oil can be used as pre-treatment for better oral health.
-
Cleaning of mouth with water or mouthwash after every meal and use of an inhaler that contains corticosteroids.38
Conclusion
Oral fungal infection reveals many microbes including Candida and Aspergillus spp. mostly. Misbalance in host immunity and saliva function plays a crucial role in the induction of fungal suspension on the oral cavity. Immunogenic misbalance of host allows microbes to be settled. Long term deposition of fungal biofilm may lead to chronic ulceration and could be life-threatening. Self-awareness about oral hygiene and regular cleansing can control the deposition of food debris and restrict the risk of oral fungal infection. Avoiding smoking, alcohol, tobacco and by adding healthy nutritional factor in the diet could enhance the innate immunity for a better host response towards an oral fungal infection. Now treatment with empirical therapy is at high risk because many antifungals become resistant to isolated microbes. Medication should be proper following antifungal susceptibility test. Clinicians have to treat timely using proper diagnostic techniques and medication.
References:
-
Damasceno JL, Santos RA, Barbosa AH, Casemiro LA, Pires RH, Martins CH. Risk of Fungal Infection to Dental Patients. The Scientific World Journal. 2017;2017.
-
Gleiznys A, Zdanavi?ien? E, Žilinskas J. Candida albicans importance to denture wearers. A literature review. Stomatologija. 2015;17(2):54-66.
-
Darwazeh AM, Al-Refai S, Al-Mojaiwel S. Isolation of Candida species from the oral cavity and fingertips of complete denture wearers. The Journal of prosthetic dentistry. 2001;86(4):420-3.
-
Akpan A, Morgan R. Oral candidiasis. Postgraduate medical journal. 2002 ;78(922):455-9.
-
Farah CS, Lynch N, McCullough MJ. Oral fungal infections: an update for the general practitioner. Australian dental journal. 2010;55:48-54.
-
Junqueira JC, Vilela SF, Rossoni RD, Barbosa JO, Costa AC, Rasteiro V, Suleiman JM, Jorge AO. Oral colonization by yeasts in HIV-positive patients in Brazil. Revista do Instituto de Medicina Tropical de Sao Paulo. 2012;54(1):17-24.
-
Menezes EA, Monteiro MN, Parente TM, Cunha FA, Augusto KL, Freire CC. Frequency and enzymatic activity of Candida albicans isolated from the oral cavity of HIV-positive patients at Fortaleza, Ceará. Jornal Brasileiro de Patologia e Medicina Laboratorial. 2006;42(4):253-6..
-
Aggarwal N, Bhateja S, Arora G, Yasmin T. Candidiasis-The most common fungal infection of the oral cavity. Biomedical Journal of Scientific and Technical Research. 2018;1-5.
-
Homann N, Tillonen J, Meurman JH, Rintama?ki H, Lindqvist C, Rautio M, Jousimies-Somer H, Salaspuro M. Increased salivary acetaldehyde levels in heavy drinkers and smokers: a microbiological approach to oral cavity cancer. Carcinogenesis. 2000;21(4):663-8.
-
Moyes DL, Naglik JR. Mucosal immunity and Candida albicans infection. Clinical and Developmental Immunology. 2011;2011.
-
Garcia-Cuesta C, Sarrion-Pérez MG, Bagán JV. Current treatment of oral candidiasis: A literature review. Journal of Clinical and Experimental dentistry. 2014;6(5):e576
-
Charyulu NR, Jose J, Shetty V. Design and characterization of a mucoadhesive buccal patch containing antifungal agent for oral candidiasis. Int J Pharm Phytopharmacol Res. 2014;3(3):245-9.
-
Diaz PI, Strausbaugh LD, Dongari-Bagtzoglou A. Fungal-bacterial interactions and their relevance to oral health: linking the clinic and the bench. Frontiers in cellular and infection microbiology. 2014;4:101..
-
Byadarahally Raju S, Rajappa S. Isolation and identification of Candida from the oral cavity. ISRN Dentistry. 2011;2011..
-
Damasceno JL, Santos RA, Barbosa AH, Casemiro LA, Pires RH, Martins CH. Risk of Fungal Infection to Dental Patients. The Scientific World Journal. 2017 Jan 1;2017.
-
Sanjaya PR, Gokul S, Patil BG, Raju R. Candida in oral pre-cancer and oral cancer. Medical hypotheses. 2011;77(6):1125-8..
-
Salvatori O, Puri S, Tati S, Edgerton M. Innate immunity and saliva in Candida albicans–mediated oral diseases. Journal of dental research. 2016;95(4):365-71.
-
Samaranayake LP, Ferguson MM. Delivery of antifungal agents to the oral cavity. Advanced drug delivery reviews. 1994;13(1-2):161-79.
-
Avila M, Ojcius DM, Yilmaz Ö. The oral microbiota: living with a permanent guest. DNA and cell biology. 2009;28(8):405-11.
-
Amerongen AN, Veerman EC. Saliva–the defender of the oral cavity. Oral diseases. 2002;8(1):12-22.
-
Bäckhed F, Hornef M. Toll-like receptor 4-mediated signalling by epithelial surfaces: necessity or threat?. Microbes and Infection. 2003;5(11):951-9..
-
Hornef MW, Bogdan C. The role of epithelial Toll-like receptor expression in host defence and microbial tolerance. Journal of endotoxin research. 2005 Apr;11(2):124-8.
-
Richardson JP, Moyes DL. Adaptive immune responses to Candida albicans infection. Virulence. 2015;6(4):327-37.
-
Dineshshankar J, Sivakumar M, Karthikeyan M, Udayakumar P, Shanmugam KT, Kesavan G. Immunology of oral candidiasis. Journal of Pharmacy & Bioallied Sciences. 2014;6(Suppl 1): S9.
-
Scully C, Ei-Kabir M, Samaranayake LP. Candida and oral candidosis: a review. Critical Reviews in Oral Biology & Medicine. 1994;5(2):125-57.
-
Shinobu-Mesquita CS, Bertoni TA, Guilhermetti E, Svidzinski TI. Antifungal activity of the extract of Curcuma zedoaria against yeasts of the genus Candida isolated from the oral cavity of patients infected with the human immunodeficiency virus. Rev. Bras. Farmacogn. 2011;21(1):128-32.
-
Netea MG, Maródi L. Innate immune mechanisms for recognition and uptake of Candida species. Trends in immunology. 2010;31(9):346-53.
-
Sherman RG, Prusinski L, Ravenel MC, Joralmon RA. Oral candidosis. Quintessence international. 2002;33(7).
-
Muzyka BC, Epifanio RN. Update on oral fungal infections. Dental Clinics. 2013;57(4):561-81.
-
DeRossi SS, Ciarrocca KN, Alawi F. Oral ulcerations in a patient with severe asthma. The Journal of the American Dental Association. 2010 Jan 1;141(1):47-51.
-
Coronado-Castellote L, Jiménez-Soriano Y. Clinical and microbiological diagnosis of oral candidiasis. Journal of clinical and experimental dentistry. 2013;5(5):279.
-
Bhattacharyya I, Chehal HK, Islam MN. Common Lesions in Oral Pathology for the General Dentist. InThe Dental Reference Manual 2017 (pp. 227-289). Springer, Cham.
-
Marty M, Bourrat E, Vaysse F, Bonner M, Bailleul-Forestier I. Direct microscopy: a useful tool to diagnose oral candidiasis in children and adolescents. Mycopathologia. 2015;180(5-6):373-7.
-
Yao Y, Shi L, Zhang C, Sun H, Wu L. Application of fungal fluorescent staining in oral candidiasis: a diagnostic analysis of 228 specimens. BMC microbiology. 2019;19(1):96.
-
Sitheeque MA, Samaranayake LP. Chronic hyperplastic candidosis/candidiasis (candidal leukoplakia). Critical Reviews in Oral Biology & Medicine. 2003;14(4):253-67.
-
Bartie KL, Williams DW, Wilson MJ, Potts AJ, Lewis MA. PCR fingerprinting of Candida albicans associated with chronic hyperplastic candidosis and other oral conditions. Journal of clinical microbiology. 2001;39(11):4066-75.
-
Soysa NS, Ellepola AN. The impact of cigarette/tobacco smoking on oral candidosis: an overview. Oral diseases. 2005;11(5):268-73.
-
Patil S, Rao RS, Majumdar B, Anil S. Clinical appearance of oral Candida infection and therapeutic strategies. Frontiers in microbiology. 2015;6:1391.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License