IJCRR - 12(18), September, 2020
Pages: 95-99
Date of Publication: 22-Sep-2020
Print Article
Download XML Download PDF
Intramedullary Interlocked Nail with Poller Screw Guidance for management of Extra-articular Proximal Tibial Fractures: A Prospective Study
Author: Avinash Kumar, Kishore K. Panda, Anurag Singh, Anand Kumar Singh
Category: Healthcare
Abstract:Introduction: proximal one-third of tibial fractures are fairly commonly seen nowadays. Their geometry makes them prone to angular deformities. The use of a Poller or Blocking screw along with an intramedullary nail helps in avoiding these angular deformities and malunion. In this study, we aim to evaluate the functional and radiological outcomes of proximal one-third fractures of tibia managed with an intramedullary nail and a Poller screw. Material and Method: This study was conducted between 2017-2019 and a total of 14 patients were operated and followed up. Their demographic, pre and postoperative data were recorded and assessed. For functional outcomes, the knee range of motion and Rasmussen functional scoring system was used. Result: The mean union time was 9.8 weeks and 3 cases had < 5\? of varus, 10 cases had< 5º valgus, and 1 patient developed varus of +7.08o. Rasmussen's Functional Scores were excellent or good in 71% of patients. Superficial wound infection was seen in 1 patient who subsided uneventfully. Conclusion: Use of Poller screw is very effective in the prevention of angular deformities in case of proximal one-third fractures of tibia managed with intramedullary nailing.
Keywords: Poller Screw, Blocking Screw, Proximal Tibia Fractures, Tibia metaphyseal Fractures, Intramedullary Nailing.
Full Text:
Introduction
The intramedullary nail is designed to treat diaphyseal fracture of the tibia and is the standard treatment modality for tibia mid diaphyseal fractures.1,2 The intramedullary fixation of mid diaphyseal fractures differs from the proximal one-third fractures which have a small proximal fragment. This can cause an increase in alignment deformity, which is most commonly seen in the coronal plane. These deformities are due to many factors like discrepancy in diameter of the nail and wide tibial metaphysis, inaccurate entry point, displacing muscular forces, and residual instability. Poller screw acts as a blocking screw which reduces the width of the metaphysis and physically blocks the nail by creating an “artificial cortex”. This helps in increasing the mechanical stiffness of the implant-bone construct and, thus, minimizes the translation of nail as well as deformity.3,4 These can be used in proximal one-third fractures of the tibia. The term ‘Poller’ denotes a short metal post placed on a ship or road to control or guide traffic.5 We aim to evaluate the alignment, deformity correction, and functional outcome of proximal one-third fractures of tibial shaft managed by a nail and a poller screw. In this study, we present a prospective follow-up of the patients with fractures of proximal 1/3rd tibia managed with an intramedullary nail and blocking screw.
Material and methods
The study was conducted in the Institute of Medical Science and SUM Hospital, Bhubaneswar, India from August 2017 to August 2019 for 2 years. A total of 14 skeletally mature patients (10 males and 4 females) with extra-articular proximal one third tibia fracture were operated and evaluated prospectively for functional and radiological outcomes. Prior Institutional ethical clearance was obtained and all the patients were explained about the procedure and informed written consent was also obtained. The patients were selected based on our inclusion criteria; i.e. a) Skeletally mature patients, both sex, b) Displaced extra-articular metaphyseal fracture, c) compound fracture (Gustilo-Anderson Grade 1 and 2) and d) Patients who gave written consent for surgery. The exclusion criteria were, a) Skeletally immature patient and severe osteoporosis, b) Comminuted fractures, c) Metaphyseal fracture with intra-articular extension and, d) surgically unfit patients. All patients were operated within one week of trauma.
The principle of surgical management is to maintain axial alignment, proper length, and early mobilization, and restore function. On the standard operating table, supine position with knee kept in a semi-flexed position, a mid patellar tendon splitting incision was made. An accurate entry-point was made and a guidewire was inserted under fluoroscopic guidance. The medullary canal was reamed using a flexible reamer of the smallest diameter (8 mm). Now the deformity was assessed by removing the reamer and guide wire and checking under a fluoroscope. Poller screw was placed in the proximal fragment of the tibia on the side where the deformity is concave to prevent valgus or in mediolateral direction to prevent procurvatum and was confirmed in both Antero-Posterior (AP) and lateral (Lat) views under image intensifier. The blocking screw should be placed at least 1 cm proximal to fracture to minimize complications. Now, a guidewire is re-introduced further medially to the poller screw and reaming is done with flexible reamers of progressively increasing diameters. The intramedullary interlocking nail is then inserted and fixed with proximal and distal locking screws (Figure 1). None of the patients was given any form of immobilization. Intraoperative data like operative time, reduction difficulties, and residual deformities were collected.
Postoperatively, knee bending and quadriceps strengthening exercises were started on day one. Partial weight-bearing with the help of a walker was started on post-op day 7 and continued for 6-8 weeks (depending on fracture pattern). Complete weight-bearing was allowed after 6-8 weeks. Patients were followed at regular intervals of 6 weeks, 12 weeks, 3 months, 6 months, and 9 months and were evaluated radiologically and functionally using Knee range of motion and Rasmussen’s Functional Scoring System.
Statistical Analysis
The data were tabulated in Microsoft Excel and statistical analysis was performed using SPSS 20 (SPSS, Inc., IL).
Results
In our study, most of the patients (9) were in the age group of 30-40 years followed by 3 patients in the age group of 20-30 and one patient each in the age group of 40-50 years and 50-60 years with a male preponderance (M:F::5:1). Eight patients had a closed fracture while six patients had compound fracture which was classified according to Gustilo and Anderson Classification. All the six compound fractures were either Grade 1 or 2.Majority of the patients in our study (11 patients) had road traffic injury as the mode of injury while 3 patients had a fall from height. The basic demographic data are given in Table 1-4. All patients were operated at a mean interval of 3 days from injury (Range- 1 to 6 days). The mean operative/surgical time was 68.1 minutes. We did not encounter any intraoperative complications and reduction difficulties. Postoperatively, 3 cases had <5° of varus, 10 cases had <5º valgus malalignment, and only one patient developed varus of +7.08o. The mean fracture union time was 9.8 weeks (Range, 8.4-12.4weeks). The union time of 8 weeks was seen in 3 patients while 8 patients had union within 8 to 12 weeks. Another 3 patients had union beyond 12 weeks. Minor complication like superficial wound infection was noted in one case which settled within 2 weeks with I .V. antibiotics according to culture and sensitivity. Full knee range of motion (0-130 degrees) was seen in 8 (57%) patients while 4 patients (28%) patients had a 0-110 degree range of motion. Two (14%) patients had a 0-70 degree range of motion at the final follow up (Table-6). According to Rasmussen’s Functional Scoring System, the results were excellent in 8 patients while they were good and fair in 4 and 2 patients, respectively. None of the patients had a poor score. (Table 7)
Discussion
The use of trans-medullary poller screw along with an intramedullary nail improves reduction and fixation of proximal one third tibia fracture at or near metaphysis where there is a strong tendency for coronal and sagittal plane displacement.
Several factors limit the reduction in proximal one third tibia fracture like pulling of the proximal fragment by patellar tendon while locking the nail in the extension position of the knee, wide medullary canal. The reduction is very difficult if the fracture is at or just above the Herzog bend of the nail.
The blocking screw augments the fixation construct as well as helps in guide the nail to the distal portion of the fracture. Poller screw provides a contact point for proximal fragment and the nail on its side and provides a three-point intramedullary construct which is mandatory for stability.5
In our study; for the coronal plane deformity correction, poller screws were placed at a point in the proximal segment 1 cm above the fracture. This is a little lateral to the proximal tibia central axis; so that the nail passes medial to the blocking screws. For the deformity in the sagittal plane; the position of the blocking screw is at a point in the proximal fragment that is in the posterior half. The direction is from medial to lateral and this helps the nail to remain near to the anterior cortex as it is progressed down the medullary canal.
In our study, out of 14 patients, ten patients had valgus <5º, 3 patients varus <5º, one patient had varus 12º, one patient with procurvatum and recurvatum was not found in any patient which is comparable to study conducted by Ricci et.al who studied on 12 patients in which only the one had a postoperative valgus misalignment of 6º that later progressed to 10º at final follow-up; however, blocking screws was not used in this case.6
In our study, non-union was not developed in any case and these results are more or less coincident with studies conducted by Ricci et al. and Nork et al.6,7
In our study, one superficial infection was noted which is settled by dressing and antibiotic according to culture & sensitivity. One patient met with iatrogenic extension fracture while applying a blocking screw intra-operatively. Two patients complained of anterior knee pain in the early postoperative period which was resolved after the rehabilitation programme.
In another study which was a retrospective study conducted by Freedman and Johnson in which they evaluated a hundred and thirty-three tibia fracture managed with intramedullary nails.8 They found that there is a higher frequency of malalignment in proximal one-third fractures as compared to the middle or distal third. They suggested that the use of a blocking screw may reduce these complications.
Poller screws are superior to other supplements of fixation like K-wire, Steinmann pin, Schanz pin, and unicortical plate because it is rigid, no need to remove, and cost-effective.8,9
Tornetta et al. described a technique of nailing in the proximal tibia fracture with the medial para-patellar approach with the semi extended knee position.10
Various other studies have documented the use of poller screws and concluded that it aids in reduction and correction of angular deformities.11-15
A recent approach of nailing is the suprapatellar entry portal in a semi-extended position reduces the deformity.
All the proximal tibia fractures in our study were treated by blocking screws. The current study has a few limitations like the small sample size of 14 patients. This is not a comparative study, non-randomized, and non-controlled clinical trial.
Conclusion
We conclude that Poller screw when used as a supplement to the intramedullary nailing of metaphyseal fractures of the tibia, provides an effective achievement of fracture alignment. It also improves the mechanical stability of the bone-implant construct, by functionally reducing the medullary canal width, maintains the fracture alignment till union, and prevents loss of initial reduction. When applied during the insertion of the nail, they help in guiding the nail centrally. Minimal soft tissue dissection during fracture reduction, cost-effective, and reduces the operative procedure time are other advantages. It also helps in the prevention of iatrogenic fracture during manipulation for fracture reduction.
Acknowledgement
I would like to thank my teachers, colleagues, and patients without whose support and cooperation in this study were impossible. We also acknowledge the immense help received from previous articles cited in our study.
Conflict of Interest
There is no conflict of interest to declare.
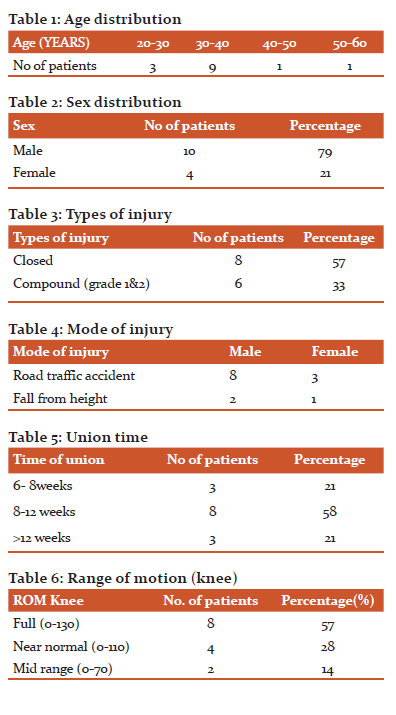
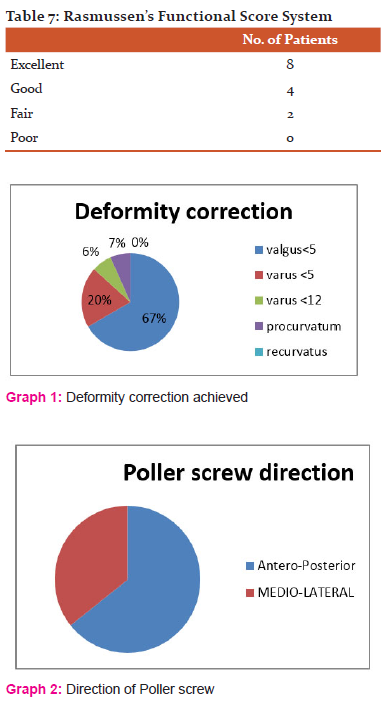

Figure 1- A) Preoperative anteroposterior and lateral radiograph of a patient with proximal 1/3rdtibial fracture, B) and C) Intra-operative anteroposterior and lateral views under image intensifier of the same patient showing correct angulation of the fracture site after giving poller screw and intramedullary nail. D) Postoperative lateral view radiograph at 6 weeks follow up.
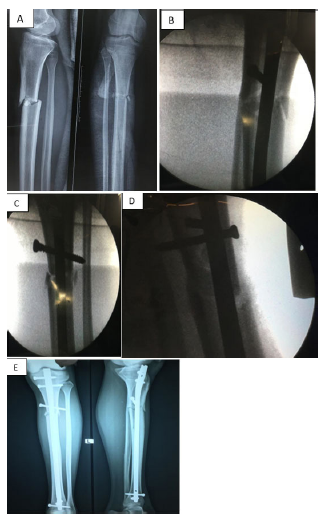
Figure 2- A) Preoperative anteroposterior and lateral radiograph of another patient with proximal 1/3rdtibial fracture, B), C) and D) Intra-operative anteroposterior and lateral views under image intensifier showing the position of poller screw and intramedullary nail. E) Postoperative AP and lateral view radiograph at 10 weeks follow up.
References:
-
Schmidt AH, Finkemeier CG, Tornetta P. Treatment of closed tibial
fractures. Instr Course Lect 2003; 52:607–622.
-
Zelle BA, Bhandari M, Espiritu M, Koval KJ, Zlowodzki M. Evidence-Based Orthopedic Trauma Working Group. Treatment of distal tibia fractures without articular involvement: a systematic review of 1125 fractures.J Orthop Trauma 2006; 20:76–79.
-
Freedman EL, Johnson EE. Radiographic analysis of tibial fracture malalignment following intramedullary nailing. Clin Orthop Relat Res 1995;315:25–3
-
Krettek C, Stephan C, Schandelmaier P, et al. The use of Poller screws as blocking screws in stabilising tibial fractures treated with small diameter intramedullary nails. J Bone Joint Surg Br. 1999 Nov; 81(6):963-8.
-
Krettek C, Miclau T, Schandelmaier P, Stephan C, Möhlmann U, Tscherne H. The mechanical effect of blocking screws (‘Poller screws’) in stabilizing tibia fractures with short proximal or distal fragments after insertion of small-diameter intramedullary nails. J Orthop Trauma 1999; 8:550–553.
-
Ricci WM, O’Boyle M, Borrelli J, et al. Fractures of the proximal third of the tibial shaft treated with intramedullary nails and blocking screws. J Orthop Trauma 2001;15:264–70
-
Nork SE, Barei DP, Schildhauer TA, Agel J, Holt SK, et al. (2006) Intramedullary nailing of proximal quarter tibial fractures. J Orthop Trauma 20(8): 523-528
-
Salai M, Israeli A, Amit Y, Blankstein A, Horoszowski H. Closed
intramedullary nailing of tibial fractures in elderly patients. J Am
GeriatrSoc 1984;32:939-41.
-
Kulkarni SG, Varshneya A, Kulkarni S, Kulkarni GS, Kulkarni MG, et al. (2012) Intramedullary nailing supplemented with Poller screws for proximal tibial fractures. J Orthop Surg (Hong Kong) 20(3): 307-311
-
Tornetta P, Collins E. Semiextended position of intramedullary nailing of the proximal tibia. Clin Orthop. 1996; 328:185-189
-
Shahulhameed A, Roberts CS, Ojike NI. The technique for precise placement of poller screws with intramedullary nailing of metaphyseal fractures of the femur and the tibia. Injury. 2011;42(2):136?139.
-
Dodd L, Jackson M, Varma R. Poller Blocking Screws and Intramedullary Nailing in TibialMalunion. Ann R CollSurg Engl. 2007;89(8):816?818.
-
Tennyson M, Krkovic M, Fortune M, Abdulkarim A. Systematic review on the outcomes of poller screw augmentation in intramedullary nailing of long bone fracture. EFORT Open Reviews. 2020 Mar 1;5(3):189–203.
-
MoongilpattiSengodan M, Vaidyanathan S, Karunanandaganapathy S, Subbiah Subramanian S, Rajamani SG. Distal tibial metaphyseal fractures: does blocking screw extend the indication of intramedullary nailing? ISRN Orthop 2014;17:542623
-
MoongilpattiSengodan M, Vaidyanathan S, Karunanandaganapathy S, Subbiah Subramanian S, Rajamani SG. Distal tibial metaphyseal fractures: does blocking screw extend the indication of intramedullary nailing? ISRN Orthop 2014;17:542623
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License