IJCRR - 9(7), April, 2017
Pages: 15-18
Date of Publication: 11-Apr-2017
Print Article
Download XML Download PDF
A Pilot Study on Vitamin D and Respiratory Diseases in Southern Part of India
Author: Vijetha Shenoy Belle, Priyanka Datta, Krishnananda Prabhu, Kriti Singh
Category: Healthcare
Abstract:Background: Over the past decade, interest has grown in the role of vitamin D in many nonskeletal medical conditions, such as cancer, diabetes mellitus, and cardiovascular diseases including respiratory infection. Emerging evidence indicates that vitamin D-mediated innate immunity is important in host defenses against respiratory tract pathogens. There are few researches linking vitamin D to various immune-related conditions, including asthma, allergic rhinitis, although the pattern of this relationship is still yet to establish. This study was done to understand the role of vitamin D levels in patients with respiratory tract infection in the southern part of India.
Materials and Methods: After obtaining ethical clearance from the institutional ethics committee retrospective study was conducted. A total of 125 Patients with respiratory complaints like bronchial asthma, chronic obstructive pulmonary disease, and allergic rhinitis were included.100 healthy volunteers were included as a control. Total serum vitamin D assay was measured by ECLIA method. Serum IgE levels were measured using COBAS 6001 analyzer. Statistical analysis was done using SPSS 16.0 version.
Results: Vitamin D level was highly significantly lower(p < 0.01) in the respiratory diseases group compared with the control group, and the total IgE level was highly significantly higher in the asthmatic groups compared with the control group.
Conclusion: Deficiency of Vitamin D levels may predispose to respiratory infections. Supplementation with vitamin D, exposure to sun light and increased physical activity may decrease the predisposition to respiratory tract infection.
Keywords: Vitamin D, Respiratory tract infections, IgE
Full Text:
Introduction:
The sunshine hormone, vitamin D is seco-steroid hormone, produced in the skin by sun exposure under the influence of UVB light. In the liver it is hydroxylated to 25-hydroxy vitamin D [25 (OH) D] by 25- hydroxylase enzyme. In kidney 1, 25-dihydroxyvitamin D, which is the final product, requires the enzyme 1-alpha-hydroxylase, also occurs in extra renal tissues, epithelial cells and immune cells. [1,2]Vitamin D insufficiency is increasingly seen in the general population due to dietary, lifestyle and behavioral changes.
The active vitamin D is present only in minute concentrations in the circulation and it is crucial for vitamin D mediated effects on immune system at the site of local activation. The prevalence of vitamin D deficiency has been increasing in the general population in recent decades. Observational studies suggest that vitamin D deficiency increases risk of respiratory infections. Vitamin D was found to be modulating the regulatory T-cell function and interleukin-10 production. [3,4]
It has long been thought that by inducing respiratory muscle weakness, vitamin D deficiency gives rise to difficulties in eliminating respiratory secretions and thus facilitates the development of infections.
These concepts now need to be integrated with the role of vitamin D in the respiratory system. Children with rickets and asymptomatic vitamin D deficiency were more likely to develop pneumonia, and this was observed in children in India.[5]
Respiratory tract infection (RTI) is widespread not only in the pediatric age group but also in adults. It is the major cause of mortality and morbidity. 2.8 million deaths were by RTI during 2010.A link between vitamin D and respiratory tract infection has been hypothesized. Recent evidence suggests that vitamin D causes suppression of inflammation and strengthening of immunity by the induction of antimicrobial peptides. Early studies of vitamin D in mice came to different conclusions, with one group reporting a link and the other no link between deficiency and infection. More recent studies in humans also had divergent results. Evidence indicates that vitamin D-mediated innate immunity is important in host defenses against respiratory tract pathogens.
Vitamin D affects B lymphocytes functions and modulates the humoral immune response including secretion of IgE.[6,7]
In addition, vitamin D modulates the adaptive immune system via direct effects on T-cell activation and on the phenotype and function of antigen-presenting cells.
Cross-sectional data indicate that low vitamin D levels in patients with mild to moderate asthma are correlated with poor asthma control, decreased lung function, decreased glucocorticoid response, more frequent exacerbations, and consequent increased steroid use[8,9]. However, there is insufficient evidence to support a causal association between vitamin D status and asthma. Also, there are very limited data in adult asthma patients addressing the impact of vitamin D status on disease control and severity [10, 11].
Therefore, the aim of this study was to investigate the adult patients with respiratory infections and its potential relationship with vitamin D levels in the southern part of India.
Materials and methods:
Study subjects:
Between March 2013 to July 2013, 125individuals of 30- 65years age group having A total of 125 Patients with respiratory complaints like bronchial asthma, chronic obstructive pulmonary disease, and allergic rhinitis visiting Kasturba Hospital, Manipal University, Manipal, India were enrolled in the study. 100 healthy volunteers were included as a control group.
Study groups:
Individuals were divided in three groups according to their disease group I = patients with asthma. Group II patients with rhinitis and group III with COPD
Exclusion Criteria:
Patients suffering from diabetes, mal-absorption, pregnant women, patients of significant cardiac, hepatic, renal, oncologic or psychiatric diseases and those on long term medications were excluded from the study.
Ethical statement:
Ethics clearance was obtained prior to data collection from the institutional ethics committee Kasturba Hospital, Manipal University, Manipal, India.
Sample collection:
Using aseptic precautions 4ml of venous blood samples were collected in red capped vaccutainer and were used for estimation of vitamin D.
Method of estimation of vitamin D and IgE:
Total serum vitamin D assay was measured by Electro Chemi-Luminiscence Immuno Assay (ECLIA) method in Elecsys 2010. Serum IgE levels were measured using COBAS 6001 analyser, Electro Chemi-Luminiscence Immuno Assay (ECLIA). The instrument is calibrated to provide quantitative values for Serum IgE up to 2500 IU/ml.
Statistical analysis:
Data was compiled and statistical evaluation was done using Statistical Package for the Social Sciences (SPSS) 16.0. Data were expressed as mean± standard deviation. ANOVA was used for comparison between groups. P value <0.05 is considered as statistically significant.
Result:
During the study period we studied 225 subjects recruited from the outpatient clinic (100 healthy volunteers, 50 diagnosed as asthma, 30 had allergic rhinitis and 45 patients had COPD).
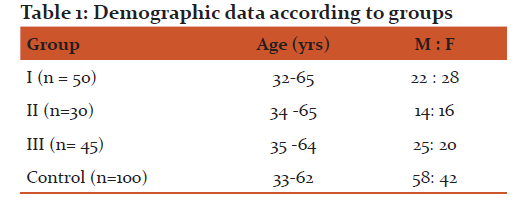
Characteristics of the study population are shown in Table 1. The mean age of the studied subjects did not differ between the disease group and control group.
Discussion:
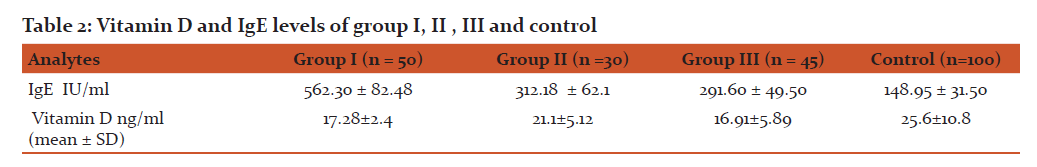
The results of the present study showed that serum vitamin D level was significantly lower (p <0.01) in the asthma and COPD compared with the control group.
This study is in agreement with that by Li et al. [11] who studied serum vitamin D level in 435 asthma patients older than 18 years (268 women and 167 men); they found that the concentration of 25(OH) vitamin D [25(OH)D] ranged from 9 to 85 nmol/l.
In our study, patients of Allergic Rhinitis(AR) showed deficiency in vitamin D indicated by mean vitamin D level of 21.1 ± 5.12 ng/ml before treatment. This result suggests the importance of assessing vitamin D levels in patients of AR. There are studies recently coming in support of this fact as stated by Arshi et al. [12] The prevalence of severe vitamin D deficiency was significantly higher in patients with AR than the normal population.
In a study performed by Moradzadeh et al. [13] the prevalence of severe vitamin D deficiency was significantly greater in patients with AR than the normal population (30% vs. 5.1%; P = 0.03) demonstrating that there is an association between serum vitamin D levels and AR status. These results may indicate subtle differences in terms of vitamin D metabolism or sensitivity in allergic patients, as hypothesized by Wjst and Hyppönen.[14]
In our study, the increased levels of serum IgE were considered to mostly reflect the allergic inflammation of the airways. Firstly, the prevalence and the levels of IgE elevation were much lower in the control population when compared with those of the COPD patient.
The results of the present study showed that serum IgE level was significantly higher(p <0.01) in the asthma group compared with the control group. Our study is in agreement with the study by Thirunavukkarasu et al. [15] who investigated serum IgE level in 60 asthmatic patients between 18 and 60 years of age, classified according to the GINA classification (31 male and 29 female), and 13 healthy controls between 18 and 60 years of age. They found that the mean IgE level in the control group was 151 IU/ml and that in the asthmatic group ranged from 404 to 1045 IU/ml.
There are plenty of evidences to show that vitamin D has potent immunomodulatory properties.[16]. During a bacterial infection, macrophages acquire the capacity to convert circulating 25 vitamin D into 1, 25 OH vitamin D, which a direct inducer of the expression of genes is encoding for antimicrobial peptides and cathelicidin antimicrobial peptide in particular.[17]
Airway epithelia contain high levels of the enzyme that converts circulating 25-OH-vitamin D3 to its active form 1,25-OH-vitamin D3. The active form of vitamin D has local effects in response to respiratory infections and might dampen the inflammation that is the consequence of these infections [18]. This study is in agreement with the study by Eman Shebl et al. [19]as well, who reported that there was a significant increase in the number of severe bronchial asthma patients with vitamin D insufficiency (41.4%) compared with those with sufficient vitamin D.
Vitamin D regulates gene expression through binding with vitamin D receptors (VDR). Active vitamin D binds to the VDR and dimerizes the retinoic X receptor. Vitamin D- VDR complex bind to vitamin D- responsive elements inside the promoter regions of vitamin D responsive genes.[20]Nuclear receptor co activator proteins enhance transcriptional activation. Expressions of gene that are involved in immunity are modulated by VDR. Toll- like receptors (TLR) monitors the host for the presence of pathogen. TLR activation of human macrophages upregulates VDR expression and vitamin D-1 hydroxylase genes, which enhances the induction of the cathelicidin[21]. Respiratory epithelial cells activate vitamin D. The local activation of vitamin D might be an important component for host defense.
In addition, reduced vitamin D levels are associated with increased expression of TNF-alpha, suggesting that enhanced expression of this pro-inflammatory cytokine is a potential pathway by which reduced vitamin D levels could exert pro-inflammatory effects in asthma [22].
We speculated that elevated serum IgE might promote the airway inflammation and remodeling, and then resulted in more serious symptoms and worse status of lung function. So we must assess the levels of IgE in obstructive airway diseases and classifying them according to its level.
There is a correlation between serum vitamin D levels and AR and asthma. Controversial data regarding correlation between level of vitamin D and eosinophil count and total IgE are presented in recent studies: some authors show that there is no link between these markers [23] , while others, present the relation [24].
Supplementation of vitamin D in such patients may alter natural course. Although more studies with a larger number of patients should be conducted to validate the role of vitamin D supplementation therapy along with initial anti allergic treatment.
Further studies are required to clarify this hypothesis. The role of vitamin D in the pathogenesis of immune-mediated diseases such as asthma is only beginning to be understood.
Conclusion: The main conclusion of our study deficient levels of vitamin D is total burden of respiratory tract infections. Vitamin D supplements, exposure to sun and physical activity may decrease the burden of respiratory infections in adults. The role of vitamin D in the immune system and in pathogenesis of various diseases has the potential to have profound effects on our ability to prevent and treat these disorders.
Acknowledgement :
We would like to express our greatest gratitude to the people who have helped and supported us through out our project. We are grateful to the Dean of Kasturba Medical College Manipal for providing the facilities for conducting the study
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Conflict of interest: The authors declares that there is no conflicts of interest regarding the publication of this article .
References:
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81.
- Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87:1080–6.
- Black PN, Scragg R. Relationship between serum 25-hydroxyvitamin d and pulmonary function in the third national health and nutrition examinationsurvey. Chest. 2005;128:3792–8.
- Searing DA, Leung DY. Vitamin D in atopic dermatitis, asthma and allergic diseases. Immunol Allergy Clin North Am. 2010;30:397–409.
- Wayse V, Yousafzai A, Mogale K, Filteau S. Association of subclinical vitamin D deficiency with severe acute lower respiratory infection in Indian children under 5 y. Eur J Clin Nutr 2004;58:563–567.
- Searing DA, Leung DY. Vitamin D in atopic dermatitis, asthma and allergic diseases. Immunol Allergy Clin North Am. 2010;30:397–409.
- Sun J. Vitamin D and mucosal immune function. Curr Opin Gastroenterol 2010;26:591–595
- Brehm JM, Celedon JC, Soto-Quiros ME, Avila L: Serum vitamin D levels and markers of severity of childhood asthma in Costa Rica. Am J Respir Crit Care Med 2009, 179:765–771.
- Chinellato I, Piazza M, Sandri M, Peroni D, Piacentini G, Boner AL: Vitamin D serum levels and markers of asthma control in Italian children. J Pediatr 2011, 158:437–441.
- Sutherland ER, Goleva E, Jackson LP, Stevens AD, Leung DY: Vitamin D levels, lung function, and steroid response in adult asthma. Am J Respir Crit Care Med 2010, 181:699–704.
- Li F, Peng M, Jiang L, Sun Q, Zhang K, Lian F: Vitamin D deficiency is associated with decreased lung function in Chinese adults with asthma. Respiration 2011, 81:469–475.
- . Arshi S, Ghalehbaghi B, Kamrava SK, Aminlou M. Vitamin D serum levels in allergic rhinitis: Any difference from normal population? Asia Pac Allergy 2012;2:45?8
- Moradzadeh K, Larijan B, Keshtkar AA, Hossein?Nezhad A, Rajabian R, Nabipour I, et al. Normative values of vitamin D among Iranian population: A population based study. Int J Osteoporos Metab Disord 2008; 1:8?15.
- Wjst M, Hyppönen E. Vitamin D serum levels and allergic rhinitis. Allergy 2007;62:1085?6.
- Thirunavukkarasu S, Mysore S, Chickballapur R, Srikantaiah C, Mohan R, Rage E et al. Evaluation of serum immunoglobulin E levels in bronchial asthma. Lung India 2010; 27:138–140.
- Adams JS, Hewison M. Unexpected actions of vitamin D: new perspectives on the regulation of innate and adaptive immunity. Nat Clin Pract Endocrinol Metab 2008;4:80–90.
- Yim S, Dhawan P, Ragunath C, Christakos S, Diamond G. Induction of cathelicidin in normal and CF bronchial epithelial cells by 1,25-dihydroxyvitamin D(3). J Cyst Fibros 2007;6:403–410
- Felicia M, Giovanni S, Allan R. Vitamin D insufficiency is associated with asthma severity. Allergy Asthma Immunol Res 2013;5:283–288
- Eman Shebl R, SM Shehata, M Elgabry, SAI Ali, Elsaid HH. Vitamin D and phenotypes of bronchial asthma. Egypt J Chest Dis Tuberc 2013;62:201–205.
- Liu PT, Stenger S, Li H, Wenzel L, Tan BH, Krutzik SR et al . Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006 Mar 24;311(5768):1770-3
- Berry MA, Hargadon B, Shelley M, Parker D et al. Evidence of a role of tumor necrosisfactor alpha in refractory asthma. N Engl J Med 2006, 354:697–708.
- Mora JR, Iwata M, von Andrian UH: Vitamin effects on the immunesystem: vitamins A and D take centre stage. Nat Rev Immunol 2008,8:685–698.
- F. Li, M. Peng, L. Jiang, Q. Sun, K. Zhang, F. Lian, et al.Vitamin D deficiency is associated with decreased lung function in Chinese adults with asthma. Respiration 2011, 81(6): 469–475.
- S. Sharief, S. Jariwala, J. Kumar, P. Muntner, M.L. Melamed.Vitamin D levels and food and environmental allergies in the United States: results from the National Health and Nutrition Examination Survey 2005–2006 .J Allergy Clin Immunol, 2011;127(5): 1195–1202.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License