IJCRR - 8(9), May, 2016
Pages: 17-20
Date of Publication: 12-May-2016
Print Article
Download XML Download PDF
METASTATIC OVARIAN CYSTOSARCOMA PHYLLOIDES OF BREAST
Author: Papa Dasari, Haritha Sagili, Priyanka Yoga Purani
Category: Healthcare
Abstract:Background: Cystosarcoma Phylloides is a rare breast neoplasm constituting ≤ 1% of all breast neoplasms. These are mostly benign and reccur. Malignant cystosarcoma Phylloides can recur and metastasize to lung, bone and abdominal viscera. Metastasis to Ovary is not reported in literature. Case Report: A 46 year old multiparous lady was diagnosed with a recurrent cystosarcoma of right breast and a large Ovarian mass which was causing her dyspnoea. The mass was of 30 weeks size and was firm and tender. CECT showed a large solid abdominopelvic mass with irregular enhancing septate extending from pelvis to infracolic area with minimal free fluid. Uterus and Ovaries could not be delineated. FNAC from the mass was reported as low-grade malignant mesenchymal tumour. CA 125 was within normal range. Laparotomy revealed a large fleshy mass with jelly like material which was adherent to intestines and pelvic and parietal peritoneum. Right ovary is not visualized. Left ovary parially visualised and incorporated into the mass. Excision of the mass with TAH and BSO was carried out. There was diffuse ooze from the pelvic and peritoneal cavity which was managed by packing, blood product transfusion and tranexamic acid. She received massive transfusion and survived. Later she developed haemoptysis and underwent tracheostomy and feeding ileostomy and was managed in ICU for 8 weeks. Palliative mastectomy and adjuvant Radiotherapy and chemotherapy were differed by Oncologists and hence she was discharged after 4 months of admission. Conclusion: Managing ovarian metastasis from cystosarcoma phylloids can be challenging and the quality of life is poor when the primary disease is not managed adequately.
Keywords: Metastatic ovarian cystosarcoma phylloides, Breast, Large solid abdominopelvic mass, Ovarian tumour
Full Text:
INTRODUCTION Phylloid tumours account for less than 1% of breast masses and occur rarely. They affect women at young and middle age unlike adenocarcinomas which occur at a later age. .They most often reccur locally and 20% to 40% develop distant metastasis. The most common sites of distant metastases are lung, bone and abdominal viscera1 .The abdominal visceral metastasis is reported in duodenum and Pancreas.2 Metastasis to ovaries is not found in literature. Hence this rare case is reported.
CASE REPORT A 46-year-old para2 live 2 whose child birth was 14 years back underwent simple mastectomy for a right sided breast mass one month ago at a private hospital, the histopathology was consistent with cystosarcoma phylloids. The breast mass re-appeared at the same site with in one month of surgery. FNAC from the recurrent breast mass revealed cystosarcoma phylloids with stromal elements. She also developed sudden onset of pain abdomen and distension of abdomen of one month duration and decreased urine output, difficulty in breathing and constipation of 12 days duration. CT scan of abdomen and pelvis reported a large solid mass in abdomen and pelvis with minimal free fluid in pelvis.
The mass is not separately seen from uterus and ovaries. She was referred to our Institute with a diagnosis of recurrent cystosarcoma phylloids with Ovarian tumour. Her Obstetric and gynecological history revealed that she had 2 normal deliveries and underwent tubectomy 14 years back and there was no family history of malignancies. She had polymenorrhea .She gave history of loss of weight and loss of appetite for the past 6 months.She also had urinary retention and hence she was on continuous bladder drainage for one week. She complained of fever with chills of 10 days duration. On examination she was emaciated, tachypnoeic, febrile, pulse was 108/min regular, BP 100/60 mm Hg. No significant lymphadenopathy. There was a hard mass of 10x6x3 cm in size on the lateral aspect of right breast with local rise of temperature and tenderness. Left breast was normal. Respiratory system was normal.
Cardiovascular system was normal except for tachycardia. Abdomen was grossly distended in sub- umbilical and umbilical region. There was a hard immobile tender mass of 30 weeks size arising from pelvis. Bowel sounds were normal. General surgical opinion was recurrent or residual cystosarcoma phylloides (as the resected margins were reported positive) with Ovarian tumour and advised to manage the ovarian tumour first. Her abdominal USG was reported as a large abdominopelvic complex mass with minimal ascites displacing the bowel loops laterally suggestive of Ovarian mass. Her CECT at our Institute after one week of admission reported as a large abdominopelvic dense mass with irregular enhancing septate extending from POD to infra colic areas.
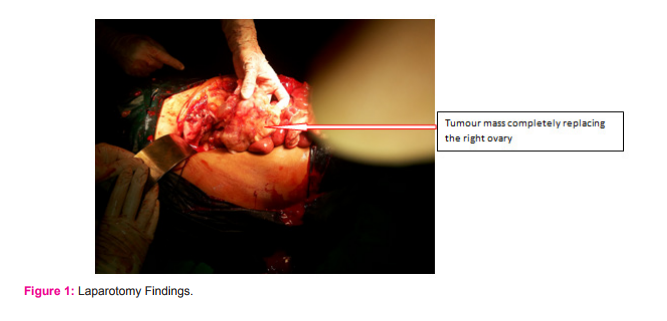
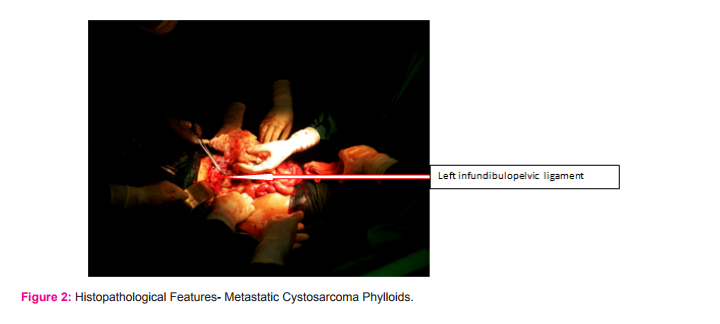
Ovaries are not visualized separately. FNAC from the abdominal mass was reported as a low grade malignant mesenchymal tumour. She was taken up for laparotomy 2 weeks after admission after surgical oncologist opinion. On laparotomy there was hemorrhagic ascites of more than 500ml. There was a large fleshy mass with jelly like material with a breach on the surface suggesting tumour rupture. The mass was of 28 week size occupied pelvis and lower abdomen and extended up to the root of the mesentery and covered by small bowels which were closely adherent. There was lot of mucoid material within the mass appearing like myxoid degeneration (Fig1a). Both ovaries incorporated in to the mass and right ovary could not be recognised and left ovary was only partially recognized (Fig 1b) Both fallopian tubes were free. Uterus was 10 weeks size and anterior to the mass which was densely adherent to POD, lateral pelvic walls and rectosigmoid.
The mass was separated from the intestines and excised with the help of surgical oncologist. Total abdominal hysterectomy with bilateral salphingo opherectomy was carried out. There was lot of oozing from the intestinal surfaces and peritoneal surfaces of POD. Multiple haemostatic sutures were taken and bilateral internal iliac arteries were ligated. As the oozing persisted from the peritoneal surfaces , pelvis and abdomen was packed. Blood loss was 1000 ml and she received 5 units of FFP, 4 packed cells. In view of poor general condition she was ventilated and was kept on SIMV mode. Abdominal pack was removed after 48 hours under general anaesthesia. She was monitored in post-operative ward and received 22 units of FFPs, 4 units of platelets,3 units of Packed cells, 12 units of cryoprecipitate over a period of 8 days. She also received intravenous tranexamic acid during surgery and for 48 hours following surgery.
Mastectomy was deferred at the time of laparotomy though it was planned to do earlier by the surgical oncologist. She could be started on oral fluids after a week and was shifted to ward after 10 days of surgery. On 14 th postoperative day she developed sudden dyspnoea and was managed conservatively with oxygen and sedation. Her fever persisted despite of 3 broad spectrum intravenous antibiotics. She had superficial wound gaping and developed dyspnoea again with decreased saturation. She was kept on mechanical ventilation. X Ray chest P/A revealed minimal left sided effusion with basal atelecatsis. She underwent tracheostomy after 4 days as prolonged ventilation was required . She produced thick sputum which required mucolytic and frequent suctioning. After 10 days she was weaned off ventilator and was maintaining 100% saturation.
The histopathological report was metastatic malignant cystosarcoma Phylloids to ovary and parametrium. Fallopian tubes and uterus and cervix were free of tumour. Tumour showed high cellularity and moderate nuclear atypia and high mitosis 16/10 high power field with extensive myxoid change. (Fig 2 a, b,and c) This was consistent with previously diagnosed and treated malignant phylloids. Her haematological parameters were with in normal limits. She was given one course of Ifosphamide and MESNA which she tolerated well. She was given total parenteral nutrition for almost one month. After seven days of receiving chemotherapy she became dyspnoeic and right sided air entry decreased and she was shifted to RICU(Respiratory Intensive care Unit) under care of the anaesthetists. Her abdominal wound healed by secondary intention. She was given ICU care and underwent feeding jejunostomy . She was decanulated after 8 weeks of tracheostomy. The breast mass increased in size 20x10 cms, infected and displaced to right lateral side of chest. Surgical Oncologists deferred in doing any kind of palliative surgery and medical oncologists and Radiation Oncologists deferred in giving chemotherapy and radiation therapy. She was in RICU for 6 weeks and received antibiotics as per the sensitivity of the organisms from wound swab, tracheal swab, infected breast mass swab etc.,.
The organisms were Acenetobacter, klebsiella, pseudomonas .The abdomen was scaphoid and there was no evidence of fluid or mass. She was asked to take over by Gynaecologists. As there was no gynaecological treatment necessary and the surgical Oncologists deferred in performing palliative surgery she was explained the inability to give further supportive treatment and discharged home.
local excision the resected margin should be free of tumour for 1 cm. Local recurrence is expected in 15 % of cases even with this modality of treatment3 . Cystosarcoma Phylloids are diagnosed to be benign, borderline and malignant based on histopathological characteristics and a clinical diagnosis of malignant variety is not made as recurrence and even metastasis can occur in benign tumours. A study correlating histopathological features with clinical presentation in 187 cases , found local recurrence in 27%, 32% and 26% of benign, borderline and malignant tumours respectively. Metastasis was present in two borderline and six malignant tumors out of 100 (8%). There were no specific histological features that correlated with local recurrence and metastasis but cytological atypia of stromal cells, stromal overgrowth and mitotic figures of >15 per 50 high power fields were present in those who showed metastasis.4 Flow cytometric analysis of s fractions greater than 0.05 was found to be a useful predictor of clinical outcome along with histological features of stromal overgrowth and and infiltrating margins5 . A literature review in 1999 to find out the predictors of recurrence after conservative surgery of cystosarcoma phylloids concluded that wide local exicision is also a suboptimal modality of treatment for borderline and malignant phylloid tmours because the recurrence rate is high (29% for borderline and 36% for malignant).6
The most common site of metastasis is lung7 and other sites reported are spine, brain, parotid gland, nasal cavity, forearm and mandible. The metastatic sites in the abdomen reported are pancreas, duodenum, jejunum and liver. Metastasis to genital organs is very rare and only one case report of metastasis to vulva 8 and another to Brenner tumour of ovary is found in literature9 . The metastasis to vulva occurred along with pulmonary metastasis a year after the management of primary by surgery and local radiation. The diagnosis in their case was made by PET-CT as the metastatic nodule was only 2x2cm and the diagnosis was confirmed by fine needle aspiration8 . The metastasis to ovary could not be diagnosed prior to laparotomy by fine needle aspiration in the present case. This is because FNAC has very high false negative rates in diagnosing cystosarcoma phylloids.10 Adjuvant therapy for management of metastatic Phylloids includes chemotherapy and Radiotherapy. Response to chemotherapy was observed in lung metastasis and abdominal metastasis but not in bone metastasis. Single agent and combined regimens have been used and response is long lasting with increase in progression free survival when Ifosfamide is used11. Radiotherapy has a role for loco regional control in recurrent benign as well as malignant Phylloids. However the control of primary tumour is important when metastasis had been taken care of to improve the survival rates as well as the quality of life.
The present case though she survived after laparotomy and complete removal of the large ovarian metastasis, she continued to suffer as the primary was not taken care of. Palliative surgery, chemotherapy and radiotherapy were deferred in the present case even after repeated discussions saying there is no role for surgery of primary in metastatic disease. But in this case the Ovarian metastasis was taken care of almost completely by surgery. Aggressive palliative surgery in metastatic Phylloids is reported to improve survival as well as quality of life. The physical and mental well being was improved after radical surgery for repeated recurrence that occurred twice . and this improved the nutritional status and immunity to undergo further treatment with chemotherapy7 .
The present case was unable to get up from the bed because of the weight of the tumour mass (breast) that progressed to large size and also because of poor nutritional status. Palliative breast surgery and palliative Radiotherapy under high risk consent may have improved her quality of life. A recent study which assessed the predictive factors for the local recurrence and distant metastasis of phylloides tumours of the breast in 192 cases concluded that histopathological type and margin status were independent predictors of distant metastasis- free survival and overall survival and it is essential to reduce the local recurrence to prevent distant metastasis.12
CONCLUSION Managing ovarian metastasis from cystosarcoma phylloids can be challenging and the quality of life is poor when the primary disease is not managed adequately. When an abdominal mass and a breast mass co-exist , metastasis from the breast mass to be considered as the first etiology rather than an association of different pathology until proved otherwise. Conflicts of Interests: None Sources of Funding: Nil
ACKNOLEDGEMENTS The authors acknowledge the immense help received from the scholars whose articles are cited and included in the manuscript. The authors are also greatful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Parker SJ, Harries SA, Phylloid tumours. Postgrad Med J 2001;77:428–435
2. Ang TL Leong Ng VW, Fock KM, Teo EK, Chong CK. JOP. J Pancreas 2007; 8(1):35-38.
3. Chen WH, Cheng SP, Tzen CY, Yang TL, Jeng KS, Liu CL, Liu TP. Surgical treatment of phyllodes tumors of the breast: retro-spective review of 172 cases. J Surg Oncol. 2005 ;91(3):185- 194.
4. Grimes MM. Cystosarcoma phyllodes of the breast: histologic features, flow cytometric analysis, and clinical correlations.Mod Pathol. 1992;5:323-329..
5. Palko MJ1 , Wang SE, Shackney SE, Cottington EM, Levitt SB, Hartsock RJ. Flow Cytometric S fraction as a predictor of clinical outcome in Cystosarcoma Phylloides. Arch Pathol Lab Med. 1990 Sep;114(9):949-52.
6. Bharat RJ Jr. Histologic features predict local recurrence after breast conservating therapy of Phylloid tumours.. Breast Cancer Res Treat. 1999 ;57(3):291-5.
7. Kapali AS, Singh M, Deo SVS, Shukla NK, Muduly DK. Aggressive palliative surgery in metastatic Phylloids tumor: Im pact on quality of life.Ind J Palliat Care. 2010; 16 (2):101-104.
8. Khangembam BC, Sharma P,Singla S,Shingal A,Dhull VS, Bal C,Kumar R. .Malignant Phylloides tumour of the Breast metastasing to the Vulva.18 F-FDG PET-CT demonstrating rare metastasis from a rare tumour Nucl Med Mol Imaging .2012 46:232–233
9. Hines JR, Gordan RT, Widger C, Kolb T.Cystosarcoma Phylloids metastatic to a Brenner tumour of the ovary. Arch Surg 1976;111(3):299-300.
10. Jacklin RK, Ridgway PF,. Ziprin P,, Healy V, Hadjiminas D, and . Darzi A, “Optimising preoperative diagnosis in phyllodes tumour of the breast,”. J Clin Pathol, 2006; 59(5):454–459.
11. Hawkins RE,Wiltshaw E,Fisher C McKinna JA..Ifosphamide is an active drug for chemotherapy of metastatic Cystosarcoma Phylloides.Cancer.1992;69:2271-2275.
12. Wei J,Tan Yu-T, Cai Yu C, Yuan Z-Yu, Yang D, Wang SS.Predictive factors for local recurrence and distant metastasis of Phylloides tumours of the breast: a retrospective analysis of 192 cases at a single centre. Chin J Cancer; 2014; 33 (10):492- 500.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License