IJCRR - 11(11), JUNE, 2019
Pages: 05-10
Date of Publication: 10-Jun-2019
Print Article
Download XML Download PDF
Combined Effectiveness of Mirror Therapy and Motor Imagery on Gait in Stroke Patients
Author: Neha Hatwar, Suchetha PS, Dhanesh Kumar KU
Category: Healthcare
Abstract:Aim: The purpose of the study was to evaluate the combined effectiveness of lower limb mirror therapy and motor imagery on gait in stroke patients.
Methods: A total number of 38 patients were recruited for the study. They were divided into two groups: Group A (n=19) and Group B (n=19). Group A was given motor imagery and conventional rehabilitation while Group B was given lower limb mirror therapy, motor imagery, and conventional rehabilitation. The interventions were given for 2weeks (5days/week). The values of Dynamic Gait Index (DGI) and Lower limb component of Fugl Meyer Assessment (FMA-LE) were taken both at baseline and after 2 weeks of intervention.
Result: Both Group A and Group B showed significant improvements in DGI and FMA-LE after 2 weeks of intervention (p value< 0.001). The comparison of DGI difference between the two groups did not show a statistically significant difference (p value=0.09). Also, comparison of FMA-LE difference between the two groups did not show a statistically significant difference (p value=0.412)
Conclusion: Based on the above results it can be concluded that the combination of mirror therapy with motor imagery is equally effective as motor imagery alone in improving gait and function in stroke patients.
Keywords: Gait disturbances, Mirror Therapy, Motor Imagery, Stroke
Full Text:
INTRODUCTION
According to WHO, stroke is defined as ‘rapidly developing clinical signs of focal (or global) disturbance of cerebral function, lasting more than 24 hours or leading to death, with no apparent cause other than the vascular origin [1]. It is one of the leading causes of disability in India, the prevalence being 84-262/100000 in rural and 334-424/100000 in urban areas[2].
It is estimated that nearly 80% of stroke patients have an upper limb or lower limb functional deficit[3]. The inability to walk properly due to lower limb impairment is a major problem confronted by many stroke patients [4].
The common abnormal gait patterns seen in stroke patients are circumduction, genu recurvatum, and spastic paretic stiff-legged gait. The deviations include decreased gait speed, decreased cadence, decreased stride length, increased step width and increased time spent in double limb support compared to healthy adults [5].
Gait restoration is one of the major goalsin post-stroke rehabilitation.For the planning of appropriate rehabilitation, the mechanism behind gait control should be understood. Spinal cord (central pattern generators) initiates rhythmic walking and the voluntary modifications are made by the cerebral cortex. In stroke patients, the cerebral cortex function is disrupted while that of the spinal cord is protected. Thus, the ability of the spinal cord of producing rhythmic walking can be used to reorganize the cerebral cortex to improve walking ability in post-stroke patients[6]. Mirror therapy and motor imagery are such methods which help in reorganizing the motor cortex.
Mirror therapy is a type of intervention which creates a reflection of the non-affected limb by using a mirror to trick the brain to think that movement has occurred in the affected extremity[3]. Mirror therapy is based on the principle of visual illusion. Mirror therapy works by activating the ipsilateral motor cortex and the premotor and sensorimotor areas which control contralateral movements. This enhances communication between the hemispheres and results in appropriate motor recovery. Mirror therapy has proved to be effective for the recovery of the upper limb after stroke. Studies regarding the effectiveness of mirror therapy on lower limb recovery after stroke are few[7].
Motor imagery is a type of therapy in which the patient rehearses the movement without actually performing it[8]. More recovery is seen when motor imagery is followed by the performance of physical activities. Systematic reviews done earlier have demonstrated that motor imagery enhances upper extremity functions in stroke patients. Recently motor imagery associated with lower limb functions has also been investigated and is found to be effective[9].
The retrieved works of literature have proved that mirror therapy and motor imagery are effective in improving the motor functioning of the upper limb and lower limb after
stroke[3,8]. Mirror therapy and motor imagery are proved to be effective in improving gait function when given isolation[10,11]. Though, there are several studies done on the use of mirror therapy on upper limb function in a stroke patient, very few studies done on the effectiveness of lower limb mirror therapy. Also, there is paucity in the literature on the combined effect of mirror therapy and motor imagery on gait in post-stroke patients. Therefore, this study has been taken up to evaluate whether mirror therapy has additional effectiveness combined with motor imagery in the improvement of post-stroke gait.
METHODOLOGY
Approval from the scientific committee and institutional ethics committee was obtained before the commencement of the study. Participants with stroke were recruited from Justice K S Hegde charitable hospital, Mangalore. These participants were screened based on inclusion criteria and consent was taken from selected participants. The participants were included based on the following criteria: a) Patients who are less than 6 months post-stroke b) Age- 45-65 years c) Ability to walk with minimal assistance (functional ambulation category less than or equal to 3.) d) No remarkable cognitive deficit (an outcome more than 25 on mini-mental status examination). The exclusion criteria were: a) Any musculoskeletal disorder impeding lower limb functionb)Any neglect of space on the affected side, or any other neurological disease or auditory or visual c) Any psychiatric disorders.
The participants were divided into two groups. Group A was given 15 minutes of mirror therapy,15 minutes of motor imagery and 30 minutes of conventional treatment whileGroup B was given 15 minutes of motor imagery and 45 minutes of conventional treatment. The interventions were given for 2 weeks (5 days a week). Fugl Meyer assessment of lower extremity (FMA-LE) and Dynamic Gait Index (DGI) values were taken at baseline and after 2 weeks of intervention (Figure 1).
In mirror therapy, the patient was made to sit and a mirror was mounted in between the legs of the patient in such a way that the paretic leg was on the non-reflective side of the mirror while the non-paretic limb was facing the reflective side of the mirror. The patient was made to perform the following exercises using the non-paretic leg (Figure 2 and 3):
Components of gait which were missing were focussed more.
In motor imagery therapy, the patient was made to sit on a chair with eyes closed in a quiet room. He was then made to listen to motor imagery scripts through headphones. The patients were made to imagine all gait specific lower limb movements (Figure 4). The scripts were recorded in local languages.
Conventional treatment was given according to patient’s requirements which included stretching, active and passive range of motion exercises, weight bearing, balance and coordination exercises.
RESULTS
SPSS software version 16.0. was used to assess the data obtained. To compare the pre and post measurements for Dynamic Gait Index(DGI) andFugl Meyer Assessment -lower extremity (FMA-LE), paired ‘t' test was used for group A and Group B. To compare the effectiveness of intervention between two groups, independent sample ‘t' test was used. The p-value less than 0.05, was regarded as significant for the study.
The comparison of age distribution between the two groups was done using the independent t-test. The mean age for group A is 57.42±8.03 and for group B is 52.95±9.16.The p-value is 0.118 which is not statistically significant. Hence, age was homogenously distributed (Table1)
The comparison of gender distribution between group A and group B was done utilizing chi-square test. The p-value is 0.118 which is not statistically significant. Hence, gender was homogenously distributed between the two groups (Table 2).
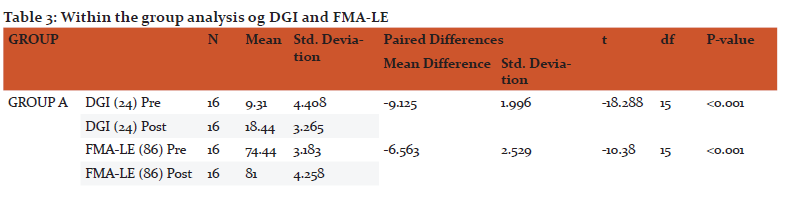
Within the group analysis for the outcome measures DGI and FMA-LE was done using a paired t-test (Table3)
For Group-A, Pre DGI, mean value is 9.31±4.40 and Post DGI mean value is 18.84±3.26. On comparison of the mean values of Pre DGI and Post DGI, the mean values of Post DGI are higher with a difference of 9.125. The p-value is less than 0.001 which is statistically significant. Pre FMA-LE mean value is 74.44±3.18 and Post FMA-LE mean value is 81±4.25.On comparison of the mean values of Pre FMA-LE and Post FMA-LE, the mean values of Post FMA-LE are higher with a difference of 6.563 and the p-value is less than 0.001 which is statistically significant.
For Group-B, Pre DGI mean value is 18±10.11 and Post DGI mean value is 18±21.28. On comparison of the mean values of Pre DGI and Post DGI, the mean values of Post DGI are higher with a difference of 11.167 and the p-value is less than 0.001 which is statistically significant.Pre FMA-LE mean value is 75.67±4.39 and Post FMA-LE mean value is 83.06±3.94. On comparison of the mean values of Pre FMA-LE and Post FMA-LE, the mean values of Post FMA-LE are higher with a difference of 7.389 and the p-value is less than 0.001 which is statistically significant.
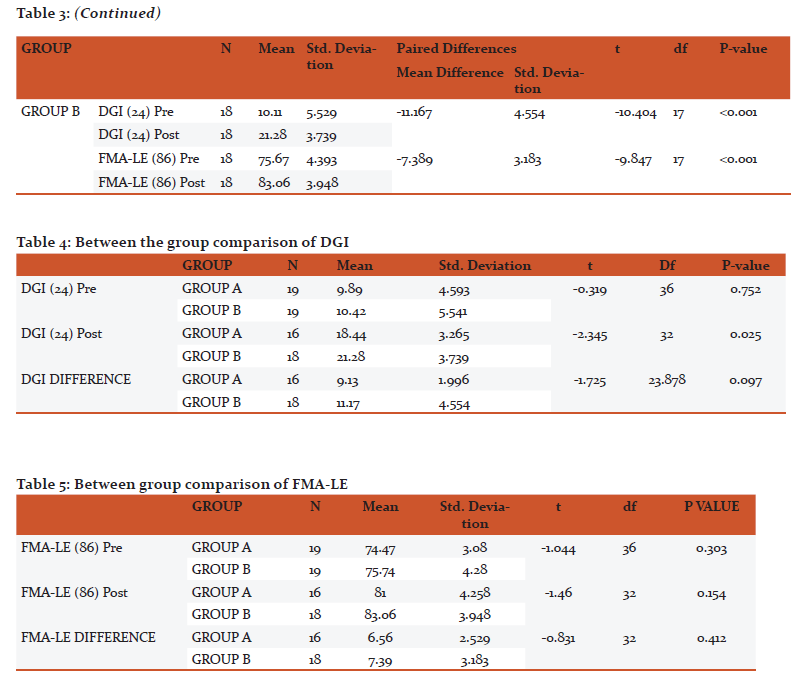
Between the group comparison for DGI was done using an independent t-test (Table 4).
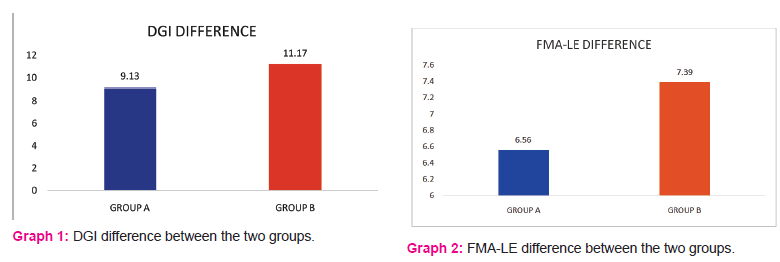
Comparison of the Pre DGI between the two groups shows that Pre DGI is higher in group B (mean=10.42±5.54) with a t value of -0.319. The p-value is 0.752 which is not statistically significant.A comparison of the Post DGI between the two groups shows that Post DGI is higher in group B (mean=21.28±3.73) with a t value of -2.345. The p-value is 0.025 which is statistically significant. A comparison of the DGI difference between the two groups shows that DGI difference is higher in group B (mean=11.17±4.55) with a t value of -1.725. The p-value is 0.097 which is not statistically significant (Graph 1)
Between group comparison for FMA-LE was done using independent t-test (table 5).
Comparison of the Pre FMA-LE between the two groups shows that Pre FMA-LE is higher in group B (mean=75.54±4.28) with a t value of -1.044. The p-value is 0.303 which is not statistically significant. Comparison of the Post FMA-LE between the two groups shows that Post FMA-LE is higher in group B (mean=83.06±3.94) with a t value of -1.46. The p-value is0.154 which is not statistically significant. A comparison of the FMA-LE difference between the two groups shows that the FMA-LE difference is higher in group B (mean=7.39±3.18) with a t value of -0.831. The p-value is 0.412 which is not statistically significant (Graph 2).
DISCUSSION
Cerebrovascular accidents or stroke may occur either due to blood clots which impair blood flow to the brain or any trauma which ruptures the blood vessels causing leakage of blood around the brain. It can adversely disrupt the functioning of the limbs which in turn causes restriction of activity and participation in day to day life. Disability caused by stroke may persist lifelong if proper rehabilitative measures are not taken.
In the present study, Group A received only motor imagery for lower limbs while group B received both motor imagery and mirror therapy for lower limbs for 2 weeks.
Previously, studies have been done in which mirror therapy was combined with other forms of therapies such as action observation therapy, neuromuscular electrical stimulation. Lee et al suggested that action observation therapy and mirror training with conventional rehabilitation significantly improved patient’s gait[12]. Xu et al demonstrated that mirror therapy combined with neuromuscular electrical stimulation caused improvement in spasticity and walking ability of stroke patients[13]. No study is being done till now combining mirror therapy with motor imagery. So, this study was taken up.
In group A (MI), there was significantly improved both gait and motor function of lower limbs after 2 weeks of intervention. Both DGI and FMA-LE showed statistically significant differences (p-value <0.001) after within the group analysis.
In group B (MI+MT) also, a statistically significant difference was seen in both DGI and FMA-LE values (p-value <0.001) after 2 weeks of intervention after within group analyses.Thus, motor imagery alone or with combination with mirror therapy improved gait and lower limb function in post-stroke patients.
The improvement which is seen in motor function and gait by motor imagery is supported by Lacourse et al, who suggested that the cortical and subcortical motor areas are simultaneously activated during motor imagery learning which indicates that motor imagery is effective in rehearsing and learning skilled movements[14].
Also, Oostra et al suggested that motor imagery may have a beneficial effect on enhancing gait function in sub-acute stroke which is matching the results of this study; however, longer-term confirmation is required[11]. However, a meta-analysis done by Guerra et al reported a high heterogeneity in methodological quality of the included randomized control studies and con?icting results. They concluded that more high-quality studies and greater standardization of interventions are needed to determine the value of motor imagery for persons with stroke[15].
Improvements which are seen in gait and function due to mirror therapy are supported by Arya et al, who demonstrated that activity-based mirror therapy accelerates lower limb motor recovery and reduces gait deviations amongst chronic poststroke subjects[7].
A systematic review by Li et al demonstrated that the use of mirror therapy in addition to some form of rehabilitation appeared promising for some areas of lower limb function, which is similar to the results obtained in this study, but there is no sufficient evidence to suggest when and how this therapy should be given[16].
In the present study, when the DGI difference was compared between the two groups, it was found that the DGI difference was higher in group B (mean=11.17±4.55) than group A (mean=9.13±1.99). But the difference was not statistically significant (p value=0.097>0.005). Also, when the FMA-LE difference was compared between the two groups, it was found that FMA-LE difference was higher in group B (mean=7.39±3.18), than group A (mean=6.56±2.5). But the difference was not statistically significant (p value=0.412>0.005). Hence, it can be concluded that the combination of mirror therapy with motor imagery has not caused any additional improvement on gait and lower limb function in stroke patients. Thus, it can be inferred that the combination of mirror therapy with motor imagery is equally effective as motor imagery alone in improving gait and function in stroke patients.
CONCLUSION
The present study demonstrates that motor imagery combined with mirror therapy improved gait and lower limb function in stroke patients. Also, motor imagery alone improved gait and lower limb function in post-stroke patients. When the results of both the groups were compared with each other, there was no statistically significant difference. But on comparing the mean difference of both the groups, motor imagery combined with mirror therapy was superior to motor imagery alone.
Hence, it can be inferred that the combination of mirror therapy with motor imagery is equally effective as motor imagery alone in improving gait and function in stroke patients.
LIMITATIONS
-
The study had a small sample size
-
The intervention period was only for two weeks
-
long term follow up was not taken
SCOPE FOR FUTURE WORK
-
A similar kind of study can be carried out with large sample size. Also, the interventions can be given for a longer period.
-
A follow-up study can be conducted to determine the long-term effects of the interventions.
-
Further studies can be conducted comparing mirror therapy with motor imagery
SOURCES OF FUNDING
Nil
CONFLICTS OF INTEREST
None

References:
-
Sacco R, kasner S, Broderick J, Caplan L, Culebras A, Elkind M et al. An Updated Definition of Stroke for 21st Century. A Statement for Health Care Professionals from the American Heart Association/American Stroke Association.Stroke. 2013;44:2064-89.
-
Pandian J, Sudhan P. Stroke Epidemiology and Stroke Care Services in India. J Stroke. 2013;15(3):128-34.
-
Thieme H, Mehrholz J, Pohl M, Behrens J, Dohle C. Mirror Therapy for Improving Motor Function After Stroke. Stroke. 2012;44(1):e1-e2.
-
Beyaert C, Vasa R, Frykberg G. Gait post-stroke: Pathophysiology and rehabilitation strategies. Clin Neurophysio. 2015;45(4-5):335-55.
-
Oh Y, Kim H, Woo Y. Effects of Rhythmic Auditory Stimulation Using Music on Gait With Stroke Patients. Phys Ther Korea. 2015;22(3):81-90.
-
Verma R, Arya K, Sharma P, Garg R. Understanding gait control in post-stroke: Implications for management. J Body Mov Ther. 2012;16(1):14-21.
-
Arya K, Pandian S, Kumar V. Effect of activity-based mirror therapy on lower limb motor-recovery and gait in stroke: A randomized controlled trial. NeuropsycholRehabil. 2017;1-18.
-
García D, Aboiti J. Effectiveness of motor imagery or mental practice in functional recovery after stroke: a systematic review. Neurología. 2016;31(1):43-52.
-
Li R, Li Z, Tan J, Chen T, Lin W. Effects of motor imagery on walking function and balance in patients after stroke: A quantitative synthesis of randomized control trials. Complement Ther Clin Pract. (2017); 28:75-48.
-
Ji S, Kim M. The effects of mirror therapy on the gait of subacute stroke patients: a randomized controlled trial. Clin Rehabil. 2014;29(4):348-54.
-
Oostra K, Oomen A, Vanderstraeten G, Vingerhoets G. Influence of motor imagery training on gait rehabilitation in sub-acute stroke: A randomized controlled trial. J Rehabil Med. 2015;47(3):204-09.
-
Lee H, Kim Y, Lee D. The effects of action observation training and mirror therapy on gait and balance in stroke patients. J Phys Ther Sci. 2017;29(3):523-26.
-
García D, Aboiti J. Effectiveness of motor imagery or mental practice in functional recovery after stroke: a systematic review. Neurología. 2016;31(1):43-52.
-
Lacourse M, Orr E, Cramer S, Cohen M. Brain activation during execution and motor imagery of novel and skilled sequential hand movements. NeuroImage. 2005;27(3):505-19.
-
Guerra Z, Lucchetti A, Lucchetti G. Motor Imagery Training After Stroke. J Neurol Phys Ther. 2017;41(4):205-14.
-
Li Y, Wei, Q, Gou W, He C. Effects of mirror therapy on walking ability, balance and lower limb motor recovery after stroke: a systematic review and meta-analysis of randomized controlled trials. Clin Rehabil. 2018;32(8):1007-21
-
Sacco R, kasner S, Broderick J, Caplan L, Culebras A, Elkind M et al. An Updated Definition of Stroke for 21st Century. A Statement for Health Care Professionals from the American Heart Association/American Stroke Association.Stroke. 2013;44:2064-89.
-
Pandian J, Sudhan P. Stroke Epidemiology and Stroke Care Services in India. J Stroke. 2013;15(3):128-34.
-
Thieme H, Mehrholz J, Pohl M, Behrens J, Dohle C. Mirror Therapy for Improving Motor Function After Stroke. Stroke. 2012;44(1):e1-e2.
-
Beyaert C, Vasa R, Frykberg G. Gait post-stroke: Pathophysiology and rehabilitation strategies. Clin Neurophysio. 2015;45(4-5):335-55.
-
Oh Y, Kim H, Woo Y. Effects of Rhythmic Auditory Stimulation Using Music on Gait With Stroke Patients. Phys Ther Korea. 2015;22(3):81-90.
-
Verma R, Arya K, Sharma P, Garg R. Understanding gait control in post-stroke: Implications for management. J Body Mov Ther. 2012;16(1):14-21.
-
Arya K, Pandian S, Kumar V. Effect of activity-based mirror therapy on lower limb motor-recovery and gait in stroke: A randomized controlled trial. NeuropsycholRehabil. 2017;1-18.
-
García D, Aboiti J. Effectiveness of motor imagery or mental practice in functional recovery after stroke: a systematic review. Neurología. 2016;31(1):43-52.
-
Li R, Li Z, Tan J, Chen T, Lin W. Effects of motor imagery on walking function and balance in patients after stroke: A quantitative synthesis of randomized control trials. Complement Ther Clin Pract. (2017); 28:75-48.
-
Ji S, Kim M. The effects of mirror therapy on the gait of subacute stroke patients: a randomized controlled trial. Clin Rehabil. 2014;29(4):348-54.
-
Oostra K, Oomen A, Vanderstraeten G, Vingerhoets G. Influence of motor imagery training on gait rehabilitation in sub-acute stroke: A randomized controlled trial. J Rehabil Med. 2015;47(3):204-09.
-
Lee H, Kim Y, Lee D. The effects of action observation training and mirror therapy on gait and balance in stroke patients. J Phys Ther Sci. 2017;29(3):523-26.
-
García D, Aboiti J. Effectiveness of motor imagery or mental practice in functional recovery after stroke: a systematic review. Neurología. 2016;31(1):43-52.
-
Lacourse M, Orr E, Cramer S, Cohen M. Brain activation during execution and motor imagery of novel and skilled sequential hand movements. NeuroImage. 2005;27(3):505-19.
-
Guerra Z, Lucchetti A, Lucchetti G. Motor Imagery Training After Stroke. J Neurol Phys Ther. 2017;41(4):205-14.
-
Li Y, Wei, Q, Gou W, He C. Effects of mirror therapy on walking ability, balance and lower limb motor recovery after stroke: a systematic review and meta-analysis of randomized controlled trials. Clin Rehabil. 2018;32(8):1007-21
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License