IJCRR - 11(7), April, 2019
Pages: 09-11
Date of Publication: 12-Apr-2019
Print Article
Download XML Download PDF
Relapsing Polychondritis with Seronegative Spondyloarthritis: A Rare Case Report
Author: Archana U., Raju H. B., Sreedhar J., Jyoti H., Shama B., Abhiram M., Rishab A., Rajani D.
Category: Healthcare
Abstract:The aim of this paper is to present a case of relapsing polychondritis and response to cyclophosphamide pulse therapy. A 19 years old female patient presented with inflammatory back pain, asymmetrical oligoartheritis and acute anterior uveitis. CT thorax revealed edema in the glottis and trachea causing narrowing of lumen. Based on the investigations and clinical finding a final diagnosis of relapsing polychondritis was done and started with 5 pulse of cyclophosphamide which showed improvement. Relapsing polychondritis is a rare condition commonly affecting 40-50 years age group. But can be seen in younger age too in both the sexes. Laryngobronchial involvement occurs in approximately 50% of patients, and is among the most serious complications. Here we present the case of a 19 year old female with relapsing polychondritis presenting with stridor due to tracheal involvement.
Keywords: Relapsing Polychondritis, Cyclophosphamide
Full Text:
INTRODUCTION
Relapsing polychondritis is an uncommon disease with an incidence of about 3.5 cases per million population per year. The peak age of onset is between the ages of 40 and 50 years. But relapsing polychondritis may affect both children and the elderly, and affects both sexes equally. Approximately 30% of patients with relapsing polychondritis will have another rheumatologic disorder, the most frequent is systemic vasculitis, followed by rheumatoid arthritis and systemic lupus erythematosus. Diagnosis is based on typical clinical features. McAdam et al. proposed a diagnostic criteria in 1976, which was further modified by Damiani and Levine in 1979.
McAdam et al, proposed the following:-
-
Recurrent chondritis of both auricles
-
Nonerosive inflammatory arthritis
-
Chondritis of nasal cartilage
-
Inflammation of ocular structures, including conjunctivitis, keratitis, scleritis/episcleritis, and/or uveitis
-
Chondritis of laryngeal and/or tracheal cartilages
-
Cochlear and/ or vestibular damage manifested by neurosensory hearing loss, tinnitus, and/or vertigo
Diagnosis is certain when 3 or more of these features are present along with a positive biopsy from the ear, nasal or respiratory cartilage1.
Damiani and Levine later suggested that the diagnosis could be made when;
-
One of the features and a positive biopsy
-
Two or more separate sites of cartilage involvement present that responded to glucocorticoids or dapsone
-
Three or more of the features mentioned were present.
We are reporting the case of a 19 year old female, who presented with inflammatory arthritis and uveitis, and later developed hoarseness of voice and an acute episode of choking.
CASE REPORT
A 19 year old female presented with symptoms suggestive of inflammatory back pain, asymmetric oligoarthritis along with acute anterior uveitis. MRI pelvis showed evidence of bilateral sacroilitis and she tested negative for Human Leukocyte Antigen B27 (HLAB27). Treatment was initiated with Non steroidal Anti-inflammatory Drugs (NSAIDs) and Sulfasalazine, further in view of lack of response to treatment, the patient was started on Infliximab therapy after a thorough work up. Following the commencement of Infliximab therapy, the joint pains subsided but, developed hoarseness of voice soon after the 1st pulse. In view of hoarseness of voice, an ENT opinion was taken, and the patient was put on steroids considering it to be Reinke’s edema, symptomatic improvement in hoarseness of voice was noted. Upon tapering steroids, the hoarseness of voice returned. In view of relapse of symptoms, an endocrinology opinion was taken to look for an endocrinologic cause for hoarseness, and following thorough evaluation, any endocrinological cause was ruled out.
Three pulses of Infliximab were completed (as per protocol). Later the patient developed an acute choking episode at her college, wherein she was referred to a local hospital and subsequently intubated, and further referred to our hospital. After admission to our hospital, and stabilization of the patient, she was extubated. General physical examination at this juncture revealed a depressed nasal bridge, and tenderness over the larynx. There was no evidence of chondritis of auricles, and no history of any previous episodes of the same. No history suggestive of cochlear or vestibular involvement was elicited. No features suggestive of vasculitis were noted.
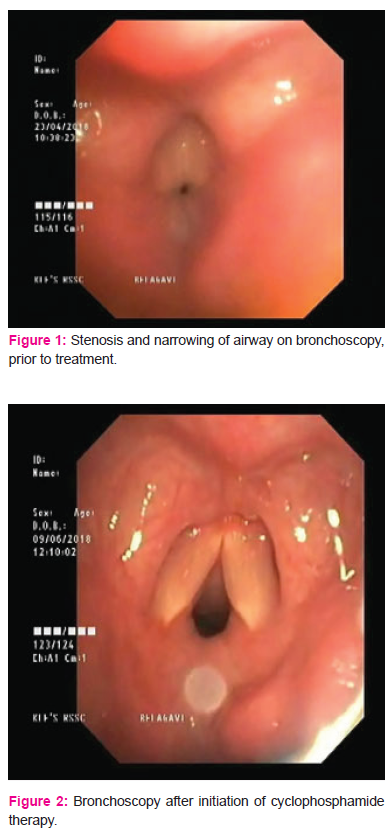
With the suspicion of Relapsing Polychondritis, the patient was subjected to a CT Thorax/Neck which revealed edema in the glottis region and trachea from C6 to D5, causing luminal narrowing. A respiratory medicine opinion was taken and a bronchoscopy performed. The bronchoscopy showed severe narrowing of the tracheal lumen. A 2 Dimensional Echocardiogram (2DECHO) performed showed anterior mitral leaflet prolapse. Positron Emission Tomography- Computed Tomography (PET CT) done, showed increased uptake in the tracheal and laryngeal cartilage.
Based on these clinical findings a diagnosis of Relapsing Polychondritis was made. She was started on Cyclophosphamide pulse therapy under the cover of Luperolide, to prevent gonadal toxicity. A repeat bronchoscopy was performed after 5 pulses of cyclophosphamide which showed improvement. A follow up CT scan showed narrowing at C4 level with no signs of edema. Currently the patient is on regular follow up on an outpatient basis, the cyclophosphamide pulses have been tapered, and her condition is stable, with no further episodes of acute respiratory distress.
DISCUSSION
Relapsing polychondritis is a systemic disease causing inflammation of cartilaginous structures in multiple organs2
Approximately one-third of patients with relapsing polychondritis suffer from another underlying autoimmune disease such as systemic vasculitis. There is genetic risk for relapsing polychondritis, as suggested by its association with Human Leukocyte Antigen- DR4 isotope (HLA-DR4), which is associated with multiple autoimmune diseases such as rheumatoid arthritis, multiple sclerosis and others. It is suggested that in RP there are circulating antibodiesagainst type II collagen, which leads to cell-mediated injury to targeted organs in the diseaseprocess3.
Clinical phenotypes of relapsing polychondritis follow two patterns; either nasal cartilage/airway involvement or external ear involvement4. Typically, auricular chondritis occurs in almost 90% of the patients5. However, as demonstrated in our patient, its absence does not rule out the diagnosis of relapsing polychondritis.The respiratory tract is affected in more than 50% of the cases5. Respiratory disturbance results from airway collapse secondary to destruction of tracheal rings or narrowingof the tracheal lumen caused by fibrous or inflammatory edema. Airway manifestations are the commonest cause of morbidity and mortality in the disease6. The management of respiratory tract involvement in relapsing polychondritis is important because sudden respiratory arrest mayoccur5, as manifested by an acute episode of choking in our patient. Failure of early diagnosis of airway involvement in relapsing polychondritis can lead to irreversible cartilage damage. Steroids or other immunosuppressants are ineffective in these advanced cases, and would require airway interventions such as tracheostomy or tracheobronchial stents6.
There is no current standard treatment for relapsing polychondritis, owing in part to its rarity. Corticosteroids are considered to be the first line treatment.6 Steroid sparing agents, such as cyclophosphamide, azathioprine, methotrexate and cyclosporine are also found to be helpful. Our patient achieved remission following cyclophosphamide pulse therapy.
CONCLUSION
Relapsing Polychondritis, is a rare condition, which can present without the classical symptom of auricle chondritis, and as involvement of the laryngotracheobronchial tree alone. In the absence of any specific diagnostic test, a high degree of clinical suspicion is required to arrive at the diagnosis. Recognition and prompt treatment of the airway symptoms of relapsing polychondritits, is beneficial so as to avoid the more invasive airway interventions at more advanced stages of the disease.
Conflict of interest: None
References:
-
Harrison’s Principles of Internal Medicine, 20th Edition, Chapter 359, Page no 2597-600
-
Ferrada MA, Grayson PC, Banerjee S et al. Patient-perceptionof disease-related symptoms and complications in relapsing polychondritis. Arthritis Care Res 2017; Advance Access published 15 December 2017, doi: 10.1002/acr.23492.
-
Maha Almackenzie, Ahmad Alharbi, Sharifa Alhassan, Eleanor Cook and Nezam Altorok, Central Nervous System Vasculitis Associated with Relapsing Polychondritis, Successful Treatment with Cyclophosphamide, The American Journal of the Medical Sciences, http://dx.doi.org/10.1016/j.amjms.2016.11.023.
-
Shimizu J, Yamano Y, Yudoh K, Suzuki N. Organ involvementpattern suggests subgroups within relapsing polychondritis: comment on the article by Dion et al. Arthritis Rheumatol 2018;70:1489
-
Vito Sabato, Olivier M Vanderveken, Tim Van den Wyngaert, Carl Van Laer & Didier Ebo (2016): A patient with a severe glottic stenosis and saddle nose, Acta Clinica Belgica, DOI: 10.1080/17843286.2015.1111657
-
Gorard C, Kadri S. Critical airway involvement in relapsing polychondritis. BMJ Case Rep. 2014; 2014. Published 2014 Sep 11. doi:10.1136/bcr-2014-205036
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License