IJCRR - 11(5), March, 2019
Pages: 01-05
Date of Publication: 14-Mar-2019
Print Article
Download XML Download PDF
Chronic lymphocytic leukemia \-Internationa Prognostic Index for Macedonian Patients with Chronic Lymphocytic Leukemia
Author: Trajkova S., Cevreska L., Ivanovski M., Popova-Labacevska M., Pivkova-Veljanovska A., Panovska-Stavridis I.
Category: Healthcare
Abstract:Introduction: Several prognostic factors have been identified to predict the outcome of patients with Chronic lymphocytic leukemia(CLL), but only a few studies investigated more markers together. To predict the time to first treatment (TFT) we integrated the data of traditional staging system, cytogenetic aberrations, and mutational status of immunoglobulin heavy chain variable region (IGHV) in Chronic lymphocytic leukemia\? Internationa Prognostic Index(CLL-IPI).
Aim of the study: To validate the prognostic value of chronic lymphocytic leukemia-international prognostic index (CLL-IPI) for Macedonian CLL patients.
Material and Methods: The study is set up retrospectively and includes 75 patients with CLL diagnosed and treated at the University Clinic of Hematology for a period of time from January 2011 to January 2018. The median follow-up was 36 months (1-72 months).We recognized the prognostic markers of TFT,in line of definition that prognostic markers we incorporated the data of Rai staging system, most adverse cytogenetic marker and mutational status of immunoglobulin heavy chain.
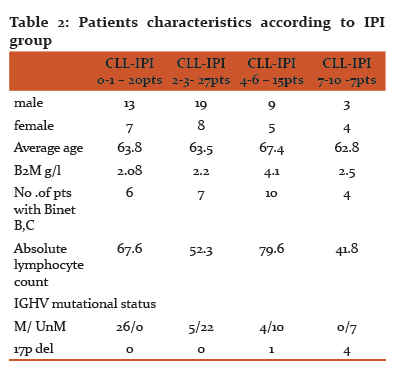
Results: The statistical data of the 75 patients shows that58.7% were males and 41.3% were females, with a median age of 64.3 (42-85) years old. The median TFS for low CLL-IPI (n=20), intermediate CLL-IPI (n=27), high risk CLL-IPI (n=15) and very high risk group (n=7) according to the CLL-IPI scoring system was 7.9, 7.6, 7.0 and 5.8 months, respectively. The median OS for low risk group was 58.5 for intermediate, high, and very high risk group was 37.8, 34.6 and 30 months, respectively. The estimated 5-year OS rate was 98.7%, 92%, 40% and 33%, respectively for low risk group intermediate, high, and very high risk group. Multivariate analysis indicated that del 17p (P< 0.00874) was independent prognostic factors of TFS.
Conclusions: CLL-IPI is the powerful tool for risk stratification in Macedonian CLL patients and this system also provided treatment recommendations for the different patient risk subgroup.Though, it is unknown how newly developed CLL therapies and newly identified prognostic and predictive markers would be merged into this revised staging system.
Keywords: Leukemia, Lymphocytic, Chronic, Prognosis
Full Text:
INTRODUCTION
Chronic lymphocytic leukemia (CLL) is the most common type of adult leukemia in Western countries. In Macedonia, with the aging of the population and the increasingly westernized lifestyle, the incidence rate is increasing year by year. The median survival of CLL patients is approximately 10 years, but the prognosis of different patients is highly heterogeneous. One group of patients can implement the "watch and waiting" strategy and have no treatment indication for life, but one third of the patients need treatment at the time of diagnosis, and only few patients turn into invasive lymphoma with a very poor prognosis. The traditional clinical staging systems Rai and Binet, based only on physical examination and laboratory findings do not include new implemented prognostic markers like TP53 deletion and immunoglobulin heavy chain variable region (IGHV) genes. Mutation status of IGHV and molecular markers have strong prognostic significance of CLL. Understanding the biology of the disease, most patients are at the early stage of diagnosis at the time of diagnosis, so the prognosis of patients with Rai and Binet clinical judgment system has become incomplete. Therefore, a new prognostic system is needed for accurate prognostic stratification of CLL.
The international group of researchers conducted a literature search for phase II and phase III clinical trials of CLL published in a pediod of time from January 1. 1950 to December 31. 2010, including eight prospective trials in their analyses. In total, the studies included 3.473 treatment-naïve patients at both early and advanced CLL stages (median age, 61 years; range, 27-86 years) from France, Germany, Poland, the United Kingdom, and the United States. Patients were followed for a median of 80 months (1).
The researchers externally validated the model in two additional datasets: a cohort from the Mayo Clinic in Rochester, Minnesota (n=838), and the SCALE Scandinavian population-based case-control study (n=416). Mean patient age in these cohorts was 62 years (range = 25-89 years), and these patients were followed for a median of 63 months (1).
From the group of 27 baseline factors the CLL-IPI researchers examined in the training dataset, five emerged as independent prognostic markers for overall survival (OS):
-
TP53 status (no abnormalities vs. del17p, TP53 mutations, or both)
-
IGHV mutational status (mutated vs. unmutated)
-
Serum ß2-microglobulin (B2M) concentration (≤3.5 mg/L vs. >3.5 mg/L)
-
Clinical stage (Binet A or Rai 0 vs. Binet B-C or Rai I-IV)
-
Age (≤65 years vs. >65 years)
Each variable was then assigned an individual weight. The researchers then added all of these factors together, derived a prognostic score ranging from 0-10, and identified four risk groups with significantly different rates of OS at five years (p<0.001 for all):
-
Low-risk patients (score = 0-1): 93.2% (95% CI 90.5-96.0)
-
Intermediate risk (score = 2-3): 79.3% (95% CI 75.5-83.2)
-
High risk (score = 4-6): 63.3% (95% CI 57.9-68.8)
-
Very-high risk (score = 7-10): 23.3% (95% CI 12.5-34.1)
We conducted this study, to validate the prognostic value of chronic lymphocytic leukemia-international prognostic index (CLL-IPI) for Macedonian CLL patients.
2. MATERIAL AND METHODS
2.1 Patients and specimens
The study was set up as retrospective and involved 75 patients with CLL diagnosed and treated at the University Clinic for Hematology for a period of for a period of time from January 2011 to January 2018. The median follow-up was 36 months (1-72 months). The study was conducted at the University Clinic for Hematology in Skopje.
The diagnosis of patients with CLL was set according to the recommendations of the International Working Group on CLL (IWCLL)(2).
All the patients were evaluated for traditional clinical and laboratory prognostic factors and newer prognostic factors including IGHV mutation status and deletion 17p/TP53 mutation. Prognostic factors were evaluated at patients’ first visit to the University Clinic for Haematology. This was done to develop a model that best correlated with time to first treatment for patients who do not have an indication for treatment at the time of evaluation. Clinical and laboratory evaluation at the first visit to the University Haematology Clinic included history and physical examination, standard clinical laboratory evaluation, and evaluation for molecular markers. Traditional prognostic factors and clinical and laboratory variables included sex; age, Rai stage, physical examination with evaluation of number of involved lymph node sites (cervical, axillary, and inguinal), measurement of liver and spleen size, white blood cell count (WBC), absolute lymphocyte count (ALC), haemoglobin level, platelet count, Beta-2 microglobulin (B-2M). IGHV mutation status and deletion 17p/TP53 mutation were characterized by the direct sequencing method. Patients were categorized as unmutated (IGHV ≥ 98% germline homology) or mutated (< 98% homology) .IGHV mutation status and detection of deletion 17p/TP53 mutation performed by the Center for Biomolecular Pharmaceutical Analyses at the Faculty of Pharmacy.
3. Results
3.1. Patient’s Characteristics
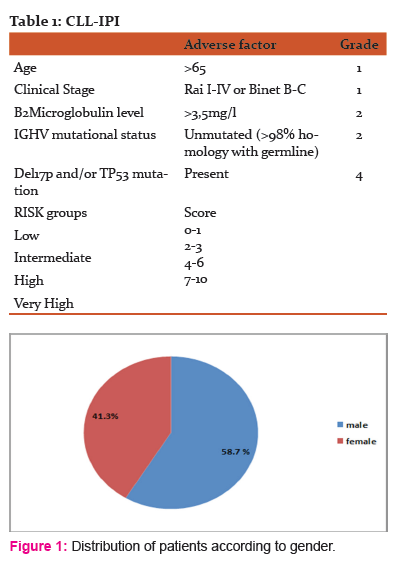
We analyzed data of 75 CLL patients, diagnosed and treated at University Clinic for Hematology within 12 months of diagnosis and who had complete data available for all parameters used to calculate the prognostic index score. According to gender distribution there was male predomination, 58.7% were males and 41.3% were females, with a median age of 64.3 (42-85) years old (figure1). To validate the prognostic value of chronic lymphocytic leukemia-international prognostic index (CLL-IPI) for Macedonian CLL patients was used. We incorporated the data of Rai staging system, most adverse cytogenetic marker and mutational status of immunoglobulin heavy chain.(table 1). On table 2 are presented patients characteristics according to IPI group.
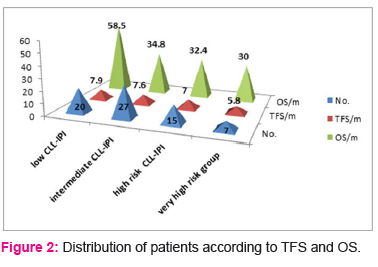
The median TFS for low CLL-IPI (n=20), intermediate CLL-IPI (n=27), high risk CLL-IPI (n=15) and very high risk group (n=7) according to the CLL-IPI scoring system was 7.9, 7.6, 7.0 and 5.8 months, respectively.
The median OS for low risk group was 58.5 for intermediate, high, and very high risk group was 37.8, 34.6 and 30 months, respectively (figure2).
Using Prognostic Nomogram we calculate estimated 5-year OS (figure3)(3). According to projected 5-year OS 98.7 % of patients with low-CLL-IPI group will have 5-years OS, 92% of patients from intermediate CLL-IPI group will have 5-years OS, only 40% of patients from high risk group will have 5-years OS, and 33% of patients from very high risk group will have 5-years OS.
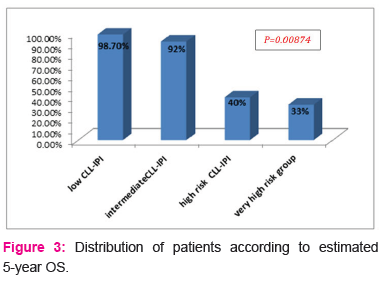
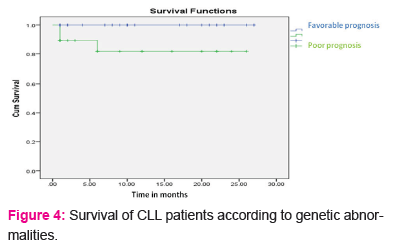
Multivariate analysis indicated that del 17p (P< 0.00874) was independent prognostic factors of TFS (figure4).
DISCUSION
CLL is a diverse disease with a median survival of about 10 years, but the prognosis varies widely among patients. In the past nearly 40 years the two clinical staging systems of Rai and Binet are used to evaluate the prognosis of patients. Though, these two systems are based on physical examination and laboratory analysis. Development of science with the expansion of disease alertness, new prognostic and predictor factors are discovered. IGHV gene mutation, combined with del (17p) and/or TP53 are the strongest prognostic and predictor factors. Next generation sequencing revealed some new mutation like NOTCH1 mutation, SF3B1 mutation, BIRC3 mutation, MYD88 mutation which are all associated with prognosis of CLL (4) .Parallel to diagnostic development, the treatment model enters the era of immunochemotherapy or even the new drug era from the age of alkylating agents, the survival prognosis of CLL patients also changes(5). Consequently, the two old clinical staging systems of Rai and Binet have been suppressed and clinician needs a new scoring system for risk stratification of CLL patients.
The CLL-IPI scoring system includes prognostic markers such as clinical features, cytogenetics, and molecular mutations, TP53 deletion and/or mutation, IGHV gene mutation status, B2Microglobulin, clinical stage, and age. CLL-IPI scoring system defines a weighted risk score for each prognostic factor, more exact risk stratification of CLL. For the low-risk, intermediate-risk, high-risk and high-risk groups, the 5-year survival rates were 93.2%, 79.3%, 63.3%, and 23.3%, respectively. Other authors like Pflug et al(6) and Rossi et al (7) proposed other prognostic scoring systems, with laboratory analysis thymidine kinase (TK1) and with the absence of clinical features such as age and staging. New CLL-IPI scoring system it is recommend the as a new prognostic score system by American NCCN and IW CLL. Consequently, this study aimed to verify whether the CLL-IPI scoring system in the Macedonian population has the same risk stratification and prognostic inferences.
This study included 75 treatment –naïve patients with CLL who were diagnosed in University clinic for hematology. The majority of patients included in the study had no treatment indication, with a high proportion of Binet A patients. According to presence of 17p deletion a few patients has the mutation distributed in very high CLL IPI risk group.
This data correlate with high awareness of CLL disease and patients are diagnosed at early stage of the disease. Therefore, the proportion of patients in the low-risk group stratified by the CLL-IPI scoring system was equal like the other Western countries.
The TFS time of the whole group was between 5.8-7.9months. The TFS time of the patients in the very high-risk group was similar to that in the West Europe, suggesting that the TFS time of these patients was extremely short. The clinical need to closely observe and timely judge the timing of starting treatment, CLL-IPI scoring system can also screen out patients who really need treatment.
Multivariate analysis showed that 17p deletion is independent adverse prognostic factors affecting patients with TFS.
The CLL-IPI scoring system has been gradually applied in clinical practice(8, 9). The controlling significance of the CLL-IPI scoring system for TFS is not affected by the treatment approach, but whether it can still have a good guiding significance for OS, and the patient data to be included in the new drug treatment is demonstrated.
Conclusion
CLL-IPI is the powerful tool for risk stratification in Macedonian CLL patients and this system also provided treatment recommendations for the different patient risk subgroup. Though, it is unknown how newly developed CLL therapies and newly identified molecular mutations would be incorporated into this revised staging system.
Acknowledgement: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1.An international prognostic index for patients with chronic lymphocytic leukaemia (CLL-IPI): a meta-analysis of individual patient data [J]. Lancet Oncol, 2016 , 17 ( 6 ): 779 - 790 . DOI:10.1016/S1470-2045 ( 16) 30029-8 .
2.Hallek M , Cheson BD , Catovsky D , et al .Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines[J]. Blood, 2008, 111(12):5446-5456.DOI: 10.1182/blood-2007-06-093906 .
3.Wierda WG, O'Brien S, Wang X, Faderl S, Ferrajoli A, Do KA, et al. Prognostic nomogram and index for overall survival in previously untreated patients with chronic lymphocytic leukemia. Blood. 2007; 109(11): 4679–85.
4. Qin SC , Xia Y , Miao Y , et al .MYD88 mutations predict unfavorable prognosis in chronic lymphocytic leukemia patients with mutated IGHV gene[J]. Blood Cancer J,2017,7(12):651.DOI:10.1038/s41408-017 -0014-y .
5.Hallek M .Chronic lymphocytic leukemia: 2017 Update ON Diagnosis, Risk Stratification, and treatment[J]. Am J Hematol, 2017,92(. 9):946-965.The DOI: 10.1002 / ajh.24826 .
6.Pflug N , Bahlo J , Shanafelt TD , et al .Development of a comprehensive prognostic index for patients with chronic lymphocytic leukemia[J]. Blood,2014,124(1):49-62. DOI: 10.1182/blood-2014-02 -556399 .
7.Rossi D , Rasi S , Spina V , et al .Integrated mutational and cytogenetic analysis identifies new prognostic subgroups in chronic lymphocytic leukemia[J]. Blood, 2013,121(8):1403-1412. DOI:10.1182/blood-2012- 09-458265 .
8.Molica S , Giannarelli D , Levato L , et al .Assessing time to first treatment in early chronic lymphocytic leukemia (CLL): a comparative performance analysis of five prognostic models with inclusion of CLL-international prognostic index (CLL-IPI)[J]. Leuk Lymphoma,2017,58(. 7):1736-1739. DOI: 10.1080 / 10428194.2016.1257791 .
9.Gentile M , Shanafelt TD , Mauro FR , et al .Comparison between the CLL-IPI and the Barcelona-Brno prognostic model: analysis of 1299 newly diagnosed cases[J]. Am J Hematol, 2018, 93(2):E35-35E37.DOI: 10.1002 / ajh.24960 .
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License