IJCRR - 11(3), February, 2019
Pages: 06-08
Date of Publication: 07-Feb-2019
Print Article
Download XML Download PDF
A Study on Effects of HbA1c Levels on Nerve Conduction Velocity in Type 2 Diabetes Mellitus Patients
Author: Abeer Masood, S. Aijaz A. Rizvi, Sheelu S. Siddiqi, Md Ziauddin
Category: Healthcare
Abstract:Aim: Diabetes mellitus is specifically a condition of hyperglycemia, insulin resistance, and relative impairment in insulin secretion.It is characterized by micro and macro vascular complications that lead to significant morbidity and mortality. Diabetic peripheral neuropathy is one of the most common long term complications of DM. HbA1c estimation is usually done which is indicative of glycaemic control. Nerve conduction studies (NCS) are electrodiagnostic tests used to evaluate the ability of the electrical conduction of the motor and the sensory nerves.
Therefore the effect of HbA1c on the nerve conduction velocity in Type 2 Diabetes Mellitus Patients was studied.
Methodology: Total number of 60 subjects (diabetic subjects and the healthy controls) were examined to assess the Diabetic neuropathy. Sensory Nerve conduction velocity (NCV) test was done along with the estimation of HbA1c levels in all the diabetic subjects (HbA1c≥6.5%) and the healthy controls.
Results: The analysis showed that the nerve conduction velocity decreased in diabetic patients with apoor glycaemic control in comparison to healthy and diabetic subjects with good glycaemic control.
Conclusion: In diabetic subjects there is progressive neuronal involvement which is accelerated by poor glycaemic control leading to development of diabetic neuropathy. Therefore, NCS can be employed for the early detection of neuropathy in diabetic patients.
Keywords: Diabetes mellitus, Nerve conduction studies, Glycated haemoglobin
Full Text:
INTRODUCTION
Diabetes mellitus is specifically a condition involving hyperglycaemia, insulin resistance, and relative impairment in insulin secretion [1]. It has become one of the fastest spreading endocrine disorders, characterized by metabolic abnormalities and with prolonged duration there is ongoing micro and macro vascular complications that can lead to significant morbidity and mortality [2]. In response to insulin resistance, hyperinsulinemia play an important role in the genesis of these abnormalities. The most commonly occurring microvascular complication is “Diabetic neuropathy” (DN) that accounts for around 28% of all the complications seen in diabetics [3]. It is a progressive condition with presence of chronic period of asymptomatic stage [4]. In the asymptomatic stages, it leads to the diabetic foot as the disease process progresses, which proves to be a highly morbid condition that arises from the infection and the ulceration of the foot, ultimately which may lead to amputation [5]. Therefore, identification of neuropathy in diabetics is considered to be important. For preventing DN and other diabetic complications; early identification and good glycaemic control are the essential factors. According to the recommendations of the American Academy of Neurology at least one of the five criteria for diagnosing DN should be present: Symptoms, Signs, electro-diagnostic tests, Quantitative sensory tests and Autonomic testing [6]. Practically, Nerve conduction studies (NCS) are electro-diagnostic tests which are used to evaluate the ability of the electrical conduction of the motor and the sensory nerves. Also, it is a known fact that poor glycaemic control is responsible for early onset of microvasular complications [7]. Glycated haemoglobin (HbA1c) has been established as a marker of glycaemic control and it also provides an indication of the risks that produces onset of microvascular complications [8]. 50% of patients present with symptoms like sensation of numbness, tingling, sharp burning pain. The patients may have a "glove and stocking" distribution of sensory symptoms involvement. Hence, we intended to correlate Nerve conduction studies (NCS) with HbA1c to establish their role in Diabetes.
MATERIALS AND METHODS
This study was undertaken in the Department of Physiology in collaboration with Rajiv Gandhi Centre for Diabetes and Endocrinology on patients of Type 2 Diabetes Mellitus (T2DM) attending Diabetes clinic at J. N. Medical College, Aligarh Muslim University, India after approval from institutional research and ethical committee.
A total number of 60 subjects were included in the study group. The patients of 29-69years of age with a history of diabetes for 5-10 years attending the diabetic OPD were selected. Glycated haemoglobin levels were estimated, depending on the values of HbA1c subjects were divided into 2 Study Groups:
Group 1: 30 Type II diabetes mellitus patients with poor glycemic control, of both sexes, of age group 29-69 years.
Group 2: 30 Non-diabetic healthy subjects, of both sexes, of age group 29-69 years as a control group.
Group 2 was not associated with polyneuropathy, family history of peripheral nerve disease and consumed alcohol or drugs with potential neurotoxic effects. Patients with Type I DM, Type II DM patients on insulin therapy were excluded.
A consent was obtained from each participant and procedure was explained. Windows based Computerized EMG/NCV equipment NeuroStim4 in NCV lab in the Department of Physiology was used for electrophysiological analysis using surface electrodes to record the NCV.
Statistical evaluation of the results was performed using the statistical package IBM SPSS22. The data was summarized to test the difference in the mean values between the groups 1 and 2 by using the Student’s (unpaired) t test; p values < 0.05 were taken as the level of significance. Pearson’s correlation was used to correlate between the different parameters.
RESULTS
DISCUSSION
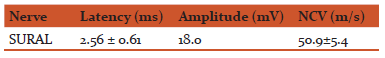
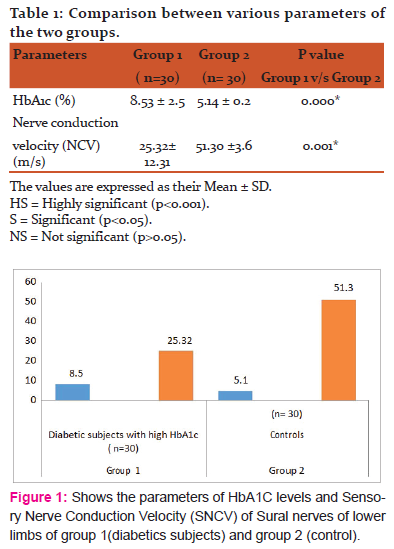
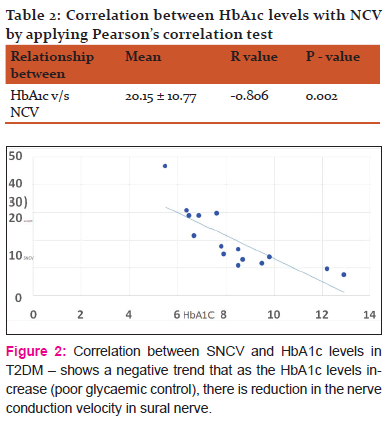
Diabetic neuropathy is a common complication of diabetes mellitus leading to severe morbidity that compromises the quality of life and affects daily routine activities. An intensive treatment of neuropathy at the sub clinical level decreases the risk of neuropathy [9]. One of the important methods for assessing nerve functions in DN is the Nerve conduction studies. In this study, it was observed that the nerve conduction velocity progressively decreased from the controls (51.30 ±3.6) to the diabetics with poor glycaemic control (25.32± 12.31). These findings are in accordance with those of previous researchers
-
Bansal et al, 2006 have suggested that the slowing of NCV indicates it is due to the continuous damage occurring to the myelin sheaths and they are also of the opinion that the amplitude decreases with the rising HbA1c levels, thus resulting in the onset and progression of axonopathy [11]. Therefore, the monitoring of diabetic patients with NCS may provide help in predicting the onset of DN. So we draw a conclusion, that the estimation of both NCV and the HbA1c levels in diabetics is helpful in identifying the risk category for DN, which is one of the main causes for severe morbidity among the diabetes. Also Clayton W, Elasy TA et al,2009 showed that the accumulation of sugar products results in a decrease in the synthesis of nerve cell myoinositol, which inhibits Na+/K+ ATPase activity, that is required for normal neuron conduction. Decrease in activity of Na+/K+ ATPase pump results in Na +/K+ retention, oedema, myelin swelling, axoglial dysfunction and nerve degeneration; further leading to cause neuropathy. [12]
CONCLUSION
The present study showed that both, nerve conduction studies and glycated hemoglobin, are useful modality for detecting diabetic neuropathy. Nerve conduction studies are one of the important methods for diagnosis and evaluation of diabetic sensorimotor polyneuropathy especially for the subclinical neuropathies. Routine nerve conduction studies can be done regularly in diabetic subjects at least on yearly basis. Our study recognises that periodic screening should be carried out in diabetics to prevent long term complications of diabetes.
ACKNOWLEDGEMENT: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/ editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
CONFLICTS OF INTEREST: There is no conflicts of interest.
The study was conducted in JN Medical College and Hospital, AMU Aligarh. The study was not funded by any organisation
References:
-
Harris MI. Impaired glucose tolerance in the U.S. population. Diabetes Care 1989 12:464.
-
-
Zargar AH, Wani AI, Masoodi SR, Laway BA, Bashir MI. Mortality in diabetes mellitus – data from a developing region of the world. Diabetes Res Clin Pract 1999; 43: 67-74.
-
Tesfaye S, Stevens LK, Stephenson JM, Fuller JH, Plater M, Ionescu -Tirgoviste C et al. Prevalence of diabetic peripheral neuropathy and its relation to glycemic control and potential risk factors. The Euro Diab IDDM complications study. Diabetologia 1996; 39: 1377-1384.
-
Perkins BA, Bril V. Diagnosis and management of diabetic neuropathy. Curr Diab Rep 2002; 2: 495–500.
-
Partanen J, Niskanen L, Lehtinen J, Mervaala E, Siitonen O, Uusitupa M. Natural history of peripheral neuropathy in patients with non-insulin dependent diabetes mellitus. N Engl J Med 1995; 333: 89 –94.
-
Consensus statement. Report and recommendations of the San Antonio conference on diabetic neuropathy. American Diabetic Association, American Academy of Neurology. Diabetes Care 1988;11: 592–7.
-
Mayurasakorn K, Somthip N, Caengow S, Chulkarat N, Wanichsuwan M. Glycemic control and microvascular complications among type 2 diabetes at primary care units. J Med Assoc Thai 2009; 92:1094-101.
-
Chandalia HB, Krishnaswamy PR. Glycated hemoglobin. Current Science 2002; 83: 1522-1532.
-
Dahl-Jorgensen K, Brinchmann-Hansen O, Hanssen KF, Ganes T, Kierulf P, Smeland E et al. Effect of near normoglycaemia for two years on progression of early diabetic retinopathy, nephropathy, and neuropathy: The Oslo Study. Br Med J 1986; 293: 1195-1199
-
The DCCT Research Group: Factors in the development of diabetic neuropathy in feasibility phase of Diabetes Control and Complications Trial (DCCT). Diabetes 1988; 37: 476-481.
-
Bansal V, Kalita J, Misra UK. Diabetic neuropathy. Postgrad Med J 2006; 82: 95-100.
[12]Clayton W, Elasy TA. A review of the pathophysiology, classica on and treatment of foot ulcers in diabetic patients. Clinical Diabetes.2009; 27(2): 52-58
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License