IJCRR - 10(23), December, 2018
Pages: 01-05
Date of Publication: 18-Dec-2018
Print Article
Download XML Download PDF
Risk Factors Determination for Complication in Adult Tubercular Meningitis Patients
Author: Arijit Sinha, Kapildev Mondal
Category: Healthcare
Abstract:Introduction: Tubercular meningitis (TBM) is an important health issue, particularly in developing countries. There are several factors which are responsible for complications. Determination and modification of such risk factors are important to manage the cases.
Aim of the study: Determination of risk factor for complication in adult tubercular meningitis.
Study design: It is a retrospective, observational, analytical study.
Methods: Adults(>18 years age) TBM cases were studied within 6 months follow up during august 2017 to December of 2017. Details history, clinical examination, investigation were done. Severity was assessed by MRC(Medical Research Council) staging and outcome was determined by Glasgow outcome scale(gos).
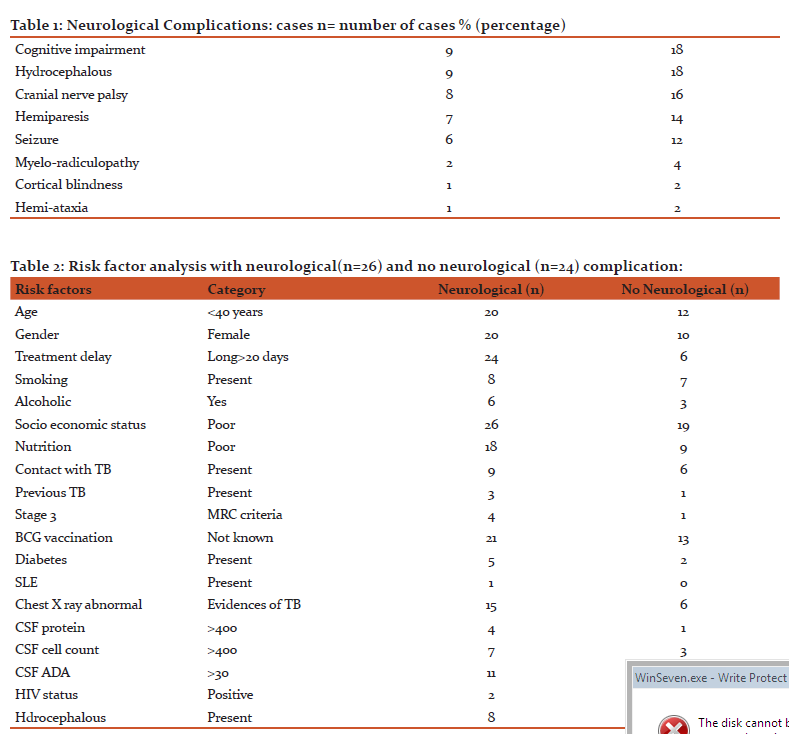
Results: Among 50 cases 90% were in low socioeconomic group and females(60%) were affected more. Major neurological complications were hydrocephalous(18%), cognitive impairement (18%), cranial nerve palsy(16%), hemi paresis(14%), seizure(12%). Important risk factors were low socioeconomic status, smoking, alcoholism, poor nutrition, diabetes, immunosuppression, high CSF protein, ADA.
Conclusion: TBM with important risk factors patient to be monitored more frequently for early detection of any complications and management.
Keywords: Tubercular meningitis, Complications, Risk factors
Full Text:
Introduction: TBM is a serious public health problem , particularly in immunocompromised persons. It is estimated that more than 1.5 million people died from tuberculosis in a year.[1] Tubercular meningeal involvement occur in about 1% patients with active tuberculosis.[2] Neurological and systemic complication are important cause of mortality and morbidity in TBM. 50% cases of TBM results with complication or death even with treatment with anti tubercular drugs.[3] Old age, alcoholism, immune disorders, malignancy, diabetes, intravenous drug user, splenectomy, immunosuppressive drugs, smoking, with pulmonary involvement, treatment delay, advanced stage of TBM on admission—may be the factors that causes more complication. Other investigational parameters like high protein & lactate in CSF, hydrocephalous are associated with increased risk [4] .Our aim of this study is to determine the risk factors and its relation with complications[5]. This study may be helpful for the clinician and to the community regarding management of TBM.
Methods
We performed the study at Murshidabad Medical College(MMC) during the period august 2017 to December of 2017 and included total 50 cases randomly. It is the catchment area of surrounding four districts of West Bengal and Jharkhand. Cases were either diagnosed at MMC or came for follow up after diagnosed out side. It is a retrospective, observational, analytical study. Inclusion criteria were: (1)diagnosed cases of TBM, (2)age more than 18 years at the time of diagnosis&(3) neurological complications associated with TBM within 6 months follow up. Exclusion criteria were:(1) Unwilling patients and(2) iatrogenic complications from this study. We noted details history, examined clinically and adviced proper investigations in each case. We collected all data for age, sex, socioeconomic status, educational back ground, nutritional status, personal habits(smoking, alcohol intake, IV drug use), occupation(type of job), glycemic status, renal function, liver function, autoimmune disorders(lupus etc.), HIV infection, malignant conditions, immunosuppressive drugs, major operation in the past (splenectomy etc.), treatment delay(interval between first symptoms and specific treatment), stage of disease at presentation(MRC- Medical Research Council, 1=no definite neurological symptoms plus minus meningism, 2=signs of meningeal irritation, clouding of consciousness, focal neurological signs—hemiparesis, cranial nerve palsy, 3= severe clouding of consciousness or delirium, convulsion, serious neurological signs such as hemiplegia, paraplegia, involuntary movements), CSF protein, cell count, CBNAAT, ADA[6] .We analysed data in respect to risk factors TBM uncomplicated, TBM complicated cases. Glasgow outcome scale were used to asses outcome(1=death, 2= persistent vegetative state,3= severe disability, dependent, 4=moderate disability, independent, 5= good, normal life.[7]
Results
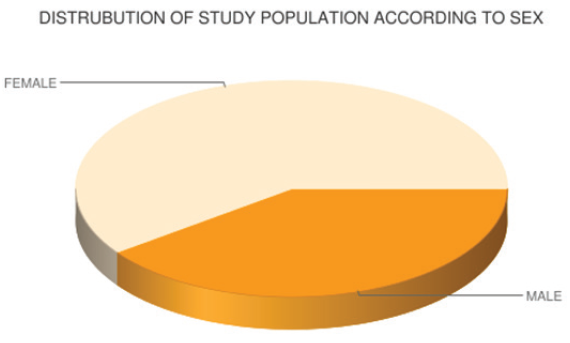
Among 50 patients in the study group 90% (n=45) were in low socioeconomic group with poor educational status, 60%(n=30) were female, 54%(n=27) were malnourished. History of contact with known tuberculosis patients was positive in 30%(n=15) cases. Vaccination with BCG was not known in 68%(n=34) cases, most of them were in older age group. Among 50 patients following data were found –smoker 30%(n=15), alcoholic 18%(n=9), heavy worker 10%(n=5), diabetic 18%(n=9), HIV+ 14%(n=7), systemic lupus 2%(n=1), vagotomy 2%(n=1), splenectomy 2%(n=1). Presentation according to MRC staging were—stage 1=50%(n=25), stage 2= 40%(n=20), stage 3= 10%(n=5). Treatment delay was found as early delay(<20 days) 40%(n=20) cases, late delay (>20 days) 60%(n=30) cases. 8%(n=4) patients were affected by pulmonary tuberculosis previously. Signs of meningial irritation was found in 90%(n=45) cases, hemiparesis 14%(n=7) cases, cranial nerve palsy in 16% (n=8) cases, seizure in 12%(n=6) cases, cognitive impairment in 18%(n=9) cases, hearing loss in 4%(n=2) cases, hemiataxia 2%(n=1) cases, cortical blindness in 25(n=1) cases, myelo radiculopathy/ paraparesis in 4%(n=2) cases.[Table 1] Evidences of tuberculosis were found in 42%(n=21) cases and miliary mottling in 18%(n=9) cases. CSF cell count(cell/micro L) was up to100 in 40%(n=20), 101 to 400 in 40%(n=20), more than 400 in20%(n=10) cases. CSF protein(mg/dl) raised upto 100 in 50%(n=25) cases, 101 to 400 in 40%(n=20) caese, more than 400 in 10%(n=5) cases. CSF glucose (mg/dl) was found <20 in 6%(n=3), 21 to 60 in 72%(n=36), >60 in 22%(n=11) cases. CSF ADA(IU/L) was 10 to 30 in 70%(n=35) cases and >30 in 30%(n=15) cases. Abnormal neuroimaging (CT/MRI Brain) in the form of meningeal enhancement in 78% (n=39) cases, hydrocephalous 18%(n=9) cases, infarct in 14%(n=7) cases, tuberculoma in 6%(n=3) cases. Among 7 infarct cases basal ganglia involved in 5 cases, with cortical involvement in 2 cases. Median age of stroke was 37 years. Outcome was determined by Glasgow outcome scale—GOS 1= not included in this study, GOS 2 =2%(n=1), GOS 3=16%(n=8), GOS 4=44%(n=22), GOS 5 =38%(n=19). Risk factor analysis with neurological complications with no neurological complications are shown in table 2.
Discussion
Tubercular meningitis is a medical emergency. Early diagnosis, proper treatment, handling of risk factors are most important to reach ultimate goal. Most of the patients in age group <40 years are susceptible to end in nervous system complications. Virmani et al obsevered 35.5% cases was in 21 to 30 years age group.[8] In our study females were more sufferer (60%) and prone to develop neurological complications. But Gambhir et al found more incidences in Males. [9] Seizure was found in12% cases which was consistent with study done by Virmani.[8] Past history of tuberculosis was found in 16% cases, whereas in Ahuja et al study, it was 10%.[10] In our study cranial nerve palsy was found in 16% cases but Khatua et al found it in 50% cases in 1961, Virman et al found in 15.4% cases.[11,8] Stroke in TBM are mostly ischemic, often with ischemic conversion ,involves deep penetrating arteries: the basal ganglion, internal capsule, thalamus. Cortical and sub cortical infarct are not uncommon.[12] In our study 18% cases were suffered from stroke but Anderson et al found it in 33% cases.[13] Ribera et al found higher CSF ADA (15.7U/L) in TBM cases.[14] CSF protein level also raised in TBM and has significant correlation with CSF ADA. [15] BCG vaccination has protection against TBM, disseminated TB, military TB.[16] In our study 68% cases had no definite history of BCG vaccination. Several studies showed role BCG vaccinate in reducing mortality from TBM. [17] Late delay in treatment was found in 60% cases. In a Taiwan study 47.6% patients experienced delay in initiating treatment.[4] MRC stage 3 was in 10% cases in our adult study but it was 62% in another paediatric study. [18] GCS, raised ICT, hydrocephalous are important predictors of mortality. [19] HIV infected patients are at increased risk to develop TBM .[20] In our study 4% cases were HIV positive. Clinical presentation, outcome do not seem to be altered in HIV positive cases. [21] We found hydrocephalous in 18% cases, in other study it was 12%.[22] Hydrocephalous was found in 18% cases in another study and predicted as poor outcome.[23] Old age, advanced stage on admission, hydrocephalous, positive TB culture in CSF are the factors associated with poor prognosis of TBM. [24] In our study we found age<40 years, female sex, long delay in treatment, alcoholism, poor socioeconomic and nutritional status, previous tubercular infection, MRS stage 3, diabetes, CSF cell count and protein >400 , ADA >30, hydrocephalous, abnormal chest x ray as important risk factors for neurogenic complication in TBM.
Conclusion:
Complications of tubercular meningitis patient having several risk factor is more than patient having no risk facor.
Acknowledgement: We are grateful & indebted to respected Principal, MSVP, Deputy superintendent, authors, editors and publishers of all those articles, journals from where the literature for the article has been reviewed, & others of Murshidabad medical college & hospital.
Ethical clearance & inform consent has taken.
Source of fund:Self.
Conflict of interest:Nil.
Abbreviation:
TBM-Tuberculer meningitis.
Ict-intracranial pressure.
CSF-cerebro spinal fluid.
SLE-systemic lupus erythematous.
MMC-Murshidabad medical college.
GCS-Glasgo coma scale.
GOS-Glasgo outcome scale
References:
1.WHO Global tuberculosis report,htt:/www.who.int./tb/publications/global_report/enAccessed,3rd Oct 2015
2.Thwaites G, Fisher M, Hemingway C, Scott G Salomon T, Innes J, British Infectious Society guidelines for the diagnosis and treatment of tuberculosis of the central nervous system in adults and children. JInf. Secur, 2009,59(3),167—187
3. Thwaites GE, Hein TT, Tubercular Meningitis: many questions too few answers, Lancet Neurol, 2005,4,160—170
4. Sheu JJ, Yuan CC, Yang CC, Predictor of outcome and treatment delay in patients with TBM. Am J Med Sci, 20009,338(2),134—139
5. Lu CH, Chang WN, Chang HW, The prognostic factor of adult tubercular meningitis, Infection, 2001,29(6),299—304
6. Streptomycin in Tuberculosis Trial Committee, Medical Research Council, Streptomycin treatment in tuberculous meningitis, Lancet 1948, 215, 582—96
7. Jennet B, Bond M, Assessment of outcome after severe brain damage. A practical scale, Lancet 1975, 305 ,480—84
8. Venkataraman S, Sarsavani V Rao, Ahuja GK, Virmani V, Clinical spectrum of neurotuberculosis in adults, JAPI, 1980,28(11), 413—37
9. Gambhir IS, Mehta M, Singh DS, Khanna HD, Evaluation CSF adenosine deaminase activity in tubercular meningitis, JAPI 1999, 47, 192-94
10. Ahuja GK, Mohan KK, Prasad K, Behari M, Diagnostic criteria for tubercular meningitis and their validation, Tuber Lung Disease, 1994,75(2), 149—52
11. Khatua SP, Tuberculous meningitis in children, Analysis of 231 cases, JIMA, 1961, 37,332
12. Kolita J, Misra UK, Nair PP, Predictors of stroke and it’s significance in the outcome of tuberculous meningitis, J Stroke Cerebrovas Dis, 2009, 18, 251—58
13. Anderson NE, Somaratane J, Manson DF, Holland D, Thomas MG, neurological and systemic complications of tubercular meningitis and it’s treatment at Auckland City Hospital, Newzeland, J Clinic Neuro Sc, 2010,17,1114—18
14. Ribera E, Martnez VJM, Cana L, Senguru RM, Pascual C, Activity of adenosine deaminase in cerebrospinal fluid for the diagnosis and follow up of tuberculous meningitis in adults, J Infec Dis1987, 155,6015.
15. Prasad R, Kumar A, Khanna BK et al , Adenosine deaminase activity in cerebrospinal fluid for the diagnosis of tubercular meningitis, Ind J Tub, 1991,38,99—102
16. Kelekci S, Krabel M, Krabel D, Hamidi C, Hosoglu S, Gurkan MF, et al ,Bacillus Calmette Guerin is a preventive factor in mortality of childhood tuberculous meningitis, Int J Infec Dis, 2014, 25, 1—4
17. Kumar R, Dwivedi A, Kumar P,Kohli N, Tuberculous meningitis in BCG vaccinated and unvaccinated children, J Neurol Neurosurg Psychia, 2005, 76, 1550—54
18. Van Well GT, Paes BF, Terwee GB, Springer P, R oord JJ, Donald PR et al, Twenty years of pediatric tuberculous meningitis: A retrospective cohort study in the Western Cape of South Africa, Pediatrics, 2009, 123 e1—8, PubMed
19. Karande S, Gupta V, Kulkarni M, Joshi A, Prognostic clinical variable in childhood tuberculous meningitis: An experience from Mumbai, India Neurol India, 2005, 53, 191—95, PubMed
20. Jenkins PA, The Microbiology Of Tuberculosis, In PDO Davies ed Clinical Tuberculosis, London, Chapman and Hall Medical, 1994
21. Yechoor VK, Shandera WX, Rodriguez P et al, Tubercular meningitis among adults with and without HIV infection, Arch Int Med, 1996, 156, 1710—16
22. Bhargaba S, Gupta AK, Tandon PN, Tuberculous meningitis,: A case study , Br J Radiol, 1982,55,189—96
23. Tan EK, Chee MWL, Chan LL et al , Culture positive tubercular meningitis,: Clinical indicators of poor prognosis, Clin Neurol Neuro Surg,1999,101, 157—60
24. Hsu PC,Yang CC, Ye JJ, Huang PY, Chiang PC, Lee MH, Prognostic factors of tuberculous meningitis in Adults,: A 6 years retrospective study at tertiary hospital in North Taiwan, J Microbiol Immunol Infec, 2010, 43(2), 111—1
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License