IJCRR - 8(10), May, 2016
Pages: 20-22
Date of Publication: 22-May-2016
Print Article
Download XML Download PDF
MECONIUM PERITONITIS - REPORT OF A RARE CASE
Author: Jeevitha K. J., Senthiru Ramachandran, Saravanan, Mahesh Bose
Category: Healthcare
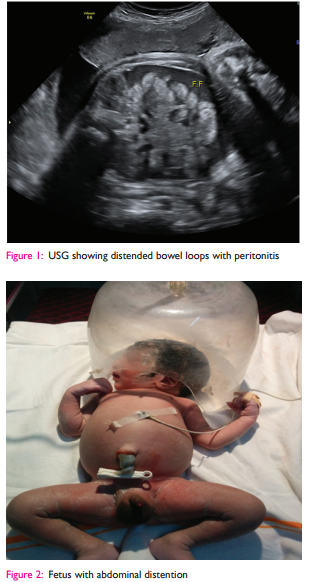
Abstract:Aim: To report on a rare case of meconium peritonitis (MP). Case Report: We report a case of G2P1L1 at 37 weeks of gestation, a post caesarean pregnancy with all prior normal ultrasound reports, came with complaints of decreased fetal movements. On ultrasound scan there was features suggestive of meconium peritonitis with small bowel perforation. She was delivered by emergency repeat caesarean section and the neonate underwent laparotomy on the first neonatal day.
Discussion: Meconium peritonitis is a rare condition diagnosed in antenatal period which has a high neonatal morbidity and mortality. Meconium peritonitis is an aseptic chemical peritonitis caused due to in-utero bowel perforation, most frequently secondary to obstruction, often diagnosed by routine fetal ultrasound. Conclusion: Early diagnosis and treatment are the keys to successful management of MP.
Keywords: Meconium, Chemical peritonitis, Bowel perforation
Full Text:
INTRODUCTION
Bowel obstruction (like atresia, intussception, bands and meconium plug) may result in bowel perforation and cause meconium peritonitis (MP). It is a sterile chemical peritonitis caused in utero. Meconium leaks into abdominal cavity and causes secondary infl ammatory reaction which results in 4 types of MP- Fibro adhesive, cystic, generalized or healed1 . It is a rare condition with estimated incidence of 1:30,000 cases2 . This can be diagnosed with routine prenatal ultrasound and have classic features of intra-abdominal calcifi - cation, ascites, intra-abdominal mass, bowel dilatation and polyhydramnios. It is diffi cult to prognosticate the outcome on the basis of the above fi ndings. Most of the neonates require emergency laparotomy and some may need second laparotomy and rarely third laparotomy for anastomosis of the intestine3 . The prenatally diagnosed MP causes overall morbidity of 22% and mortality of 11% and has better prognosis than postnatally diagnosed MP4, 5.
CASE REPORT
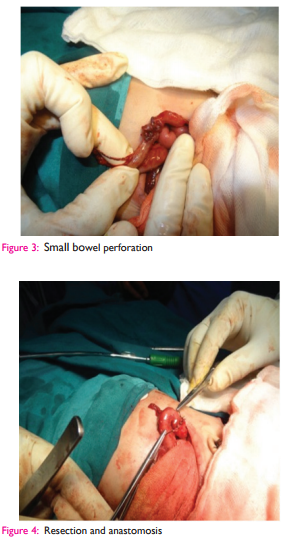
A 24 years old G2 P1 L1 post-caesarean pregnancypresented to our hospital, with an antenatal ultrasound at 37 weeks which was suggestive of small bowel perforation with meconium peritonitis (fi g1). Although her previous ultrasound scans were normal, the presenting condition warranted an emergency repeat lower segment cesarean section in view of fetal distress. She delivered a 3 kg boy baby with gross abdominal distention (fi g2) and mild respiratory distress. Following NICU admission, the baby was started on intravenous fl uids and an ultrasound was done to confi rm the diagnosis. Baby was posted for emergency laparotomy (Fig 3, 4, 5) under general anesthesia. Following layered dissection, bowel distention with perforation in the distal ileum was noted and the caecum was fi lled with meconium. Meconium was drained and ileostomy was done. In view of poor general condition of the neonate due to severe peritonitis, colon was not explored and drain was placed. On day 2 there was meco-nium drained in the drainage tube and neonate was posted for second laparotomy and found to have perforation in transverse colon with meconium in entire segment. Excision of 2 cm bowel and end to end anastomosis was done. Multiple bowel biopsies were taken to look for ganglion cells and their presence in the histopathology report ruled out aganglinosis. Neonate was placed on ventilator support and inotropes. Later baby was supported with total parenteral nutrition and gradually feeding established with concomitant ileostomy care. Neonate was discharged on day 12 and was advised for review and follow up after 3 months.

DISCUSSION
Meconium peritonitis should be considered when hyper-echogenic areas are found in the fetal abdomen during II and III trimester scan6 . Some of the common causes of obstruction which cause meconium peritonitis are atresia, volvulus, intussception, congenital bands, and meckel’s diverticulum- all of which accounts for 50% incidence. Other causes of MP include viral infections caused by cytomegalovirus and parvo virus B19, meconium ileus(25%) and cystic fi brosis (7-40%)7 . Bowel obstruction leads to perforation and causes meconium peritonitis which can be diagnosed by routine prenatal screening ultrasound. Some of the ultrasound features are ascites, polyhydramnios, dilated bowel loops, and intra-abdominal calcifi cation. Some of the complications following MP are prematurity (20% to 30%) and polyhydramnios(10%- 20%)8 . The prognosis depends on the etiology for bowel rupture. If MP is diagnosed before 24 weeks of gestation cystic fi - brosis should be ruled out by cordocentesis, chorionic villi sampling or amniocentesis. The defi nitive diagnosis is sweat chloride test in post natal period. Termination of pregnancy is the fi rst step in the management of MP followed by postnatal fetal x-ray and ultrasound to confi rm the diagnosis. The fetus can also be delivered vaginally but due to the presence of massive ascites and abdominal distention, dystocia have been reported. However in progressive disease, delivery by caesarean section is the preferred option9 . The neonate can be managed conservatively if there is no feature of bowel obstruction or peritonitis and the prognosis is good. In presence of bowel obstruction, surgery is the treatment of choice – drainage of the cyst/ascites, identifying the site of lesion and resection anastomosis with ileostomy care, which can be closed in later months. In the reported case the neonate was managed by resection anastomosis with ileostomy care.
CONCLUSION
Meconium peritonitis is a rare condition; however it can be effectively diagnosed on routine prenatal ultrasound. Management requires a multidisciplinary approach with astute NICU care and meticulous follow up. Early identifi cation and timely intervention signifi cantly reduces the concomitant morbidity and mortality associated with the disease. Consent of the patient: Obtained Source of funding: Nil Confl ict of interest: None
ACKNOWLEDGEMENT
The authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also greatful to authors/ editors/ publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. The author wish to acknowledge the help and contribution of Dr. Vijai Anand DNB, Mch.(Paediatric Surgery), Consultant peadiatric surgeon, Rio hospital, Annanagar, Madurai.
References:
1. Mcnamara A, Levine D. Intraabdominal fetal echogenic masses: a practical guide to diagnosis and management: Radiographics, 2005;25(3):633-45.
2. Nadia S, Annegret G, Ulrich G, Axel H, Andreas H, Peter B et al. Prenatal diagnosis and postnatal management of meconium peritonitis. J Perinat Med, 2009;37:535-38.
3. Amagada JO, Premkumar G, Arnold JM. Prenatal meconium peritonitis managed expectantly. J Obstet Gynaecol, 2004;24:311-12.
4. Saeed AI, Mahmood A. Meconium peritonitis in neonates: Management dilemma. Bahrain medical bulletin, 2008;30:1-6.
5. Hyun N, Chul SK, Yeon DK. Experience with meconium peritonitis. J Pediatr Surg,007;42:1822-25.
6. Maha S, Rukhsana I, Osama O. a case of in utero meconium peritonitis in a fetus delivered to a woman diagnosed with primary extrahepatic biliary atresia. JMC,2011;2:15-17
7. Ahmadu BU. Meconium peritonitis associated with meconium pseudocyst and intraperitoneal calcifi cation- a case report. IJBPAS, 2013; 2(5):1214-19.
8. Saxena P, Dabral A, Arora R, Minocha B. Meconium peritonitis- two case reports. J Obstet Gynecol India,2009;59: 475-76
9. Konje JC, Chazal R, MacFadyen, Taylor DJ. Antenatal diagnosis and management of meconium peritonitis: a case report and review of literature. Ultrasound Obstet Gynecol,1995;6:66-69.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License