IJCRR - 10(17), September, 2018
Pages: 06-10
Date of Publication: 10-Sep-2018
Print Article
Download XML Download PDF
Correlation between the Type of Arterial Vascularizacion and Presence and Localization of Myocardial Bridges
Author: Lujinovi? Almira, ?osovi? Esad, Kapur Eldan, Maida Šahinovi?, Kulenovi? Amela, Ajanovi? Zurifa
Category: Life Sciences
Abstract:Introduction: Myocardial bridges represent an anomaly of the coronary arteries' flow, which can be asymptomatic, or can lead to the coronary insufficiency and its clinical consequences. The aim of this research was to derermine whether there is a correlation between the type of arterial vascularization and presence and localization of the myocardial bridges. Material and Methods: As a material for this work, we used 45 human heart specimens from the Institute of Anatomy of the Medical Faculty in Sarajevo. At each heart, the type of arterial vascularization was determined, and in those specimens with myocardial bridges, the branch on which they were localized was recorded. Results: Out of total 45 human hearts, myocardial bridges were present at 24 (53.3%). One myocardial bridge was present in 16 hearts, two in 7 hearts and three in one heart. In the heart group with myocardial bridges, the incidence of right type of vascularization was 79.2%, and in the group without myocardial bridges 76.2%. The left type of vascularisation was least represented in both groups, with 9.5% in the heart group without bridges and 8.3% in the group with myocardial bridges present. Out of 33 detected myocardial bridges, 25 of them were on the left and 8 on the right coronary artery, so myocardial bridges are much more often localized on the branches of the left than the right coronary arteries, regardless of the type of arterial vascularization. Conclusion: There is no correlation of the type of arterial vascularization of the human hearts with the presence and localization of myocardial bridges.
Keywords: Coronary arteries, Type of arterial vascularizacion, Myocardial bridges
Full Text:
INTRODUCTION
Myocardial bridges represent an anomalies in the flow of coronary arteries in which coronary arteries and their branches that run subepicardially plunge shallow or deeper into the myocardium and after a short or long intramiocardial flow, return to the subepicardicial space (1).
The anomaly of bridging coronary arteries of human hearts was first mentioned by Reyman, distant in 1737 (2), and then Black in 1805 (3).
In the 20th century, many morphologists studied this anomaly, which was labeled with different names before the term myocardial bridge became established in medical terminology. Thus, Tandler used the name of the tunneled artery (4), alleging that the artery, in one part of its course, leaves the suepicardial space and plunges into the myocardium. Afterwards, Geiringer referred to it as the mural artery (5), then Polacek and Kralove first used the term myocardial bridge, which would become the most commonly used term for this anomaly (6).
For a long time, myocardial bridges have been considered as benign anomalies of coronary artery flows, without any clinical significance (7, 8).
However, at the end of the last century, using quantitative coronary angiography and intravascular ultrasound, it was established that the systolic reduction of the lumen of the "tunneled" segment of the dissected artery was caused by myocardial bridge contraction, maintained in the first half of the diastole, which is the dominant phase in myocardial perfusion, it became clear myocardial bridges can lead to coronary insufficiency and its clinical consequences (9,10). Since then, myocardial bridges have attracted not only morphologists but also clinicians. A vast number of clinical manifestations (angina pectoris, myocardial infarction, sudden cardiac death, cardiac rhythm disorders) have been described as a consequence of myocardial bridges' effect on coronary haemodynamics (11-15), mechanisms leading to the same (16-19), as well as significant influence of the morphological characteristics of myocardial bridges on the occurrence of coronary insufficiency (20-22). However, there is still a small number of data that speak of the presence and localization of myocardial bridges with the type of arterial vascularization of the heart, which led to this research.
MATERIALS AND METHODS
As a material for this research, we used 45 human hearts specimens from the Insitute of Anatomy of the Medical faculty of University of Saeajevo. The hearts were perserved 3-5 days in 10% formalin solution, followed by careful disecction and prepared arterial blood vessels of the heart. Type of arterial vascularization was determined in each specimen, and in those specimens where myocardial bridges were detected, the branch on which they were localized was recorded.
The obtained results were processed via SPSS 21 statistic program and a chi-square test was used to establish whether there is a correlation between the type of arterial vascularization of the heart with the presence and localization of myocardial bridges.
RESULTS
Out of a total 45 analyzed human heart specimens, the right type of the arterial vascularization was established in 35 (77.8%) specimens. The symmetrical (codominant) type of arterial vascularization was established in 6 specimens (13.3%) and the left type in only 4 (8.9%).
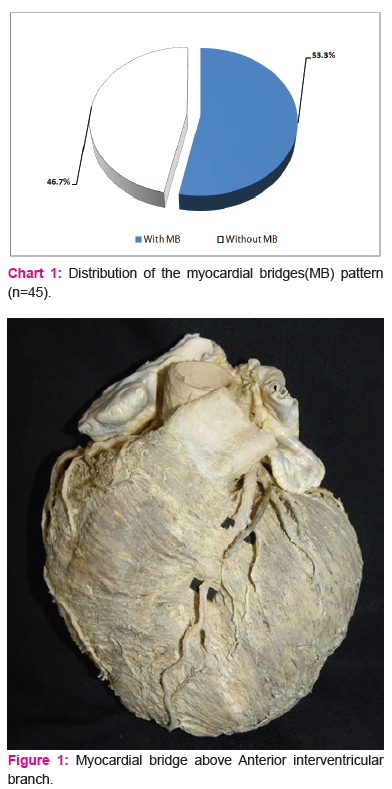
More than a half of heart specimens, 24 (53.3%) of them, had myocardial bridges present at the branches of the coronary arteries (Chart 1).
Chart 1. Distribution of the myocardial bridges(MB) pattern (n=45)
Total number of myocardial bridges was 33, from which 16 hearts had one myocardial bridge (Fig.1), 7 hearts had two and in one heart 3 myocardial bridges were found.
In the group of hearts with myocardial bridges, as well as in the group of hearts without them, dominant type of arterial vascularization was the right type (Chart 2).
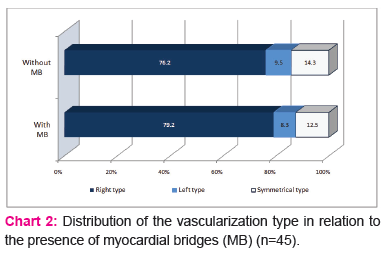
As seen from chart 2, the left type of the arterial vascularization was the least present in the both of the heart groups (8.3% in the group with the myocardial bridges and 9.5 % in the group without them). The symmetrical type of the vascularization was present in the 12.5% of the hearts with the myocardial bridges, and in the 14.3% of the hearts without myocardial bridges.
By testing the hypothesis of (non) existence of association of the type of vascularization and the presence of myocardial bridges, we conclude that in our sample there is no association between the type of vascularization and status in relation to the presence of myocardial bridges (χ2=0.057, p=0.972).
Table 1 shows the distribution of a part of the heart specimens in which myocardial bridges existed(24 hearts), accordingly to their location: left coronary artery (LCA), right coronary artery (RCA), and both left and right coronary arteries (LCA and RCA), in regard to the type of vascularization.
As shown in table 1, in 24 hearts with myocardial bridges, in 17 of them bridges were found on the left coronary artery, in 2 on the right coronary artery, and 5 hearts had myocardial bridges on both the left and right coronary arteries.
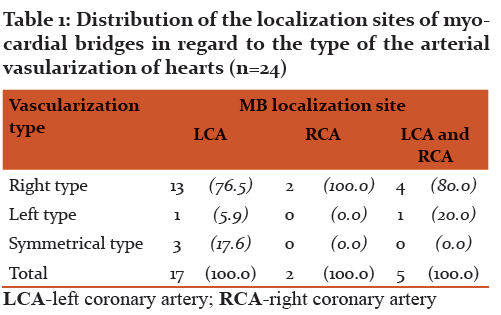
Regardless of the localization of myocardial bridges ( left coronary artery-LCA, right coronary artery-RCA, or both), the right type of vascularization is dominant (the same is represented by 77.3% in the hearts with myocardial bridges on the left, with 80.0% in the hearts with bridges on both the left and right, and the only type of vascularization identified in the hearts with myocardial bridges only on the right coronary artery).
Hearts with symmetrical type of vascularization did not have myocardial bridges on the right coronary artery, whereas this type of vascularization was present in 17.6% of the hearts with myocardial bridges localized only on the left coronary artery.
Left type of vascularization, as the least represented, was present in 5.9% of hearts with myocardial bridges only on the left, or in 20.0% of hearts with myocardial bridges present on both left and right coronary arteries.
By testing the hypothesis of the independence of the type of vascularization and localization of myocardial bridges, we obtain evidence for accepting the zero hypothesis, therefore we conclude that there is no association between the type of vascularization (right, left, or symmetrical) and localization sites of myocardial bridges (left coronary artery-LCA, right coronary artery-RCA, or both) (χ2=2.467, p=0.651).
Independently of the type of vascularization, most of the myocardial bridges, 25 of 33 (75.6%), were localized to the left, and only 8 bridges (24.24%) on the right coronary artery.
DISCUSSION
Data regarding frequency of myocardial bridges varies greatly depending on the method used for their detection. Using coronary angiography, they are detected in as little as 0.4-12% (23-26). Using dissection method, myocardial bridges are detected in a significantly larger number, so that the frequency of 53.3% determined in this paper coincides with the results of other authors using the same method and reported a frequency of 34.5% (27), 54% (28), 56% (29) and 58% (30).
Of the total of 45 hearts used as a material for this work, 37 (77.8%) had the right type of arterial vascularization, which confirmed the results of numerous authors that this type is dominant in human heart vascularization (31-33). The variation in the frequency of this dominant type of arterial vascularization of the heart may be related to the ethnic diversity of the inestigated populations, ranging from 60.5% to the Pakistani (34), to 86.6% in Turkish (35), up to 89% in the Indian population (36). The recorded frequency of the left type of vascularization of 8.9% and symmetric of 13.3% is also similar to the results obtained by the mentioned authors.
The relation between the type of coronary circulation and the presence of myocardial bridges is rarely investigated and there is little data in the literature (37-39). The results of this study have indicated that the incidence of arterial vascularization types is approximately same in the heart group with myocardial bridges as well as in the group without them, so it is established that there is no correlation between the presence of myocardial bridges and the type of arterial vascularization of the heart. Up to the same conclusion came Luis Erresto and his associates who investigated the Colombian population (37), as well as Ashraf and Nasr (38) among the Saudi population. However, these results are opposite to the results of Loukas and associates (39) who state that among the hearts with present myocardial bridges, the left type of vascularization is most common, in 66.6% of cases, while the right type is represented by only 24.6%. They further point out that the localization of myocardial bridges is closely related to the type of vascularization and state that out of 17 hearts with myocardial bridges and the right type of vascularization, 11 of them had myocardial bridges on the right coronary artery, and 46 hearts with myocardial bridges and left type vascularization, even at 42 hearts, the bridges were localized to the left coronary artery and its branches. Contrary to the results of Loukas and associates, the results obtained in this paper undoubtedly show that there is no correlation between the type of vascularization of the human hearts and the myocardial bridges localization, and that, regardless of the type of vascularization, myocardial bridges are most often localized to the branches of the left coronary artery. Namely, from 19 hearts with bridges and right type of vascularization, as many as 17 had myocardial bridges on the left coronary artery, where bridges were also located in both hearts with left and all 3 hearts with symmetrical type of coronary vascularization. The lack of correlation between the type of vascularization and localization of myocardial bridges was confirmed in the studies of Bharambe and Arole (40). Ashraf and Nasr (38) came to the same conclusions and point out that 77.8% of myocardial bridges were on the left coronary artery, without a significant difference in regard to the type of vascularization, which is in accordance with the results of this study, where of a total 33 myocardial bridges, 25 (75.76%) were localized to the left coronary artery.
Our opinion is that the study of the relation between myocardial bridges and the type of arterial vascularization should be continued because, as we have stated, the number of data is limited and controversial, and the possible association may have an effect on the origin, intensity and clinical consequences of myocardial ischemia.
CONCLUSION
There is no correlation of the type of arterial vascularization of the human heart with the presence of myocardial bridges. Myocardial bridges are much more often localized on the branches of the left than the right coronary arteries, regardless of the type of arterial vascularization.
ACKNOWLEDGEMENT
The authors acknowledge the immense help received from the scholars whose articles are cited and included in refer ences of this manuscript.
Conflict of interest: TheAuthors declare that they have any conflict of interest
Source of Funding: This research was financially supported by the Federal Ministry of Science and Education of Bosnia and Herzegovina, rescript number: 05-39-3910-1/15.
References:
- Shinjo SK, Oba-Shinjo SM, Prates Nevb. Bovine myocardial bridge morphology and association with coronary atherosklerosis. Braz J Morphol Sci. 2004;21(2):95-98.
- Alegria JR, Herrmann J, Holmes DR, Lerman A, Rihal CS. Myocardial bridging. European Heart Journal. 2005; 26(12):1159-1168.
- Black S. A case of angina pectoris with a diddection. Memoirs Med Soc London.1805;6: 41-48.
- Tandler J. Gefasse des Herzens. Anatomie des Herzens. 1913;41:219-229.
- Geirenger E. The mural coronary. Am Heart J. 1951; 41(3):359–368.
- Pola?ek P, Kralove H. Relation of myocardial bridges and loops on the coronary arteries to coronary occlusions. Am Heart J. 1961;61:44-52.
- Kramer JR, Kitazume H, Proudfit WL et al. Clinical significance of isolated coronary bridges: benign and frequent condition involving the left anterior descending artery. Am Heart J. 1982;103:283-288.
- Julliere Y, Berder V, Suty-Selton C et al. Isolated myocardial bridges with angiographic milking of the left anterior descending coronary artery: a long-term follow-up study. Am Heart J. 1995; 129:663-665.
- Schwarz ER, Klues HG, vom Dahl J et al. Functional, angiographic and intracoronary Doppler flow characteristics in symptomatic patients with myocardial bridging: effect of short-term intravenous beta-blocker medication. J Am Coll Cardiol. 1996; 27: 1637–1645.
- Ge J, Jeremias A, Rupp A et al. New signs characteristic of myocardial bridging demonstrated by intracoronary ultrasound and Doppler. Eur Heart J. 1999; 20: 1707–1716.
- Farugui AM, Maloy WC, Felner JM et al. Symptomatic myocardial bridging of the coronary artery.Am J Cardiol. 1978; 41: 1305-1310.
- Tsujita K, Maehara A, Mintz GS, et al. Impact of myocardial bridge on clinical outcume after coronary stent placement. Am J Cardiol. 2009; 103:1344-1348.
- Feldman AM, Baughman KL. Myocardial infraction associated with a myocardial bridge, Am Heart J. 1996; 111: 784-788.
- Dulk K, Brugada P, Braat S et al. Myocardial bridging as a cause of paroxysmal atrioventricular block. J Am Coll Cardiol. 1983; 1:965-969.
- Bestetti RB, Costa RS, Oliveira JM. Can isolated myocardial bridging of the left anterior descending coronary artery be associated with sudden death during exercise? Acta Cardiologica. 1991; XLVI: 27-30.
- Klues HG, Schwarz ER, vom Dahl J et al. Disturbed intracoronary hemodynamics in myocardial bridging: Early normalization by intracoronary stent placement. Circulation. 1997; 96(9):2905-2913.
- Ishii T, Asuwa N, Masuda S, Ishikawa Y, Kiguchi H, Shimada K. Atherosclerosis suppression in the left anterior descending coronary artery by the presence of a myocardial bridge: an ultrastructural study. Mod Pathol. 1991; 4: 424–431.
- La Grutta, Runza G, Lo Re G et al. Prevalence of myocardial bridging and correlation with coronary atherosclerosis studied with 64-slice CT coronary angiography. Radiol Med. 2009; 114(7): 1024-1036.
- Ge J, Erbel R, Görge G, Haude M, Meyer J. High wall shear stress proximal to myocardial bridging and atherosclerosis: intracoronary ultrasound and pressure measurements. Br Heart J. 1995; 73:462-465.
- Ishikawa Y, Akasaka Y, Fujiwara M et al. Anatomic properies of myocardial bridge predisposing to myocardial infraction. Circulation. 2009; 120(5): 376-383.
- Ishikawa Y, Kawawa Y, Kohda E, Shimada K, Ishii T. Significance of the anatomical properties of a myocardial bridge in coronary heart disease. Circ J. 2011;75(7):1559-66.
- Lujinovi? A, Kulenovi? A, Kapur E, Gojak R. Morphological aspects of myocardial bridges.Bosn J Basic Med Sci. 2013 Nov;13(4):212-217.
- Mavi A, Sercelik A, Ayalp R, Karben Z, Batyraliev T, Gumusburun E. The angiographic aspects of myocardial bridges in Turkish patients who have undergone coronary angiography. Ann Acad Med Singapore. 2008 Jan;37(1):49-53.
- Juilliére Y, Berder V, Suty-Selton C, Buffet P, Danchin N, Cherrier F. Am Heart J. Isolated myocardial bridges with angiographic milking of the left anterior descending coronary artery: a long-term follow-up study. 1995;129(4):663-5.
- Ishimori T. Myocardial bridges: a new horizon in the evaluation of ischemic heart disease.Cathet Cardiovasc Diagn. 1980;6(4):355-7.
- Lujinovi? A, Ovcina F, Arslanagi? A, Voljevica A, Spuzi? M. Presence of the muscular bridges and their influence on coronary insufficiency. Med Arh. 2005;59(3):152-155.
- Hostiuc S, Negoi I, Rusu MC, Hostiuc M. Myocardial Bridging: A Meta-Analysis of Prevalence.J Forensic Sci. 2017: 10.1111/1556-4029.13665.
- Lee SS, Wu TL.The role of the mural coronary artery in prevention of coronary atherosclerosis.Arch Pathol. 1972;93(1):32-5.
- Ferreira AG Jr, Trotter SE, König B Jr, Décourt LV, Fox K, Olsen EG. Myocardial bridges: morphological and functional aspects Br Heart J. 1991;66(5):364-367.
- Lima VJ, Cavalcanti JS, Tashiro T. Myocardial bridges and their relationship to the anterior interventricular branch of the left coronary artery.Arq Bras Cardiol. 2002 Sep;79(3):215-22
- Vinitha G, Sarala HS, Priya R. A cadaveric study on coronary preponderance. Int J Anat Res 2015,3(3):1289-1292.
- Gupta T, Saini A, Sahni D. Terminal branching pattern of the right coronary artery in left-dominant hearts: a cadaveric study.Cardiovasc Pathol. 2013;22(3):179-82
- Ortale JR, Keiralla LC, Sacilotto L. The posterior ventricular branches of the coronary arteries in the human heart. Arq Bras Cardiol. 2004;82(5):468-72, 463-467.
- Fazlul AM, Malik SN, Khan IS, Kachlu AR, Rehman M, Hussain J, Ahmed I. Coronary Artery Dominance: What pattern exists in Pakistani Population? Ann. Pak. Inst. Med. Sci. 2011; 7(1): 3-5.
- Erol C, Seker M. The prevalence of coronary artery variations on coronary computed tomography angiography.Acta Radiol. 2012;53(3):278-84
- Kalpana, R. A Study On Principal Branches of Coronary Arteries In Humans. J Anat. Soc. India. 2003; 52(2) 137-140.
- Luis Ernesto Ballesteros Acunã, Luis Miguel Ramírez Aristeguieta, Saldarriaga Bladimir Telle. Morphological description and clinical implications of myocardial bridges: an anatomical study in colombians. Arq Bras Cardiol 2009;92(4):242-248.
- Nasr AY. Myocardial bridge and coronary arteries: morphological study and clinical significance.Folia Morphol (Warsz). 2014;73(2):169-82.
- Loukas M, Curry B, Bowers M, Louis RG Jr, Bartczak A, Kiedrowski M, Kamionek M, Fudalej M, Wagner T.The relationship of myocardial bridges to coronary artery dominance in the adult human heart.J Anat. 2006 Jul;209(1):43-50.
- VK Bharambe, V Arole.The study of myocardial bridges. J Anat Soc India 57 (1),14-21.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License