IJCRR - 10(12), June, 2018
Pages: 08-11
Date of Publication: 22-Jun-2018
Print Article
Download XML Download PDF
A Case Report of Cytomegalovirus Esophagitis in an Immune-competent Patient
Author: Dosieah Pooja, Jagessar Sabreen, Zhang Zhenyu
Category: Healthcare
Abstract:Cytomegalovirus (CMV) esophagitis usually occurs in immunocompromised individuals. Cases of Cytomegalovirus esophagitis in immunocompetent patients have not been reported yet in China. This report is mainly based on a case study and the relevant literature review to summarize the clinical manifestations, endoscopic characteristics, diagnosis and treatment of cytomegalovirus
esophagitis in immunocompetent patients.
Keywords: Cytomegalovirus, Esophagitis, Immune competent, Literature review
Full Text:
Cytomegalovirus (CMV) can cause various kinds of diseases in the human body, such as encephalitis, retinitis, hepatitis, pneumonia and so on [1,2,3]. Cytomegalovirus gastroenteritis
is rare, but esophagitis is the second most common gastrointestinal manifestation of cytomegalovirus (CMV) infection after colitis [4]. It usually occurs in patients with immunodeficiency, such as HIV infection, history of organ transplantation, long-term history of renal dialysis, and long-term use of immunosuppressant [5].
There is currently growing proof of CMV infection in immunocompetent patients [6,7,8]. Here, we present a case of CMV esophagitis in an immunocompetent patient, who presented with severe progressive chest pain and dysphagia. The patient was successfully treated with ganciclovir. This positive outcome has been added to an updated review of the literature relating to CMV esophagitis in immunocompetent hosts.
Case Presentation
A 71-year-old male patient was admitted to the hospital on April 15, 2016 following 20 days of progressive chest pain and dysphagia. After eating, he constantly had difficulty swallowing, but had no symptoms like nausea and vomiting, melena, cough and sputum, chills or fever.
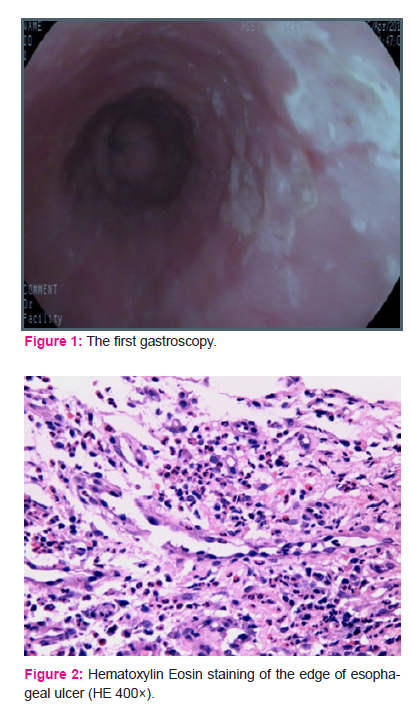
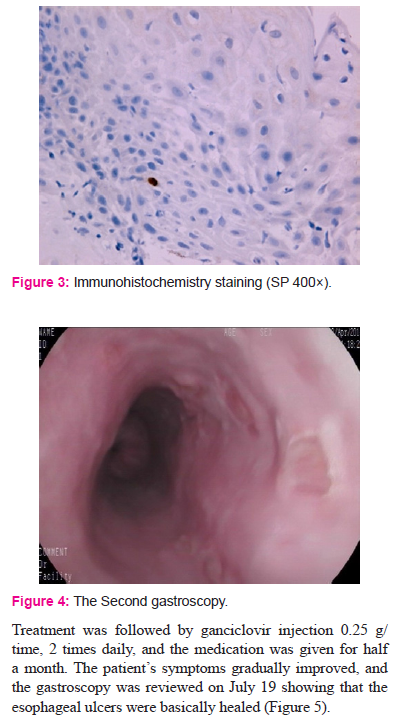
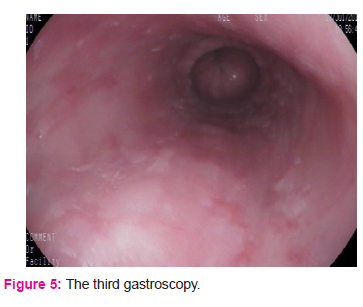
Upon referral, the patient underwent esophagogastroduodenoscopy (EGD), shown in Figure 1, which revealed a rough esophageal mucosa, scattered multiple ulcers were visible about 30-36cm from the incisor teeth, covered with a thin white coating, surrounded by slightly hyperemic peripheral mucous membrane which was altogether diagnosed as multiple esophageal ulcers. The patient had a history of hypertension, cerebral infarction, but no oral antiplatelet drugs. After admission, for acid suppression and mucosal protection, symptomatic and supportive care was given. There was no obvious abnormality in the blood routine examination, urine test, Biochemistry examination, tumor marker, blood transfusion test, anti nuclear antibody, anti neutrophil cytoplasmic antibody, enhanced CT of the chest and abdomen. Other laboratory results showed: Cytomegalovirus IgM antibody (-), cytomegalovirus IgG antibody (+), cytomegalovirus DNA (-), EB virus early antigen IgG (-), EB virus shell antigen IgA (-), EB virus nuclear antigen IgA (-). Colonoscopy results revealed colorectal polyps, which was then treated with EMR (Endoscopic Mucosal Resection). Postoperative pathology results showed tubular adenoma of the sigmoid colon and rectum with glandular low-grade intraepithelial neoplasia. A high-grade intraepithelial neoplasia was found in the focal point. Gastroscopic pathology (Shown in Figure 2) revealed esophageal ulcers and more inflammatory cell infiltration with granulation tissue, scattered macrophages, multiple inflammatory cell infiltration in the middle of squamous epithelium. Immunohistochemistry (shown in Figure 3) revealed HSV-1 (-), CMV (+). After treatment, the patient’s symptoms were slightly improved. On April 22, another gastroscopy was performed. As shown in Fig. 4, 6-8 shallow ulcers were seen at a distance of 30-36 cm from the incisors, and the size varied from 0.4cm to 0.4cm to 0.6x0.6cm. The boundary was well defined and clear. The base was smooth
and the mucosa between the lesions was normal. After the first endoscopic immunohistochemistry, CMV was found positive.
DISCUSSION
The cytomegalovirus (CMV) belongs to the herpes virus family and DNA virus and can be infected through placenta, contact, injection, blood transfusion, or organ transplantation. Once a person has CMV infection, he or she always carries the virus for life. Cytomegalovirus esophagitis usually occurs in immunocompromised patients, such as HIV infection, organ transplantation, long-term use of immunosuppressive patients, etc. The older age of onset may be due to the weakening of immunity of older patients and the decrease of resistance [9], and more basic diseases of the elderly, such as chronic obstructive pulmonary disease, hypertension, diabetes, etc. Some medicines used to treat underlying diseases may damage the digestive tract and are more susceptible to cytomegalovirus infection.
In patients with normal immune function, cytomegalovirus esophagitis mainly presents with chest pain, swallowing pain, hematemesis, and melena, as well as patients with weight loss, difficulty in swallowing, etc. Cytomegalovirus esophagitis in immunocompetent patients and immunodeficient patients showed similar clinical symptoms, which is consistent with previous reports [10]. Endoscopic manifestations of esophageal mucosal erosion, ulcers, erosions and
ulcers often occur in the lower esophagus, but also occur in the upper esophagus. Ulcers are often multiple, and can also be solitary. The borders of ulcers are smooth and the base is
knife-cut or coated with a small amount of white moss.
The key to the diagnosis of cytomegalovirus esophagitis is the discovery of cytomegalovirus inclusion bodies in the nucleus of the biopsy tissue. Since cytomegalovirus often infects fibroblasts and endothelial cells, cytomegalovirus inclusion bodies are easily found on the base of ulcers. Therefore, biopsy specimens should be taken from the base of ulcers, which can increase the detection rate of inclusion bodies [11,12]. There are also opinions that biopsies should be taken from the edge of the ulcer and multinucleated giant cells or nuclear inclusions can be found [13]. Positive cytomegalovirus immunohistochemistry is considered the “gold
standard” for the diagnosis of cytomegalovirus esophagitis [14]. In addition, serological tests, PCR methods for the detection of DNA, serum, or urine culture are important auxiliary diagnostic methods [15].
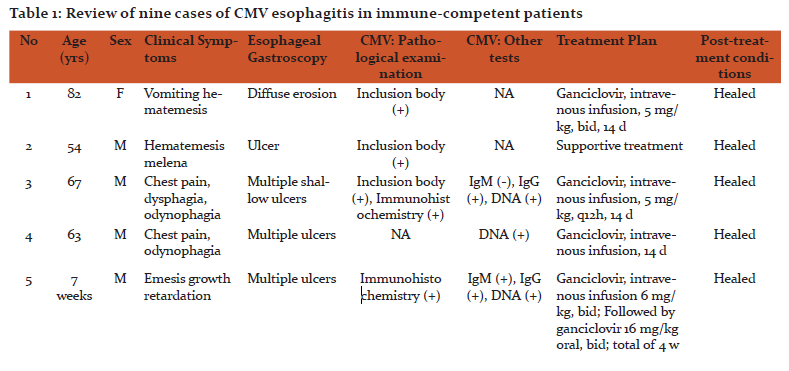
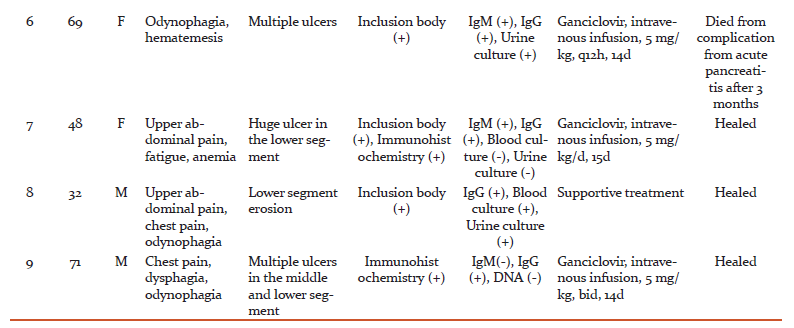
The treatment of cytomegalovirus esophagitis, the most widely used is the intravenous infusion of ganciclovir, treatment for at least 2-3 weeks [16], for ganciclovir intolerance, can be considered with foscarnet sodium [17]. Antiviral therapy is particularly important for patients with immunodeficiency. In the study done, (shown in table 1) 9 patients with normal immune function and 7 patients were treated with ganciclovir. However, it is worth noting that another 2
patients were cured with supportive treatment alone.
In summary, although cytomegalovirus esophagitis is rare in patients with normal immune function, when esophageal ulcers and diffuse erosions are detected by gastroscopies,
the possibility of cytomegalovirus esophagitis must be considered when the cause of common esophagitis is excluded. Cytomegalovirus related tests should be performed, especially pathological examination. Once diagnosed, antiviral treatment may be considered. However,
whether antiviral treatment must be necessary, further studies are still needed.
CONCLUSION
In conclusion, we have portrayed our perceptions of one immune competent patient with CMV esophagitis and have checked on nine detailed cases. This data demonstrates that CMV esophagitis can cause critical morbidity, even in immune competent patients, and support leading substantial examinations to decide the clinical helpfulness of ganciclovir
treatment.
ACKNOWLEDGEMENT
I would like to extend my gratitude to my professor, Dr. Zhang Zhen Yu and my colleague Dr Tan Lu Xuan for encouraging me and helping me in writing this article.
I am also grateful to all the authors, editors and publishers of all those articles, journals and books from where the literaturefor this article has been reviewed and discussed.
Source of Funding: No funding
Conflict of Interest: No conflict of interest.
References:
1. Goodgame RW. Gastrointestinal Cytomegalovirus Disease. Ann Intern Med. 1993;119:924–935.
2. Wenshi T. Changes of miRNA levels in peripheral blood before and after treatment in patients with hepatitis syndrome caused by human cytomegalo virus [J]. Chinese Journal of Gastroenterology and Hepatology, 2016, 25 (2):178-180.
3. Dong W U, HongY, Yue L I, et al. Clinical features of pulmonary abnormalities associated with inflammatory bowel disease [J]. Chinese Journal of Gastroenterology and Hepatology, 2016, 25 (10):1132-1135.
4. Wang H W, Kuo C J, Lin W R, et al. The clinical characteristics and manifestations of cytomegalovirus esophagitis [J]. Dis Esophagus, 2016, 29 (4):392-9.
5. Patel N C, Caicedo R A. Esophageal infections: an update[J]. Curr Opin Pediatr, 2015, 27 (5):642-8.
6. T. G. Wreghitt E. L. Teare O. Sule R. Devi P. Rice. Clinical Infectious Diseases, Volume 37, Issue 12, 15 December 2003, Pages 1603–1606,
7. Rafailidis PI, Mourtzoukou EG, Varbobitis IC, Falagas ME. Severe cytomegalovirus infection in apparently immunocompetent pa- tients: a systematic review. Virol J 2008; 5: 47.
8. Limaye AP, Leisenring WM, Boeckh M. Reactivation of Cytomegalovirus Infection in Critically Ill Immunocompetent Patients— Reply. JAMA. 2008;300(20):2367–2368. doi:10.1001/
jama.2008.697
9. Akin S, TufanF, BahatG, et al. Cytomegalovirus esophagitis precipitated with immunosuppression in elderly giant cell arteritis patients[J]. Aging Clin Exp Res, 2013, 25 (2): 215-8.
10. Demir D, Doganavsargil B, Sarsik B, et al. Is it possible to diagnose infectious oesophagitis without seeing the causative organism? A histopathologicalstudy[J]. Turk J Gastroenterol, 2014, 25 (5):481-7.
11. Kanda K, Kume K, YoshikawaI, et al. Cytomegalovirus esophagitis with massive upper GI hemorrhage [J]. Gastrointest Endosc, 2004, 59 (6):741-3.
12. Sharaf R N, Shergill A K, Odze R D, et al. Endoscopic mucosal tissue sampling [J]. Gastrointest Endosc, 2013, 78 (2):216-24.
13. O’Rourke A. Infective oesophagitis: epidemiology, cause, diagnosis and treatment options[J]. Curr Opin Otolaryngol Head Neck Surg, 2015, 23(6):459-63.
14. Ozaki T, YamashitaH, KanekoS, et al. Cytomegalovirus disease of the upper gastrointestinal tract in patients with rheumatic diseases: a case series and literature review[J]. Clin Rheumatol, 2013, 32 (11):1683-90.
15. Reggiani B L, LosiL, Di Gregorio C, et al. Cytomegalovirus infection of the upper gastrointestinal tract: a clinical and pathological study of 30 cases[J]. Scand J Gastroenterol, 2011, 46(10):1228-35.
16. Ahuja N K, Clarke J O. Evaluation and Management of Infectious Esophagitis in Immunocompromised and Immunocompetent Individuals [J]. Curr Treat Options Gastroenterol, 2016, 14(1):28-38.
17. BacigalupoA, Boyd A, Slipper J, et al. Foscarnet in the management of cytomegalovirus infections in hematopoietic stem cell transplant patients [J]. Expert Rev Anti Infect Ther, 2012,
10(11):1249-64.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License