IJCRR - 10(11), June, 2018
Pages: 07-10
Date of Publication: 11-Jun-2018
Print Article
Download XML Download PDF
Prevalence of Molar-Incisor Hypomineralization in 7-13 Years Old Children of Biratnagar, Nepal: A Cross Sectional Study
Author: Deep Jitendra Meisheri, Ashwin Devasya, Giri DK, Ravi Acharya, Jha MS
Category: Healthcare
Abstract:Background: Molar incisor hypomineralization (MIH) describes the clinical picture of hypomineralization of systemic origin affecting one or more first permanent molar and incisors. Although the reported prevalence of MIH ranges from 2.4% to 40.2% worldwide, very little data is available from Nepal.
Objective: To assess the prevalence of MIH in children aged 7-13 years of Biratnagar, Nepal.
Study design: This cross-sectional descriptive study consisted of 567 children aged 7-13 years selected by cluster sampling method. Examinations were performed by one calibrated pediatric dentist. The European Academy of Pediatric Dentistry (EAPD) 2003 criteria was used for diagnosis.
Results: The prevalence of MIH was 8.6% in the age group of 7 to 13 years. The prevalence of MIH was 8.33% in males and 9.01% in females. The prevalence and severity of MIH increased with increase in age. The prevalence of MIH was 10.54% in the age group of 10 to 13 years as compared to 5.95% in the age group of 7-9 years.
Conclusion: The prevalence of MIH was 8.6% in the age group of 7 to 13 years. Developmental dental defects hold significance for scientists and practitioners from both medicine and dentistry. Dental interest has recently swung toward Molar Hypomineralisation. MIH imposes a significant burden on global health and has potential to become medically preventable, being linked to infantile illness.
Keywords: First permanent molars, MIH in Nepal, Molar-incisor hypomineralization
Full Text:
INTRODUCTION:
Developmental dental defects hold significance for scientists and clinicians from both medicine and dentistry. Dental interest has recently swung toward Molar Incisor Hypomineralisation (MIH), a prevalent condition characterized by well-demarcated opacities in enamel. Molar incisor hypomineralization is defined as the developmentally derived dental defect that involves hypomineralization of one to four permanent molars, frequently associated with similarly affected permanent incisors.[1] MIH is also named as idiopathic enamel hypomineralization, nonfluoride hypomineralization in first permanent molars, and cheese molars.[2,3,4] The condition is attributed to disruption of ameloblastic activity during the transitional and maturational stages of ameloblasts.[5] MIH clinical appearance may vary from white to yellow opacities and from soft to porous enamel. The porous enamel when subjected to masticatory stress lead to post eruptive breakdown of enamel, making tooth susceptible to thermal and cold stimuli.
The MIH prevalence varies from 2.4% to 40.2% globally. [1] Most of the studies have been carried out in Northern Europe and the rates between 3.6% and 25% were reported. The reported prevalence of MIH varied from 2.4% in Germany and Bulgaria, 40% in Leeds, and 44% in Sydney. [1,3,4] Very little data is available for the prevalence of MIH in children in Nepal. The objective of this study is to assess the prevalence of MIH in children aged 7-13 years of Biratnagar, Nepal.
Materials and methods
The study was approved by the Institutional Review Committee of the Nobel Medical College Teaching Hospital. The nature and purpose of the study was explained to the heads of the schools and prior permission was obtained to conduct the survey in their schools. The study was conducted during the period of Oct-Feb 2017/18.
Study Population
The study population consisted of 600 children aged 7-13-yrs old recruited from the schools. The socio-economic status was almost similar and rated low moderate according to parental education and occupation. A cluster sampling method was used in this study (schools as clusters). The children with generalized hypoplastic/hypomineralized defects, such as amelogenesis imperfecta and those suffering from any chronic illness were excluded from the present study.
Selection Criteria
All the children who participated in the present study were instructed to brush prior to the clinical examination. The status of permanent incisors and molars was evaluated and recorded, according to the European Academy of Paediatric Dentistry (EAPD) 2003 criteria.[1] Teeth were inspected visually in daylight with a torch, while the child is seated in an ordinary chair by a single pediatric dentist. To examine, sterilized mouth mirror and probe were used. The probe was occasionally used to remove plaque. All the children diagnosed with MIH were reexamined by a second investigator to rule out any discrepancy. The entire indexed tooth was kept wet while examination to rule out opacities due to excessive drying, and the size of lesion was not taken into consideration.
Statistical Analysis:
Statistical analysis was performed using the Statistical package for the Social Sciences (SPSS) (SPSS Inc, Version 16 Chicago, IL, USA) to analyze the data. Karl Pearson Chi-square test is used to compare the proportions. Differences were considered statistically significant if P ≤ 0.05.
Results:
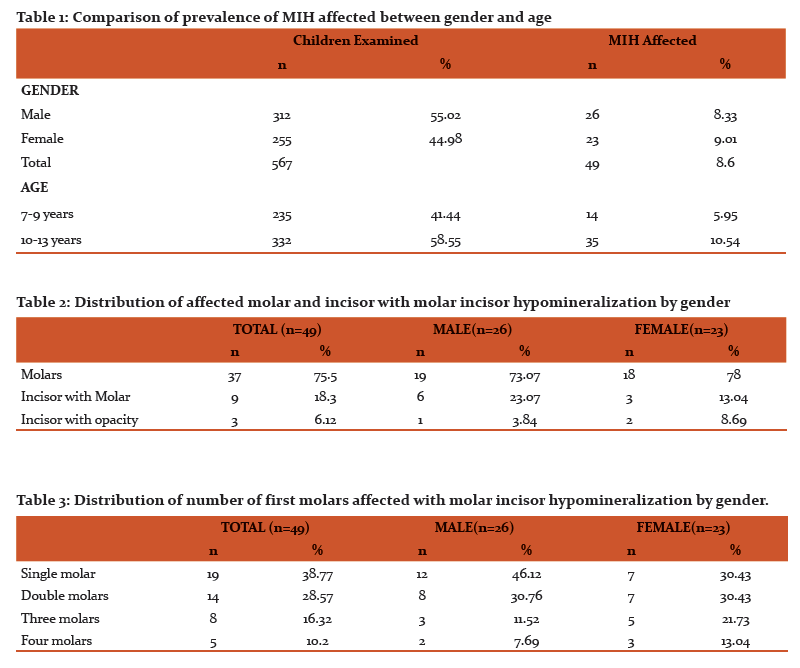
In total, 600 children aged 7 to 13 years were examined of which 567 were included in the study. Data of 49 children diagnosed with MIH were statistically analyzed. The interexaminer agreement was good (kappa = 0.879). A total of 26 male and 23 female children were diagnosed with MIH. Distribution of the subjects by age and gender is presented in (Table 1). Prevalence of hypomineralized lesions was assessed; the majority of children were unaffected, whereas 49 (8.6%) had either molar/incisor or both affected with MIH. The children diagnosed were divided into three categories on the basis of tooth affected, viz., molars, molars with incisors, and incisors with opacities. 37(75.5%) children had only molars affected compared to 9(18.3%) which had both incisors and molars affected. Only 3(6.12%) children had only incisors with opacities. (Table 2)
MIH in single molars were the most common finding at 38.77% with all the four molars least affected at only 10.2%. (Table 3)
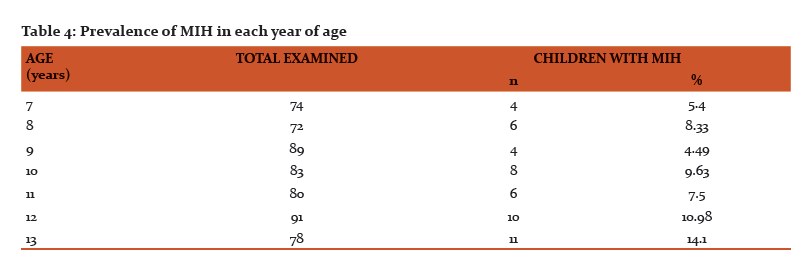
The prevalence of MIH was 8.6% in the age group of 7 to 13 years. The prevalence of MIH was 8.33% in males and 9.01% in females. The prevalence and severity of MIH increased with increase in age. The prevalence of MIH was 10.54% in the age group of 10 to 13 years as compared to 5.95% in the age group of 7-9 years. (Table 4)
Discussion:
In our study, the prevalence of MIH was found to be 8.6%, which was well within the range observed in other studies conducted in various parts of the world. As far as Asia was concerned the prevalence rate was estimated to be the least (2.8%) in Hong Kong and highest (18.6%) in Iraq (2003-2011). [6-8] No significant correlation was found between age groups and the number of affected teeth. The present study also found 18.3% of children diagnosed with MIH presented lesions in both permanent first molars and incisors which is much lower than global values. [9-14]The incisors of the MIH affected children revealed demarcated enamel opacities and enamel loss with higher rate of opacities. This finding tends to be in line with most other studies which found affected incisors to have rarely exhibited posteruptive breakdown because of the absence of masticatory forces upon these surfaces. [15-21] One possible limitation for this study may be the association of MIH with past medical history which was not possible due to lack of information available with the parents and schools. Future studies can overcome this limitation by using the child’s medical records and thorough history given by parents. There is also a need to better understand the condition in the country of Nepal. There is also a need for longitudinal studies with large sample size to better obtain the prevalence rate and also understand the etiological factors associated with MIH in Nepal.
Conclusion:
The present study reports a prevalence of 8.6% in children of age group 8 to 12 years. Thus, MIH is a frequently occurring dental ailment in the pediatric population. Children with MIH require therapy shortly after tooth eruption. This study shows that the severity of MIH lesions increases with age. Therefore, dentists must be aware of the clinical consequences and pay special attention to children with MIH. This data could be helpful in estimating the baseline data of MIH among the Nepalese population. The first step in effective management of MIH should be the implementation of comparable, representative studies of MIH prevalence among different populations throughout the world. The awareness about the condition would help in the preventive and therapeutic measures for combating this alarming developmental disturbance of teeth which is also of relevance for public health authorities.
References:
-
Weerheijm KL, Duggal M, Mejàre I, Papagiannoulis L, Koch G, Martens LC, Hallonsten AL. Judgement criteria for molarincisor- hypomineralisation (MIH) in epidemiologic studies: a summary of the European meeting on MIH held in Athens, 2003. Eur J Paediatr Dent 2003 Sep;4(3):110-113.
-
Koch G, Hallonsten AL, Ludvigsson N, Hansson BO, Holst A, Ullbro C. Epidemiologic study of idiopathic enamel hypomineralisation in permanent teeth of Swedish children. Community Dent Oral Epidemiol 1987;15:279-85.
-
Leppäniemi A, Lukinmaa PL, Alauusua S. Nonfluoride hypomineralizations in the permanent first molars and their impact on the treatment need. Caries Res 2001;35: 36-40.
-
van Amerongen WE, Kreulen CM. Cheese molars: A pilot study of the etiology of hypocalcifications in first permanent 1st molars. ASDC J Dent Child 1995;62:266-9.
-
Dietrich G, Sperling S, Hetzer G (2003) Molar incisor hypomineralisation in a group of children and adolescents living in Dresden (Germany). Eur J Paediatr Dent 4: 133-137.
-
Garg N, Jain AK, Saha S, Singh J. Essentiality of early diagnosis of molar incisor hypomineralization in children and review of its clinical presentation, etiology and management. Int J Clin Pediatr Dent 2012;5:190-6.
-
Ghanim A, Morgan M, Mariño R, Bailey D, Manton D. Molar-incisor hypomineralisation: Prevalence and defect characteristics in Iraqi children. Int J Paediatr Dent 2011;21:413-21.
-
Ahmadi R, Ramazani N, Nourinasab R. Molar incisor hypomineralization: A study of prevalence and etiology in a group of Iranian children. Iran J Pediatr 2012;22:245-51.
-
Muratbegovic A, Markovic N, Ganibegovic Selimovic M. Molar-Incisor Hypomineralization in Bosnia and Herzegovina: Aetiology and clinical consequences in medium caries activity population. Eur Arch Paediatr Dent 2007;8:189-94.
-
Alaluusua S, Lukinmaa PL, Vartiainen T, Partanen M, Torppa J, Tuomisto J. Polychlorinated dibenzo-p-dioxins and dibenzofurans via mother’s milk may cause developmental defects in the child’s teeth. Environ Toxicol Pharmacol 1996;1:193-7.
-
Jasulaityte l, Veerkamp JS, Weerheijm KL. Molar-incisor hypomineralization: Review and prevalence data from a study of primary school children in Kaunas/Lithuania. Eur Arch Paediatr Dent 2007;8:87-94.
-
Cho SY, Ki Y, Chu V. Molar incisor hypomineralization in Hong Kong Chinese children. Int J Paed Dent 2008;18:348-52.
-
Lygidakis NA, Dimou G, Briseniou E. Molar-incisor hypomineralization (MIH). Retrospective clinical study in Greek children. I. Prevalence and defect characteristics. Eur Arch Paediatr Dent 2008;9:200-6.
-
Zawaideh FI, Al-Jundi SH, Al-Jaljoli MH. Molar-Incisor Hypomineralization: Prevalence in Jordanian children and clinical characteristics. Eur Arch Paediatr Dent 2011;12:31-6.
-
Suckling GW, Brown RH, Herbison GP. The prevalence of developmental defects of enamel in 696 nine-year-old New Zealand children participating in a health and development study. Community Dent Health 1985;2:303-13.
-
Condo R, Perugia C, Maturo P. MIH: epidemiologic clinical study in paediatric patients. Oral and Implantology Anno V-N. 2-3/2012.
-
Beentjes VEVM, Weerheijm KL, Groen HJ. Factors involved in the aetiology of molar-incisor hypomineralisation. Eur J Paediatr Dent 2002 Mar;3(1):9-13.
-
Alaluusua S. Aetiology of molar incisor hypomineralization: a systematic review. Eur Arch Paediatr Dent 2010 Apr;11(2): 53-58.
-
Kreshover SJ, Clough OW. Prenatal influences on tooth development II. Artificially induced fever in rats. J Dent Res 1953 Aug;32(4):565-577.
-
Alaluusua S, Lukinmaa PL, Koskimies M, Pirinen S, Hölttä P, Kallio M, Holttinen T, Salmenperä L. Developmental dental defects associated with long breast feeding. Eur J Oral Sci 1996 Oct-Dec;104(5-6):493-497.
-
Whatling R, Fearne JM. Molar incisor hypomineralization: a study of aetiological factors in a group of UK children. Int J Paediatr Dent 2008 May;18(3):155-162.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License