IJCRR - 10(9), May, 2018
Pages: 15-21
Date of Publication: 05-May-2018
Print Article
Download XML Download PDF
Histopathological Pattern of Ovarian Tumours \? An Experience
Author: Manzoor Ahmad Sofi, Nusrat Bashir, Afshan, Arvind Khajuria, Nausrat Ali
Category: Healthcare
Abstract:Background: Ovarian neoplasms exhibit a wide variation in structure and biological behaviour. There are numerous types of ovarian tumours, and over all they fall into benign, borderline, and malignant categories. Ovarian carcinoma represents the sixth most common female cancer and the fourth leading cause of death due to cancers in women.
Aims: To study the clinical presentation and pathological patterns of ovarian tumours.
Materials and Methods: The clinicopathological study was at ASCOMS Sidra Jammu, in the department of pathology. This was a prospective observational study conducted over a period od 1 year (Nov 2014 to Oct 2015).
Results: A total of 189 cases of ovarian lesions were studied, of which 119 were neoplastic and 70 were non-neoplastic. Maximum cases 26.1% were reported in the age group of 41-50 years. Among 70 non-neoplastic lesions, luteal cyst was commonest comprising 48.5% of total non-neoplastic lesions. Of 119 neoplastic lesions 56.3% were benign, 1.7% were borderline and 42% were malignant. Tumours were classified as per WHO classification 2003. The surface epithelial group formed the largest group constituting 74.8% of all the ovarian neoplasms, followed by germ cell tumours (16%), metastatic tumours (5.9%), sex cord stromal tumours (1.7%) and miscellaneous (0.84%). Among the individual neoplasms, serous tumours were the commonest (59.7%), followed by teratomas (13.4%). One case each of endometriod carcinoma, clear cell carcinoma, mixed epithelial carcinoma, thecoma, fibroma, yolk sac tumour, struma ovarii and lymphangioma was also reported in the present study.
Conclusion: Ovary is a frequent site of primary and metastatic tumors. Due to its complex structure, primary ovarian neoplasms are of diverse histological types. Our observations and results proved to be valuable baseline information regarding patterns of ovarian tumors in our population. More studies, to define the risk factors in our population and to identify specific etiological factors, are recommended.
Keywords: Ovarian, Histopathology, Neoplasms
Full Text:
Introduction:
Ovaries are paired pelvic organs that lie on either side of the uterus close to lateral pelvic wall, behind the broad ligament and anterior to the rectum1. During the reproductive period, there average size is 4 X 2 X 1 cm, and there average weight is 5 to 8g; after menopause, they shrink to one half or less of this size2. Ovarian neoplasms exhibit a wide variation in structure and biological behaviour3. There are numerous types of ovarian tumours, and over all they fall into benign, borderline, and malignant categories4. Benign ovarian cysts may occur at any point in life but they are most common during childbearing age and constitute about 90% of ovarian tumours. These occur mostly in young women between the ages of 20 and 45 years, borderline tumours occur at slightly older ages. Malignant tumours are more common in older women, between the ages of 45 and 65 years5. Ovarian carcinoma represents the sixth most common female cancer and the fourth leading cause of death due to cancers in women6. It varies widely in frequency among different geographic regions and ethnic groups, with a high incidence in Northern Europe and low incidence in Japan7. In United States it accounts for 4% of all cancer in women and 5% of estimated cancer deaths. In Eastern India, the fourth most frequent reported malignancy in females was ovarian8. Asian countries and Japan have rates of 2–6.5 new cases per 100,000 women per year 9. The majority of cases are sporadic, and only 5-10% of ovarian cancers are familial7. A number of epidemiologic studies have evaluated a variety of risk factors for ovarian tumour. To date, these risk factors include: age´ chronic inflammation and non-steroidal anti-inflammatory drug (NSAID) use, diet, ethnicity, hysterectomy, infertility, drug use, obesity, low parity, smoking, and talc use/asbestos exposure. Use of combined oral contraceptive pills is a protective factor. According to the National Cancer Institute (NCI), a woman without a family history of ovarian cancer has a 1 in 55 lifetime chance of developing ovarian cancer10. This risk increases 10-fold when known familial/hereditary conditions exist11. As such, patients with a history suspicious for a hereditary breast-ovarian cancer syndrome (BRCA1 or BRCA2) or hereditary nonpolyposis colorectal cancer syndrome, are at increased risk for development of a malignant mass12. Early diagnosis of ovarian tumours is a challenge to the gynaecologists, mainly due to the fact that symptoms in early disease are vague and non-specific5. Although some of the specific tumours have distinctive features and are hormonally active, most are non- functional and symptom free with non-specific signs until they attain a large size7. By the time an ovarian malignancy is diagnosed, about two-thirds of these have already become far advanced3. The present study is undertaken to study the frequency and diverse histomorphological patterns of ovarian lesions in this part of region. This information will hopefully help in arriving at specific diagnosis which will improve the quality of treatment and prognosis of the patient.
Materials and methods:
This clinicopathological study was conducted at ASCOMS sidhra Jammu, J and in the Department of Pathology. This was a prospective observational study conducted over a period of 1year (Nov,-2014- Oct , 2015).
Inclusion criteria
All the specimens of ovarian lesions both neoplastic as well as non-neoplastic were included. The detailed clinical information of all of these patients was collected as per the pro-forma.
Methodology
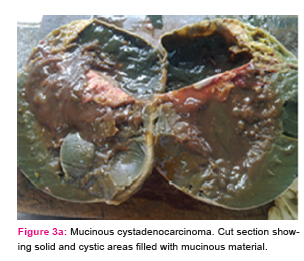
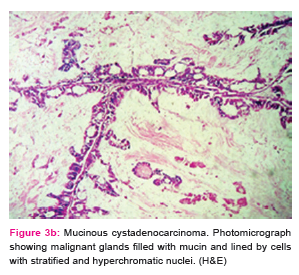
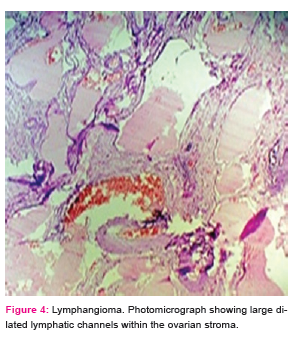
The specimens obtained after surgical exploration of patient were examined grossly and then sectioned by conventional method after overnight fixation by 10% formalin. Gross photographs of the specimens were taken to represent various tumour types. Minimum of four sections from the tumour were taken.
The tissue was processed as per standard procedure. The lesions were studied and classified as per the WHO classification of ovarian tumours (2003). Microphotographs of tumours were taken to represent various histological variants of ovarian tumours.
Results:
The present study was a one year prospective observational study conducted in the Department of Pathology at ASCOMS Jammu from Nov 2014 to Oct , 2015.
A total of 189 cases of ovarian lesions were studied, of which 119 were neoplastic and 70 were non-neoplastic. Of the 119 neoplastic ovarian specimens evaluated, 67 (56.30%) harboured benign ovarian tumour; 2 cases (1.70%) were having borderline tumours whereas 50 cases (42.0%) had malignant lesions. (Table-1). The ages of patients ranged from 1 month to 70 years. Maximum cases, 31 (26.1%) were reported in the age group of 41-50 years. Malignant tumours presented in higher age group than benign tumours. 58.2% of benign ovarian neoplasms were seen in patients less than 40 years of age where as 58% of malignant neoplasms were seen in patients more than 40 years of age. Non-neoplastic lesions occurred in all groups but majority occurred in the age group of 20-40 years, accounting for 68.6%.
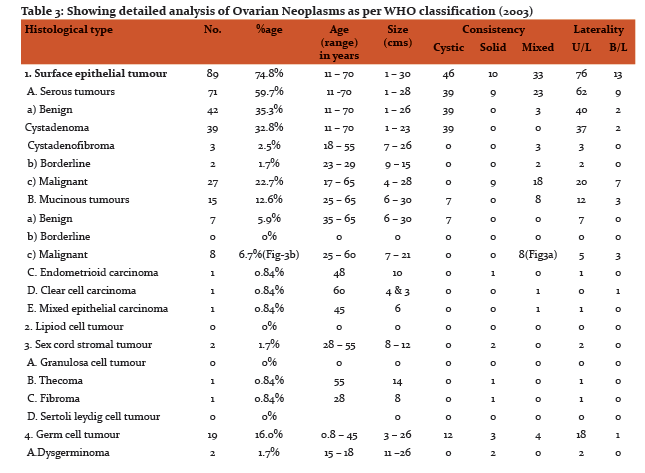
The commonest symptom with which the patients presented was abdominal pain/discomfort, 77 cases (64.7%). Abdominal swelling/distension was present in 64 patients (53.8%). Ascites was seen in 26 patients (21.8%). All the cases with ascites were associated with malignancy except for one benign mucinous cystadenoma (Fig-1a,Fig1b) which had ruptured. Associated menstrual disturbances in the form of amenorrhea, polymenorrhea, dysmenorrhea and metrorrhagia were seen in 8.4% of cases. (Table-2). Among non-neoplastic cases majority, 30 (42.6%) were asymptomatic and came to attention when being investigated for an unrelated condition. Among the symptomatic cases majority presented with pain (40%) followed by Pain with menstrual irregularity (8.6%). The occurrence of ovarian tumour is more among nulliparous (25.2%) and those with parity of less than 3 (49.6%) as compared to those with parity of more than three (25.2%). Out of 119 cases 101 cases (84.9%) had unilateral involvement. Of these, right sided tumours, 71 cases (59.7%) were more common than left sided tumours, 30 cases (35.7%). There were 18 cases (15.1%) which were having bilateral ovarian involvement. Among the benign tumours 63 cases (94.0%) were unilateral and 4 cases (6%) were bilateral. Thirty six (72%) malignant tumours had unilateral involvement with 25 cases (50%) showing right sided involvement. Bilateral involvement was seen in 14 cases (28%).
The frequency of bilateral tumours was more for malignant tumours i.e. 14 cases (11.8% of all the ovarian neoplasms) while 4 cases (3.4% of all ovarian neoplasms) were benign. For non –neoplastic lesions majority of the cases, 88.6%, were unilateral. About 60% of the total non-neoplastic tumours were on the right size and 28.6% were on the left. Bilateral tumours comprised 11.4% of the total non-neoplastic lesions.
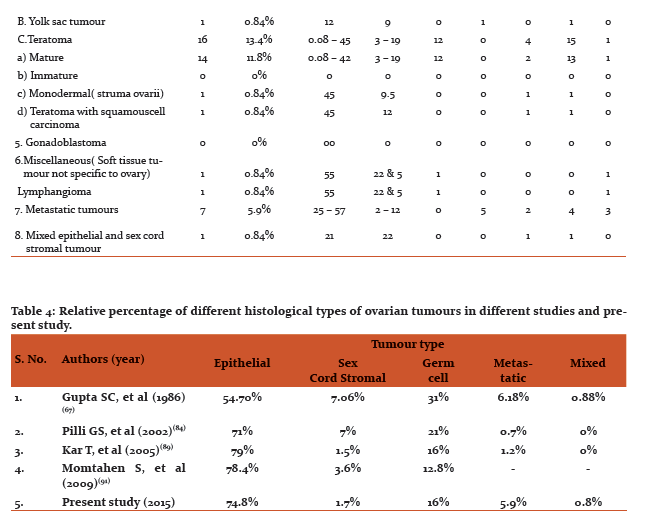
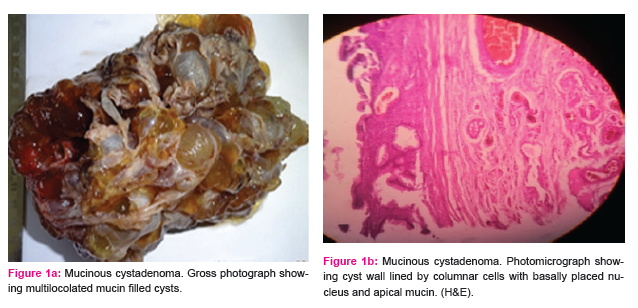
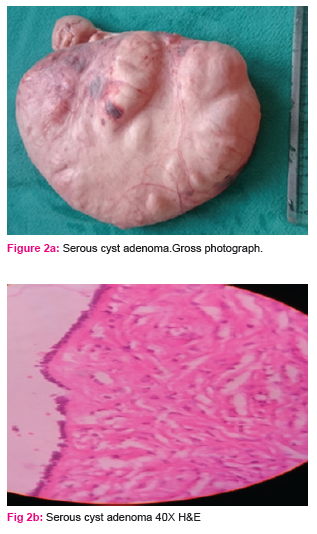
Most commonly occurring malignant lesion was serous cystadenocarcinoma (7 cases), comprising 38.9% of bilateral ovarian neoplasms. The most common benign lesion was benign serous cystadenoma (2 cases), comprising 11.1% of bilateral ovarian neoplasms. On gross examination tumours ranged in size from 1 to 30 cm with majority, 76 (63.8%) falling in the range of 1-10 cm. The smallest tumour measured 1X1X1cm in size and was diagnosed as benign serous cystadenoma. The largest tumour measured 30x25x22 cm and was reported as benign mucinous cystadenoma (Fig 2a,Fig 2b). Out of 119 neoplastic lesions 49.6% were cystic neoplasms, 16.8% were solid and 33.6% showed mixed consistency. Among non –neoplastic tumors 94.3% of the cysts ranged in size from 1-10 cm. Minimum size of the tumour was 2.5 cm and maximum was 15 cm. Tumours arising from the surface epithelium formed the largest group, 89 cases comprising 74.8% of total ovarian neoplasms. These were followed by 19 cases of Germ cell tumours (16.0%). 2 cases (1.7%) were reported as sex cord stromal tumour. 7 cases (5.9%) of metastatic ovarian tumour were also reported. Benign surface epithelial tumours constituted 73.1% of all benign neoplasms and its malignant counterpart constituted 76.0% of all malignant neoplasms. Table-3 shows detailed analysis of histopathological pattern of ovarian neoplasms in our study as per WHO system (2003).
Discussion:
The ovary is a frequent site for both primary and metastatic tumours. Due to its complex structure, the neoplasms arising from the ovary inherit a wide spectrum of histogenesis, clinical behaviour and histological types. In recent years, WHO (2003) has proposed a classification for tumours of the ovary based upon its histogenesis. Wider application of this classification has made the clinicopathological data more meaningful.
The observations and analysis of the present study provide a fair insight into the clinical presentation and histopathological pattern of ovarian tumours. The current study presents the data on 189 consecutive cases of ovarian lesions diagnosed in the Department of Pathology, from a tertiary care centre over a period of 1year (Nov , 2014 to Oct , 2015) Out of 189 cases of ovarian lesions studied, 119 were neoplastic and 70 were non-neoplastic. Out of 119 neoplastic ovarian lesions, 67 i.e. 56.30% were labelled as benign, 2 i.e. 1.7% as borderline and 50 i.e. 42.0% as malignant.
Present study is comparable to the studies done by Gupta SC, et al (1986) 21 and Ahmed Z, et al 13. Yasmin S, et al (2008) 14reported lesser incidence of malignant tumours as compared to present study.
In the present study patients ranged in age from 1 month to 70 years, with peak incidence in 3rd and 4th decade i.e., 51 cases (42.8%).
Our study is in concordance with study done by Pilli,et al (2001) 15 and Ramchandran G,et al (1972) 16 where incidence of ovarian neoplastic lesions was more common in 21-40 years of age group. Kar T,et al (2005) 17 reported highest incidence of ovarian tumours in 41-60 years of age group.
Age distributions among benign borderline and malignant ovarian tumours seen in the present study were compared with other studies. In our study, the majority of benign tumours occurred in the age group of 20-39 years. This finding is consistent with the studies by Ramachandran G, et al16 and Mehta and Purandare 18.
Majority of the malignant tumours in the current study were seen in the age group of 40-60 years which is comparable to study done by Ramachandran G, et al 16, Mehta and Purandare (1964) 18 and Arab M, et al 19.
Commonest mode of presentation in our study was abdominal discomfort / pain i.e. 64.7%. Abdominal distension/swelling was observed in 52.0% of patients. Many of the patients had a combination of symptoms. Other symptoms observed were menstrual disturbances, gastrointestinal symptoms and urinary symptoms
Our study concorded well with studies done by Pilli, et al 15and Yasmin S, et al 14 where pain abdomen was the commonest symptom followed by abdominal mass. Ascites was seen in 21.8% of patients. Similar observation was also made in the above mentioned studies.
Out of total 119 cases in our study, 101 were unilateral and 18 were bilateral.
The present study is concordant with the study done by Prabhakar and Maingi 20. Among unilateral neoplasms right sided lesions(59.7%) were more common compared to left sided tumours. The results were comparable with the study done by Ramachandran G, et al 16 who reported 46.04% incidence of right sided lesions.
Out of 18 bilateral cases, 14 (77.8%) were malignant and 4 ( 22.2%) were benign. None of borderline tumour was bilateral. This is comparable to the findings of former workers. In the study done by Prabhakar and Maingi 20 75.9% of bilateral ovarian neoplasms were malignant. These observations indicate a greater association of bilaterality with malignant tumours than with benign or borderline tumours.
Histologically, 119 neoplastic ovarian lesions were classified according to WHO classification. Relative percentage of different histological types of ovarian tumours compared with other studies is shown in the table
Present study conforms to the patterns observed by Kar T, et al 17, Pilli,et al 15 , and less with Gupta SC, et al 21 who comparatively reported higher incidence of germ cell tumours.
In the present study, out of 119 neoplastic lesion 59% (49.6%) were cystic, 20 (16.8%) were solid and 40 (33.6%) had mixed consistency.
Observations in the present study are closer to those made by Couto F22 than with those made by Gupta SC, et al (1986)21
Majority of the benign tumours had cystic consistency (88.1%) and majority (64%) of malignant neoplasm had mixed consistency.
Among the individual neoplasms, serous tumours were the commonest (59.7%), followed by teratomas (13.4%), mucinous tumours (12.6%),metastatic tumours (5.9%) and dysgerminomas (1.7%). One case each of endometriod carcinoma, clear cell carcinoma, mixed epithelial carcinoma, thecoma, fibroma, yolk sac tumour, struma ovarii and lymphangioma (Fig-4) was also reported in the present study. Table 4 shows relative percentage of different histological types of ovarian tumours in different studies and present study. .
Among 70 non-neoplastic lesions, luteal cyst was commonest comprising 48.5% of total non-neoplastic lesions. Follicular cyst comprised 34.3% and endometriotic cysts comprised 17.1% of non-neoplastic lesions.
CONCLUSION
Ovary is a frequent site of primary and metastatic tumors. Due to its complex structure ,primary ovarian neoplasms are of diverse histological types. Our observations and results proved to be valuable baseline information regarding patterns of ovarian tumors in our population. More studies, to define the risk factors in our population and to identify specific etiological factors are recommended.

References:
-
Kurman RJ, Ellenson LH and Ronnett BM. Bluestein's pathology of the female genital tract. 6th edition. Springer New York Dordrecht Heidelberg London. 2011.
-
Rosai and Ackerman’s Surgical Pathology. 10th edition, Elsevier.2011. P.1553-1606.
-
Howkins & Bourne. Shaw’s Text Book of Gynaecology, 15th. Elsevier, A division of Reed Elsevier India Pvt. Ltd.,2011. Chapter 28,29: p. 367-431.
-
Ellenson LH, Edyta C and Pirog. The female genital tract. Robbins and Cotran Pathologic Basis of Disease. 8th edition., Elsevier, A division of Reed Elsevier India Pvt. Ltd., 2010. Chapter 22: p. 1005-1063.
-
Wasim T, Majrroh A, Siddiq S. Comparison of clinical presentation of Benign and Malignant Ovarian Tumours. J Pak Med Assoc.2009;59: 18-21.
-
Tortolero L, Mictchell FM, Rhodes HE. Epidemiology and screening of ovarian cancer. Obstetric Gynecologic Clin North Am 1994;21: 63-75
-
Holschneider CH and Berek JS. Ovarian cancer: Epidemiology, biology, and prognostic factors. Seminars in Surgical Oncology. 2000;19: 3-10.
-
Sen U, Sankaranarayanan R, Mandal S, Ramanakumar AV, Parkin DM, Siddiqi M. Cancer patterns in Eastern India: The first report of Kalkata Cancer Registry. Int J Cancer 2002; 100: 86-91.
-
Murad A. Ovulation induction and ovarian tumours: the debate continues. J Pak Med Assoc 1998 ;48:353-6.
-
Ries LAG, Young JL, Keel GE, Eisner MP, Lin YD, Horner M-J, editors. SEER Program, NIH Pub. No. 07-6215. National Cancer Institute; Bethesda, MD: 2007. SEER Survival Monograph: Cancer Survival Among Adults: U.S. SEER Program, 1988-2001, Patient and Tumour Characteristics.
-
Pike MC, Pearce CL, Peters R, Cozen W, Wan P, Wu AH. Hormonal factors and the risk of invasive ovarian cancer: a population-based case-control study. Fertility and Sterility. 2004; 82 186–95
-
Elit L, Esplen MJ, Butler K, Narod S. Quality of Life and Psychosexual Adjustment after Prophylactic Oophorectomy for a Family History of Ovarian Cancer. Familial Cancer. 2001; 1: 149–56.
-
Ahmed Z, Kayani N, Hassan SH, Muzaffar S, Gill MS. Histological patterns of ovarian neoplasms. J Pak Med assoc.2000;50: 416-9.
-
Yasmin S, Yasmin A, Asif M: Clinicohistological pattern of ovarian tumours in Peshawar Region. J Ayub Med Coll Abbottabad 2008; 20: 11-13.
-
Pilli GS, Suneeta KP, Dhaded AV, Yenni W: Ovarian tumours. A study of 282 cases. J Indian Med Assoc. 2002; 100 : 420,423-24, 447.
-
Ramachandran G, Harilal KR, Chinnamma K, Thangavelu H. Ovarian neoplasms- A study of 903 cases. J Obstetric Gynecologic India. 1972;22: 309-315.
-
Kar T, Kar A, Mohapatra P C. Intra-operative cytology of ovarian tumours. J Obstetric Gynecologic India.2005; 55 : 345-349.
-
Mehta RC, Purandare BN: Clinicopathological study of 149 cases of ovarian neoplasms. J Obstetric Gynae India.1964; 14: 532-542.
-
Arab M, Khayamzadeh M, Tehranian A, Tabatabaeefar M, Hosseini M, Anbiaee R, Golfam F, Akbari ME, et al. Incidence rate of ovarian cancer in Iran in comparison with developed countries. Indian J of Cancer. 2010; 47; 322-7.
-
Prabhakar BR, Maingi Kalyani: Ovarian tumours. Prevalence in Punjab. Indian J Pathol Microbial. 1989; 32: 276-81.
-
Gupta GC, Singh PA, MehrotraTN, Agarwal R: A clinicopathological study of ovarian tumours. Indian J Pathol Microbiol. 1986; 29: 354-62
-
Couto F, Nadkarni NS, Rebello MJ. Ovarian Tumours in Goa: A clinicopathological study. J Obstetric Gynae India.1993;43: 408-12.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License