IJCRR - 10(8), April, 2018
Pages: 10-14
Date of Publication: 28-Apr-2018
Print Article
Download XML Download PDF
Assessment of Changes in Tongue Position in Class II Division 1 Patients Treated with Functional Appliances - An in-vivo Study
Author: Akanksha Kumar, Narendra Sharma, Sunita Shrivastav, Ranjit Kamble, Neha Bhandari
Category: Healthcare
Abstract:Objective: The objective of this study was to evaluate the effects of functional treatment on positional changes in tongue and to determine if any relationship exists between the functional appliance therapy in Class II division 1 and position of tongue.
Material and Method: Pre-treatment and post-treatment lateral cephalographs of 30 Class II division 1 patients within the age group of 8-12 years were taken and traced. After identification of determining landmarks, reference lines were marked and 4 linear measurements were evaluated \? 2 each in horizontal and vertical plane. These linear measurements were compared for reliability using statistical analysis.
Results: Statistically significant (p < 0.05) differences were found in linear measurements indicative of alteration in tongue position in horizontal and vertical direction. There was a significant interrelationship between reduction of ANB angle and movement of tongue in forward direction.
Conclusion: The results suggest that Functional appliances are very effective in altering the position of tongue during treatment of Class II division 1 malocclusion.
Keywords: Tongue, Functional appliance, Class II malocclusion
DOI: 10.7324/IJCRR.2018.10802
Full Text:
Introduction
The form-function debate has always been a perpetual one for the orthodontic community. The effect of facial form on the function and vice-versa has been a subject of great interest and controversy for a research oriented orthodontic clinician.1
Bones grow, as many believed, in a predetermined manner by the genetic code of individual. This predetermined growth may be changed and altered by exposure to altered epigenetic environment or functional environment. Craniofacial form and the factors that alter them have, since many years, intrigued the minds of researchers. Pioneering works by Van der Klaauw and Moss have substantiated the effects of function in changing facial form.2,3
Class II malocclusion is one of the most frequently encountered problems in the orthodontic practice. It causes aesthetic, functional, and psychological problems of varying intensities.4 Class II division 1 malocclusion may present with skeletal features of mandibular retrognathism, midface protrusion and dental features of distal step molar, an unusually large overjet and/or variable combination of these features5,6. However, the majority of Class II malocclusions can be attributed to mandibular retrognathia rather than maxillary prognathism.7
Tongue is one of the muscular structures of the craniofacial region whose position is affected by different types of malocclusion. Takahashi et al8 recorded the EMG activities of craniofacial temporalis muscle in 10 patients and found that the position of the tongue varies greatly in patients with different malocclusions. Class II malocclusion with mandibular deficiency results in decreased tongue space leading to curvature of the posterior aspect of the tongue.9
Severe mandibular deficiency has been linked to reduced space between the cervical column and the mandibular corpus that leads to a posteriorly postured tongue and soft palate10. This increases the chances of impaired respiratory function during the day and possibly causing nocturnal problems as well, such as snoring, upper airway resistance syndrome (UARS), and Obstructive sleep apnea syndrome (OSAS)10. Thus tongue position can contribute significantly towards increasing the future risk of Obstructive sleep apnoea (OSA) in Class II malocclusion patients with reduced tongue space.
There are various treatment modalities available to correct Class II malocclusions including use of headgear, elastics, removable myofunctional appliances, fixed appliances, dental extractions or distalization of maxillary teeth and orthognathic surgery. Awareness of mandibular deficiency as the main contributing part of the Class II structural etiology had led to the increased popularity of mandibular advancement appliances or the functional appliances.
In 1902‚ Pierre Robin11 was the first to use an intraoral appliance to bring the lower jaw forward in newborns with mandibular deficiency, thereby preventing posterior relocation of the tongue during sleep and the occurrence of oropharyngeal collapse. Today, this concept is widely used in dentofacial orthopaedics to stimulate mandibular growth and functional appliances form the main stay of treatment of skeletal Class II involving mandibular deficiency in growing children.11,12
The term functional appliance refers to a variety of orthodontic appliances designed to induce a change in activity of the various muscle groups that influence the function and the position of the mandible in order to transmit forces to the dentition and the basal bone13. Altering the sagittal and vertical mandibular position causes changes in muscular forces and result in orthopedic and orthodontic changes.14-16
Several types of functional appliances currently used for Class II treatment are aimed at improving skeletal imbalances, arch form, and orofacial function.13 During treatment with functional appliance in patients with Class II division 1 malocclusion, mandible is positioned in inferior and anterior position.14-16 Consequently, alterations in tongue position can be one of the effects of functional appliance therapy. 13
Lateral Cephalogram is one of the most commonly used 2-dimensional imaging method for evaluation of tongue position with proven reproducibility17. Also it is economical and non-invasive with low dose of radiation.
Though there are numerous studies in literature evaluating the skeletal and dental changes brought about by functional appliances, there are very few studies, to our knowledge, which assesses the changes in tongue position in response to functional appliances. Thus this study was carried out with the aim to evaluate the effects of functional treatment on the positional changes in tongue and to determine if any relationship exists between the functional appliance therapy in Class II division 1 and position of tongue.
MATERIALS AND METHOD
The study was conducted in the Department of Orthodontics and Dentofacial Orthopaedics, Sharad Pawar Dental College and Hospital, Sawangi, Wardha in co-ordination with Department of Oral Medicine and Radiology, AVBRH, Sawangi, Wardha. Total 30 cases, within the age group of 8-12 years, were selected from the OPD of Department of Orthodontics, SPDC. After getting informed consent, they were subjected to cephalometric evaluation and treated with functional appliance for an average of 8 months.
The following criteria were established for the sample:
- Patients with skeletal Class II malocclusion with a normal maxilla and functionally retruded mandible.
- Class II molar and Class II canine relation.
- Overjet equal to or greater than 4mm.
- ANB angle - Greater than 4.5 degrees
- Patient in active growth period, CVMI status – Stage 3 (transition) by Hassel and Farman vertebral index.
- Positive VTO on clinical evaluation.
Patients with class I and class III malocclusion and patients with Class II division 1 malocclusion due to involvement of maxillary component were excluded from the study.
Patients with moderate crowding and severe lower proclination in the dental arches, craniofacial syndromes or systemic disease or having any history of any orthodontic treatment were not included in the sample.
After the selection of cases, informed consent was obtained from each patient and pre-treatment lateral cephalogram of all the selected cases were taken. All the cephalograms were recorded with the same exposure parameters (kVp – 72, scan time of 1.2 sec) with the same magnification and the same machine (Planmeca, Finland) in the Department of Oral Medicine and Radiology, SPDC.
All the selected samples were treated with functional appliance. Patients were routinely monitored for regular wear of the appliance and after 8 months of appliance delivery, posttreatment lateral cephalogram of all the treated cases were taken and the changes in tongue position compared thoroughly.
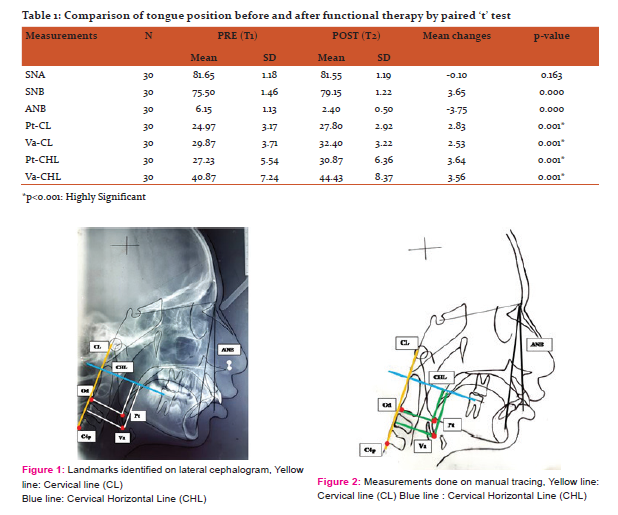
Various landmarks, reference planes and linear parameters used for the evaluation of the tongue position were based on methods described by Yassaei at al.9 Following points were traced in pre-treatment and post-treatment lateral cephalograms to determine positional changes of tongue. [Figures 1 and 2]
Cephalometric landmarks:
Od: The most posterior point of the odontoid process of the second cervical vertebrae
C4p: The most postero-inferior point on the 4th cervical vertebrae.
Pt: The most posterior point on the contour of the tongue.
Va (Valeculla): The deepest point of the valeculla.
Tb: Intersection point between the lower border of the mandible and contour
of the tongue.
Reference lines:
CL (cervical line): line connecting Od and C4p
CHL (cervical horizontal line): perpendicular line from Od to cervical line.
Tongue position:
Pt-CL: perpendicular distance from Pt to the cervical line. This variable indicates tongue position in horizontal plane.
Pt-CHL: perpendicular distance from Pt to the cervical horizontal line. This variable indicates tongue position in vertical plane.
Va-CL: perpendicular distance from valeculla to the cervical line. This variable indicates tongue position in horizontal plane.
Va-CHL: perpendicular distance from valeculla to the cervical horizontal line. This variable indicates tongue position in vertical plane.
Reliability:
All the lateral cephalograms were traced twice by hand onto acetate tracing paper. If the difference exceeded 1mm or 1 degree, third measurement was taken and the middle value of the two nearest measurements was used.
STATISTICAL ANALYSIS
A master file was created, and the data was statistically analyzed on a computer with Statistical Package for Social Sciences (version 11.5) (Chicago: SPSS Inc). The data was subjected to descriptive analysis for mean and standard deviation. Paired-t test was used to analyze the significance of differences in mean value before (T1) and after (T2) treatment. A value of p<0.05 is considered as significant.
RESULTS
The mean values, standard deviations of all cephalometric variables at pre and post-treatment are presented in Table 1.
When comparison was done between pre-treatment and post-treatment values, statistically significant differences were found in SNB angle (p= 0.00) and ANB angle (p= 0.00). No significant difference was seen in SNA angle (p = 0.163).
In horizontal plane, statistically significant differences were found when measuring distance of point Pt from CL plane, Pt-CL (p<0.001) and point Va from CL plane, Va-CL (p<0.001).
In vertical plane, statistically significant differences were found when measuring distance of point Pt from CHL plane, Pt-CHL (p<0.001) and point Va from CHL plane, Va-CHL (p<0.001).
There was a significant interrelationship between decrease of ANB angle and forward movement of tongue.
DISCUSSION
The growth of each compartment of the craniofacial system is integrated with that of others, and coordinated growth is required for normal development to occur18. Growth and function of the tongue, nasal cavities, the nasopharynx and the oropharynx are closely associated with the normal growth of the craniofacial complex18. As the root of the tongue is attached to mandible and hyoid bone, therefore the growth and spatial displacement of the adjoining skeletal components governs the position and size of the tongue.
The tongue has been an area of interest in orthodontics, with topics such as the relationships between different skeletal malocclusions and tongue position, function and posture and the clinician's potential to modify them. Retro-positioning of the tongue has been increasingly recognized as the most commonly found physiological characteristic in growing patients of Class II division 1 malocclusion with mandibular retrusion.
An unfavourable tongue position established early in life may predispose one to future sleep-disordered breathing, when subsequent soft tissue changes caused by age, obesity, or genetic background further reduce the available oropharyngeal airway19. Therefore, it can only be regarded as beneficial if functional appliance treatment in children results in improvement in tongue position10. Thus, the proper positioning of tongue will eliminate the possible effect of an impaired oropharyngeal airway function as an etiological factor for abnormalities in facial structures and might even modify the vertical and/or sagittal growth pattern of the craniofacial complex.
This study investigated the changes in tongue position in patients following treatment with functional appliances.
Tongue position in horizontal dimension: The results of this study indicate that following treatment with functional appliance, the tongue repositions significantly forward and these results are in accordance with the result of Zhou's study20. S Yassaei et al13 also found similar results in their study on 28 patients with Class II division 1 malocclusion in growing age.
The tongue moves forward with age. However, according to Ordoubazari21 who studied over 9-14, 18-30 age groups, he reported that forward reposition of tongue with age was minor. In this study, we found that there was a significant forward repositioning of tongue. This can be because of muscle attachments. Since the genioglossus muscle originates at the inner surface of the mandibular symphysis and inserts into the tongue, it acts as the main protruder of the tongue along with an accessory respiratory function, thus resulting in advancement of the base of the tongue and dilation of the upper airway22,23. Therefore it could be claimed that treatment with functional appliance leads to significantly forward alteration in tongue.
Also the decrease of ANB angle was significantly correlated with forward movement of tongue. There was significant correlation between forward movement of tongue with increase in size of oropharynx in sagittal dimension.
Thus we can say that treatment with functional appliance in Class II division 1 malocclusion improves the patency of airway, which in future, will result in decrease incidence of Obstructive sleep apnea.
In vertical dimension: According to the results of this study, following treatment with functional appliances, the position of the tongue moved significantly in a downward direction. This is in contrast to findings by S Yassei et al13 who found no significant downward movement of tongue following treatment with functional appliance.
Due to increase in vertical dimension during bite registration of functional appliance, the mandible moves downward due to molar extrusion, taking tongue along with it, thereby repositioning it in vertical direction.
CONCLUSIONS
Our results clearly suggest the existence of a relationship between functional orthopaedic treatment and improvement in tongue position in skeletal Class II growing subjects. In the results of this study, the tongue moved significantly forward in horizontal direction and downward in vertical direction. Corresponding with the decrease of ANB angle, there was a significant correlated forward movement of tongue. Thus treatment with functional appliance leads to significant alterations in tongue position.
This study helps in gaining knowledge about the effectiveness of functional appliances in altering the position of tongue during treatment of Class II division 1 malocclusion and also establishes the interdependence of Class II division 1 malocclusion and position of tongue.
Acknowledgement: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Source of Funding: Nil
Conflict of interest: Nil
References:
1. S Shishir. Timing of Myofunctional Appliance Therapy. J Clin Pediatr Dent 35(2): 233–240, 2010
2. Moss ML, and Salentijn. The primary role of functional matrices in facial growth. Am J Orthod, 55: 566–77, 1969.
3. Moss ML. The functional matrix hypothesis revisited 3: The genomic thesis. Am J Orthod Dentofacial Orthop 1997;112: 338–342.
4. Kharbanda OP. Orthodontics: Diagnosis and Management of Malocclusion and Dentofacial Deformities. 2 nd ed. New Delhi: Elsevier India; 2013. P. 4, 57, 459-519.
5. Hägg U, Pancherz H. Dentofacial orthopaedics in relation to chronological age, growth period and skeletal development. An analysis of 72 male patients with Class II division 1 malocclusion treated with the Herbst appliance. European Journal of Orthodontics. Aug 1988;10(3):169-76.
6. Moyers RE, Riolo ML, Guire KE, Wainright RL, Bookstein FL. Differential diagnosis of Class II malocclusions: Part 1. Facial types associated with Class II malocclusions. American Journal of Orthodontics. Nov 1980;78(5):477-94.
7. McNamara Jr JA. Components of Class II malocclusion in children 8–10 years of age. The Angle orthodontist. Jul 1981;51(3):177-202.
8.Takahashi S, Kuribayashi G, Ono T, Ishiwata Y, Kuroda T. Modulation of masticatory muscle activity by tongue position. Angle Orthod 2005;75:35-9.
9. Moss JP. The soft tissue environment of teeth and jaws. British J Orthod 7(3):127-137,1980.
10. Ozbek MM, Memikoglu UT, Gogen H, Lowe AA, Baspinar E. Oropharyngeal airway dimensions and functional-orthopedic treatment in skeletal Class II cases. Angle Orthod. 1998;68: 327–336.
11. Robin P. Glossoptosis due to atresia and hypotrophy of the mandible. Am J Dis Child 1934;48:541-7.
12. Anita G, Suma S. Growth modulation in Class II malocclusion - facts or delusion. Indian Journal of Dental Advancements 2010;1 (1): 20-23.
13. S Yassaei, Z Bahrololoomi, M Sorush. Changes of Tongue Position and Oropharynx Following Treatment with Functional Appliances. J Clin Pediatr Dent 31(4):287-290, 2007.
14. Bishara SE, Ziaja RR. Functional appliances: a review. 95:250-258,1998.
15. Patel HP, Moseley HC, Noar JH. Cephalometric determination of successful functional appliance therapy. Angle orthod. 72(5): 410-417 2002.
16. Kulbersh VP, Berger JL, et al. Treatment effects of the mandiular anterior repositioning appliance on patients with class II malocclusion Am J Orthod Dentofac Orthod. 123(3): 286-95, 2003.
17. Malkoc et al. Reproducibility of airway dimensions and tongue and hyoid positions on lateral cephalograms. Am J Orthod Dentofacial Orthop;128:513-6, 2005.
18. Preston CB, Lampasso JD, Tobias PV. Cephalometric evaluation and measurement of the upper airway. Seminar in Orthodontics 2004;10:3-15.
19. Martin SE, Mathur R, Marshall I, Douglas NJ. The effect of age, sex, obesity and posture on upper airway size. Eur Resp J. 1997;10:2087–2090
20. Zhou L, Zhao Z, Luo D:The analysis of the changes of tongue shape and position, hyoid position in class II, division I malocclusion treated with functional appliances (FR-I). Hua Xi Kou Qaaing,; 18(2):123-5. 2000
21. Ordoubazari M, Farokhnia F, Tuki Z, Ezzati F: Comparison of oropharyngeal space in 9-14 years and 18-30 year old Iranian groups. Dental journal of Shahid Beheshti Medical University, 19 (2):95-100, 1998
22. Yamaoka M, Furusawa K, Uematsu T, Okafuji N, Kayamoto D, Kurihara S. Relationship of the hyoid and posterior surface of the tongue in prognathism and micrognathia. J Oral Rehab; 30:914-920,2003.
23. Takahashi S, Ono T, Ishiwata Y, Kuroda T. Effect of changes in the breathing mode and body position on tongue pressure with respiratory-related oscillations. Am J Orthod Dentofac Orthop;115:239-44,1999.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License