IJCRR - 10(1), January, 2018
Pages: 27-30
Date of Publication: 10-Jan-2018
Print Article
Download XML Download PDF
Total Thyroidectomy for Large Goitres: Case series
Author: Nagarajan Raghupathy, Suresh K. Sinha
Category: Healthcare
Abstract:Aim: To present the experience of performing Total thyroidectomy for Large Multinodular goitres.
Case Report: Series of nine patients with large multinodular goitres treated in our institute between April 2016 and March 2017 were reported here. All of them underwent Total thyroidectomy. The clinical evaluation, intra operative management and complications
were analysed retrospectively.
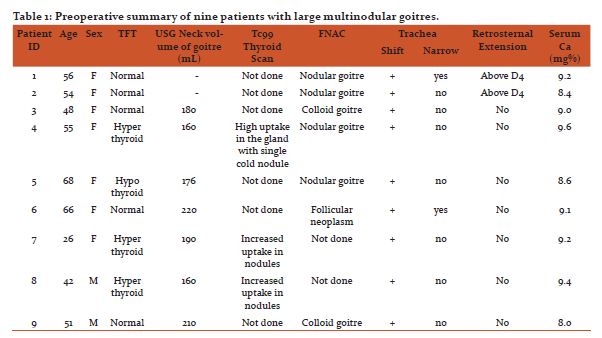
Discussion: In this series of nine patients,seven were Females and two were Males, age ranged from 26 to 68 years, seven of those patients had thyroid volume of more than 150 mL by neck ultrasonography and the other two had large goitres with retrosternal extension. Tracheal deviation was found in all nine patients and two patients had tracheal narrowing as well. Thyroid function test revealed three of the patients were hyperthyroid, one hypothyroid, and the rest euthyroid. Technetium(Tc99) scintigraphy showed cold nodule in only one patient out of the three hyperthyroid cases. Fine needle aspiration (FNAC) showed benign
pathology (Bethesda II) in six patients, one patient had follicular neoplasm (Bethesda IV). FNAC was not performed in two toxic goitres that did not have cold nodule. Total thyroidectomy was performed successfully in all nine patients.
Conclusion: Total Thyroidectomy can be safely performed even in large goitres; no incidence of tracheomalacia was observed; none had permanent hypoparathyroidism or recurrent laryngeal nerve injury.
Keywords: Large multinodular goitre, Total thyroidectomy, Tracheomalacia
DOI: 10.7324/IJCRR.2018.1017
Full Text:
Introduction
Benign multinodular goitres can be treated with thyroxine suppression therapy, radioactive iodine, or surgery (1). Total thyroidectomy for benign multinodular goitre circumvents reoperations and provides immediate relief from toxic symptoms inthe cases of hyperthyroidism(2). However, performing total thyroidectomy in large goitres is highly challenging due to the distorted anatomy.
Case Reports
Series of nine patients with large multinodular goitres treated in our institute between April 2016 and March 2017 were reported here, (seven Females and two Males), age ranged from 26 to 68 years. Clinical and ultra-sonographic examination of the neck was done in all nine patients. All of them had Grade 2goitreaccording to world health organization’s classification of goitres (3). Three patients were toxic without eye signs. Clinically lower border of the goitre was not palpable in two patients but Pemberton sign was negative.
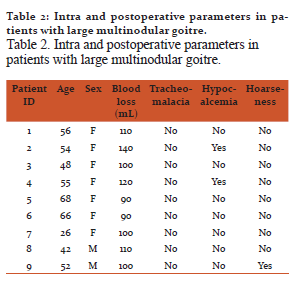
Ultrasonography of the neck performed with 7.5 MHz probe by the same radiologist. It did not reveal any features of malignancy in all nine patients. Maximum dimensions (length, width, and thickness) were measured for each lobe. Each lobe volume was calculated by using the formula: length× width×thickness×0.479 (4).Addition of both lobe volumes gave the total volume of the gland. Volume of the thyroid gland was greater than 150 mL in seven patients and the other two patients had retrosternal extension. Volume of the gland could not be accurately measured by ultrasonography in patients with retrosternal extension. So, MRI or CT scan should be used for that purpose(5). As the gland was massive, CT scan was done in all patients to study the position of trachea, oesophagus, vasculature, and retrosternal extension. CT scan of neck revealed tracheal shift in all nine patients and two of them had tracheal narrowing as well (Figure 1 and 2). CT scan of chest was done along with neck in two patients, which showed retrosternal extension of multinodular goitre. Lower border of the goitre reached above D4 level (Figure 1 and 2).
Figure 1. CT scan of neck (axil view) showing large multinodular goitre with tracheal shift to right.
Figure 2. CT scan of neck and mediastinum (coronal view) showing large goitre with tracheal shift to right, narrowing of tracheal lumen and retrosternal extension.
Thyroid function tests revealed three (33%) patients to be hyperthyroid, one hypothyroid, and the others(55.5%)to be euthyroid (Table 1). Technetium(Tc99) scintigraphy was done in three patients whose TSH were supressed. Those three patients had high uptake and only one patient had a single cold nodule. Fine needle aspiration (FNAC) showed benign pathology (Bethesda II) in six patients and one patient had follicular neoplasm (Bethesda IV). FNAC was not performed in two toxic goitres without cold nodule. Mean serum calcium level was 9.03mg% (range:8.4–9.6 mg%) (Table 1).
Table 1. Preoperative summary of nine patients with large multinodular goitres.
Management and operative procedure
Toxic multinodular goitre patients were given a course of Carbimazole to achieve euthyroid status before surgery. One hypothyroid patient was started on Thyroxine and was made euthyroid before surgery. Video laryngoscopy wasperformed in all patients and it showed mobile vocal cords in all nine patients. Risks and complications of total thyroidectomy were explained to the patients and informed consent was taken. Adequate blood was reserved before surgery.
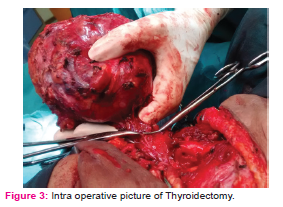
Fibreoptic scope was used for intubation. Nasogastric tube was put in all patients. It was useful in dissecting the mass without injuring the oesophagus. Skin incision was made from anterior border of one sternomastoid to the other and it was even longer in a two cases. Subplatysmal ?aps were raised and anterior jugular vein was ligated if required. Deep cervical fascia was opened in the midline. Both sternohyoid and sternothyroid were divided to get adequate exposure. Ligasure was used for dissection and vessel sealing. Middle thyroid vein was secured with energy device.Superior pedicle was dissected and ligated safely. Branches of inferior thyroid artery were coagulated and divided. All parathyroid glands were identified and preserved. In three patients, single parathyroid gland was auto transplanted in sternomastoid muscle due to injured vasculature(6). Recurrent laryngeal nerve was identi?ed in both sides in all patients and preserved. Ligasure minimised the blood loss (7,8)(Figure 3). Mean blood loss in our series was 106.6 mL. Retrosternal portion of goitres were gently dissected with finger while avoiding traction. Both retrosternal goitres were removed through cervical incision(9,10).Perfect haemostasis was secured. Tracheomalacia was ruled out and then the neck wound was closed with a suction drain. All nine patients were safely extubated at the end of surgery. Blood transfusion was not required in any case.
Figure 3. Intra operative picture of Thyroidectomy.
Postoperative complications
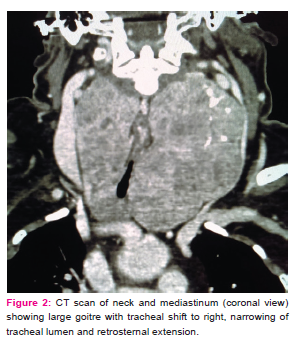
Transient hypoparathyroidism occurred in two out of nine cases (22.2%)and one patient had transient hoarseness (Table 2). Postoperative haematoma or infection did not happen in any of the cases. All of them discharged three days after the surgery. All nine specimens were benign by histopathology (Table 2).
Table 2. Intra and postoperative parameters in patients with large multinodular goitre.
Discussion
Multinodular goitre, enlarged to moderate to massive proportions, is very common, especially in patients hailing from rural India. Clinical, functional, ultrasonography with 7.5-10 MHz probe constitute the initial evaluation(1).CT scan is recommended in large goitres to assess the tracheal shift, adequacy of tracheal lumen, and retrosternal extension (11).Total thyroidectomy for benign multinodular goitre avoids reoperations and gives immediate relief from toxic symptoms in cases of hyperthyroidism. Complication rate is also low with meticulous dissection(2).
High dose radioiodine therapy has been triedin large goitres with volume more than 150 mL in both euthyroid and toxic thyroid patients. One third of goitre size reduction was achieved only after one year with high doses of I131 (26.7–124.9 mCi) therapy. Relief from toxic symptoms and compression werealso not immediate (5).
Intubation in massive goitres is a challenge to anaesthetist. Awake intubation was done using fibreoptic scopein allof our patients. Meticulous surgical techniquesare essential topreserve parathyroid and recurrent laryngeal nerve. Parathyroid gland has to be autotransplantedin cases of injury to its blood supply. Injured parathyroid gland has to be minced into thin slices and put into a pouch created in sternomastoid muscle. This measure circumventspermanent hypoparathyroidism (6). Ligasure energy device saves operating time and blood loss(7,8). Retrosternal goitres reaching above aortic arch (D4 level) can be removed through cervical route (9,10).
Long standing extrinsic compression over the trachea due to large goitres may soften the tracheal cartilages. It has been commonly suggested that after the removal of such large goitres, airway maycollapse in excess of 50% of diameter and warrant an emergency tracheostomy(12). After the removal of large goitre, tracheomalacia has to be ruled out. It can be done by the following steps; Oropharynx has to be cleared with suction. Endotracheal tube cuff needs to be de?ated. Tracheomalacia would cause tracheal collapse over the tube and prevent peri-tubal air leak. Therefore, the presenceof peri-tubal air leak after the cuff deflation rulesout Tracheomalacia (13). Trachea can also be palpated and the firm consistency of the tracheal cartilage excludes tracheomalacia. None of our patients developed tracheomalacia and all of them extubated safely at the end of surgery. No incidence of tracheomalacia was reported even in high risk patients with tracheal compression(14).However, it is safe to rule out tracheomalacia before closure.
Transient hypoparathyroidism occurred in two of our patients and one had transient hoarseness of voice. Our study included only nine cases but other studies with large number of cases also con?rmed that total thyroidectomy for large benign multinodular goitres is a safe surgical procedure(15,16,17).
Conclusion
Total thyroidectomy can be safely performed even for large multinodular goitres with minimal complications.
Acknowledgement
Authors acknowledge the immense help received from the scholars whose articles are cited and included in the references of this manuscript. The authors are also grateful to authors/ editors/ publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Source of funding: No funding received. Conflict of interest: Nil.

References:
- Samuels MH. Editorial: Evaluation and treatment of sporadic nontoxic goiter-some answers and more questions. The Journal of Clinical Endocrinology and Metabolism 2001; 86: 994-997.
- Liu Q Djuricin G Prinz R. Total thyroidectomy for benign thyroid disease.Surgery 1998; 123: 2-7.
- World Health Organization. Indicators for assessing iodine deficiency disorders and their control through salt iodization. WHO/NUT/94.6 1994; Geneva, Switzerland.
- Ple?niak J Urba?ski S. Comparative thyroid gland volume by two methods: ultrasonography and planar scintigraphy. Polish Journal of Radiology 2012; 77(2): 19–21.
- Bonnema, SJ Bertelsen H Mortensen J. The feasibility of high dose iodine I31 treatment as an alternative to surgery in patients with a very large goiter: effect on thyroid function and size and pulmonary function. Journal of Clinical Endocrinology and metabolism 1999; 84(10): 3636-41.
- Olson Jr JA DeBenedetti MK Baumann DS Wells Jr SA. Parathyroid auto transplantation during thyroidectomy: results of long-term follow-up. Annals of Surgery 1996; 223(5): 472–480.
- TestiniM PasculliA Di Meo G. Advanced vessel sealing devices in total thyroidectomy for substernal goitre: A retrospective cohort study. International Journal of surgery 2016; 35: 160-164.
- Luo Y Li X Dong J Sun W. A comparison of surgical outcomes and complications between hemostatic devices for thyroid surgery: a network meta analysis. European Archives Otorhinolaryngology 2017; 274(3): 1269-1278.
- Raffaelli M De Crea C Ronti S Bellantone R Lombardi CP. Substernal goiters: incidence, surgical approach, and complications in a tertiary care referral center. Head and Neck 2011;33:1420-5.
- HuinsCT Georgalas C Mehrzad H Tolley NS. A new classification system for retrosternal goiter based on a systematic review of its complications and management. International Journal of Surgery 2008; 6: 71-76.
- Cooper JC Nakielny R Talbot CH. The use of computed tomography in the evaluation of large multinodular goitres. Annals of Royal College of Surgeons 1991; 73(1): 32–35.
- Kandaswamy C Balasubramanian V. Review of adult tracheomalacia and its relationship with chronic obstructive pulmonary disease. Current Opinion in Pulmonary Medicine 2009; 15: 113-119.
- Sinha PK Dubey PK Singh S. Identifying Tracheomalacia. British Journal of Anaesthesia 2000; 84: 127-128.
- Findlay JM Sadler GP Bridge H Mihai R. xPost-thyroidectomy tracheomalacia: minimal risk despite significant tracheal compression. British Journal of Anaesthesia 2011; 106(6): 903-906.
- Hisham AN Azlina AF Aina EN Sarojah A. Total thyroidectomy: the procedure of choice for multinodular goiter. European Journal of Surgery 2001; 167(6): 403-405.
- Qiang LiuVassiliou I Tympa A Arkadopoulos N. Total thyroidectomy as the single surgical option for benign and malignant thyroid disease: a surgical challenge. Archives of Medical Science 2013; 9(1): 74-78.
- Search for articles by this authorTezelman SI Borucu I Senyurek GY Tunca F Terzioglu T. The change in surgical practice from subtotal to near-total or total thyroidectomy in the treatment of patients with benign multinodular goitre. World Journal of Surgery 2009; 33(3): 400-405.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License