IJCRR - 9(24), December, 2017
Pages: 40-42
Date of Publication: 26-Dec-2017
Print Article
Download XML Download PDF
Mediastinal Pancreatic Pseudocyst - A Rare Cause of Dysphagia (Case Report)
Author: Vipin Mathur, Rohit Kumar Jain
Category: Healthcare
Abstract:Pseudocyst is a common complication of both acute & chronic pancreatitis due to any cause. It is a localised fluid collection, rich in pancreatic enzymes surrounded by a wall of non- epithelialized fibrous tissue. Mostly it presents in and around the pancreatic tissue but on rare occasions it may extend into mediastinum causing symptoms due to compression & invasion of adjacent structures. We report a rare presentation of a young patient with dysphagia due to pancreatic pseudocyst extending into posterior mediastinum and compressing esophagus.
Approximately 50 cases of mediastinal extension of the pancreatic pseudocyst in the world literature are reported. Successful drainage of a mediastinal pseudocyst using a transesophageal approach under endoscopic ultrasound guidance has been reported. The literature was reviewed for clinical presentation, complications, and available treatment options for mediastinal pancreatic pseudocysts.
Keywords: Mediastinal, Pancreatic pseudocyst, Dysphagia, Transesophageal drainage
DOI: 10.7324/IJCRR.2017.9248
Full Text:
INTRODUCTION –
Pseudocysts are common complication of acute or chronic pancreatitis and pancreatic trauma. Most of them are located in and around pancreas but on rare occasions they can extend into mediastinum through anatomical openings in the diaphragm.
The mediastinal pseudocyst may present with symptoms like dysphagia, chest pain, dyspnoea, odynophagia, pseudoachalasia & cardiac tamponade.
CASE REPORT-
A 30 Years old male presented to us with complains of dysphagia of 3 months duration. Dysphagia was more to solids than liquids and nonprogressive. This young man had been consuming alcohol daily since last 8-10 years.
He was admitted 4-5 months earlier at a district hospital for severe pain abdomen, distention & vomiting. He was treated conservatively for 7-8 days and discharged in stable state. After 4-6 months of this episode he started feeling difficulty in swallowing.
His general physical examination, vitals signs and systemic examination did not reveal any significant abnormality. He was evaluated with basic lab investigations, gastroscopy and Contrast Enhanced-CT of abdomen.
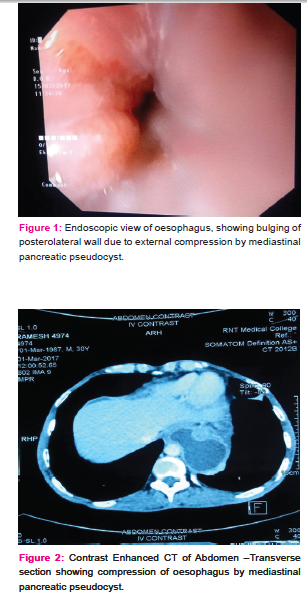
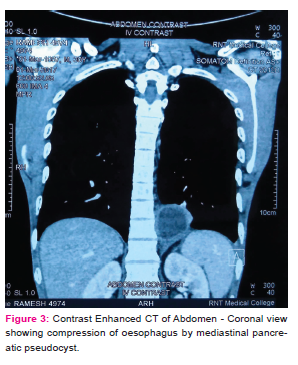
Gastroscopy revealed a smooth bulge in lower esophagus with normal overlying mucosa. Contrast Enhanced-CT Abdomen revealed changes of chronic pancreatitis with multiple pseudocysts. A large cyst in the tail of the pancreas was found extending into thoracic cavity through esophageal hiatus, compressing the lower esophagus and adjacent left lung parenchyma.
The patient showed slight improvement in dysphagia during admission and was allowed semi solid food. Endoscopic ultrasound guided transesophageal drainage was planned but patient refused the procedure for time being. So he was advised to eat soft diet and review after 3 months, as spontaneous resolution is rare in these cases.
DISCUSSION-
Mediastinal pseudocyst was first described in 1951(1) and it remains a rare complication of pancreatitis. In general mediastinal pseudocyst occurs due to rupture of pancreatic duct posteriorly into retroperitoneal space & tracking of fluid through esophageal and aortic hiatus, hence posterior mediastinum is the most common location(2). Extension through foramen of Morgagni is less common while mid mediastinal extension have also been reported through direct erosion of diaphragm.
Mediastinal pancreatic pseudocyst can cause complications due to invasion or compression of mediastinal structure or rupture into surrounding structures(3). Rupture into pleural space can cause pancreatic pleural effusion. Pressure into cardiac chambers could lead to CHF or rarely cardiac tamponade.
Approximately 50 cases of mediastinal pancreatic pseudocyst have been reported in world literature till date(4). Spontaneous regression of mediastinal pseudocyst is rare. Treatment options depend on severity of symptoms, size of pseudocyst, the ductal anatomy and local expertise. Complete resolution of mediastinal pseudocyst with Octreotide infusion have been reported by Yasuda & colleagues(5). However it may take long time.
Before 2000, surgical drainage or percutaneous drainage was chosen option but these modalities had a recurrence rate of 20% & a complication rate of 15%. With advancement of endoscopic technique, endoscopic drainage has become the standard of care.
Endoscopic internal drainage options include ERCP (Endoscopic retrograde cholangiopancreatography) with transpapillary duct drainage combined with endoscopic stent placement or transmural drainage. All endoscopic procedures for the treatment of pancreatic pseudocysts have recurrence of less than 5% and complication rate of 10%(6)
Endoscopic retrograde cholangiopancreatography with transpapillar stent placement can be used only when the mediastinal pseudocyst communicates with the pancreatic duct. Endoscopic ultrasound is increasingly used to guide transesophageal internal drainage of mediastinal pancreatic pseudocyst. It helps to identify wall thickness, site to be punctured in a nonbulging cyst as well as help avoid major vessels.
CONCLUSION-
Mediastinal pancreatic pseudocyst should be suspected in a patient presenting with atypical chest pain, dyspnea, or dysphagia, in the setting of a clinical history of pancreatitis. The timely and accurate diagnosis is important for this unusual and potentially life-threatening presentation of a common complication of pancreatitis. The finding of a thin-walled low-attenuation cystic mass in the posterior or middle mediastinum in continuity with pancreas seen into radiological imaging and history suggestive of pancreatitis are required for diagnosis. With the limited experience so far transmural drainage using transesophageal or transgastric approach under endoscopic ultrasound guidance appears to be a technically feasible, minimally invasive, and safe procedure for drainage of such mediastinal pancreatic pseudocyst. Physicians should be aware of atypical presentations and treatment options available for such mediastinal extension of a pseudocyst in a patient with a history of acute or chronic pancreatitis.
References:
- Topa L, Laszlo F, Sahin P, PoszarJ ; Endoscopic transgastric drainage of a pancreatic pseudocyst with mediastinal and cervical extensions : Gastrointestendosc 2006, 64 : 460-63
- Leung Mu, Grasser B, et al : Imaging of cystic masses of Mediastinum : Radiographics 2002
- Komtong S, et al : Mediastinal pseudocyst with pericardial effusion and dysphagia treated by endoscopic drainage : IOP 2006-7 , 105-10
- Rose EA ,Haider M, Yang SK. Medistinal extension of pancreatic pseudocyst. Am J. Gastroenterol, 2000 ; 95 : 3638-3639 [Pubmed]
- Yasuda et al : A case of pancreatic pleural effusion and Mediastinal pancreatic pseudocyst. Eur I Gastroenterol Hepatol2002:14 , 1279-82.
- BardiaA , Stokes N , Wilkinson NW : Mediastinal pancreatic pseudocyst with acute airway obstruction : J Gastroenterolsurg 2006 : 10, 146-50.
ACKNOWLEDGEMENT-
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
SOURCE OF FUNDING- NIL
CONFLICT OF INTEREST- None declared
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License