IJCRR - 9(24), December, 2017
Pages: 28-31
Date of Publication: 26-Dec-2017
Print Article
Download XML Download PDF
Spectrum of Clinical Presentation of Intracranial Tuberculoma
Author: Rohit Kumar Garg, Rattilal Meena, Neera Samar, Mayank Sharma, Sourav Shristi, Ankur Mittal
Category: Healthcare
Abstract:Objectives: To describe the clinical presentation, radiological findings in 15 patients with intracranial tuberculoma.
Design: Consecutive cases admitted with tuberculoma to the MBGH Hospital, Udaipur, Rajasthan, were included in the study. The diagnosis was based on clinical and neuro-imaging features.
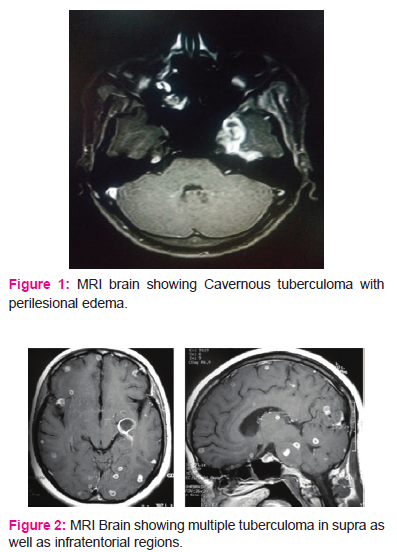
Results and Conclusions: The commonest presenting features were generalized convulsion(86.66%) and altered consciousness (80%). Computerised axial tomography/magnetic resonance imaging (CT/MRI) revealed single or multiple lesions that
showed intense contrast enhancement and perilesional edema. After receiving 6 months of ATT all patients were symptom free. We advocate early empirical trial of anti-tuberculosis drugs for intracranial tuberculoma even after a presumptive diagnosis.
Keywords: Anti-tuberculosis drugs, Intracranial tuberculoma
DOI: 10.7324/IJCRR.2017.9245
Full Text:
INTRODUCTION
Tuberculosis (TB), which is caused by bacteria the Mycobacterium tuberculosis complex, is one of the oldest disease known to affect humans and is a major cause of death worldwide. This disease most often affects the lungs, although other organs are involved in up to one-third of cases.1
Central nervous system (CNS) tuberculosis is a serious form of TB, due to haematogenous spread of Mycobacterium tuberculosis, manifest as meningitis, cerebritis and tuberculous abscesses or tuberculomas.2
Intracranial tuberculomas are the least common presentation of CNS TB, found in 1% of these patients.3They are multiple in 15%-33% of the cases.4
Tuberculomas often present with symptoms and signs of focal neurological deficit without evidence of systemic disease.5 Our study highlights the spectrum of clinical presentations of intracranial tuberculomas with the role of magnetic resonance imaging, a noninvasive tool, in prompt diagnosis and thereby early clinical management of such cases with a positive outcome.
Study design
A retrospective cross sectional study was done in 15 patients in whom neuroimaging shows ring enhancing lesion and was suspected as tuberculoma lesion.
Material and methods
This study was done retrospectively by analyzing patients presenting with tubercular infection of the CNS in the form of tuberculoma under the author in last one and half years (July 2015-dec. 2016) in medicine department.
Inclusion criteria
- Only adult patients (more than 16 year of age) were included
- All patients with ring enhancing lesions on neuroimaging who were suspected as tuberculoma analyzed in the view of their clinical presentation.
Exclusion criteria
Methods
A detailed clinical history was noted as described in the study Performa in all patients in which neuroimaging study was suggestive of tuberculoma lesion. A detailed past, family and personal history was taken in all patients. A thorough general and systemic examination was done.
Laboratory tests done included a complete blood count with erythrocyte sedimentation rate(ESR), electrolytes and routine biochemical tests. Specific laboratory tests for establishing etiology were performed like screening for HIV-1 and 2, blood cultures, sputum microscopy and culture. Cerebrospinal fluid analysis for protein, sugar, cell count and morphology, Cerebrospinal fluid ADA, IgM toxoplasma antibodies, cryptococcal antigen were done when indicated. Imaging studies done included computed tomography (CT) brain or magnetic resonance imaging (MRI) brain with contrast as was indicated. Ancilliary investigation like X-ray chest and USG abdomen was done whenever the clinical situation demanded.
Results
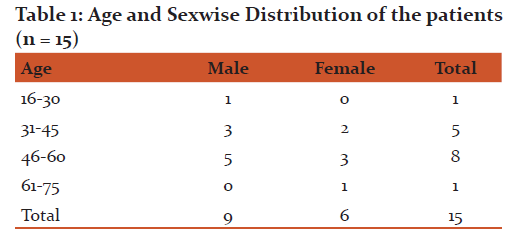
Fifteen indoor patients admitted to medical ward satisfying the inclusion criteria were selected for the study, all of them from rural area near Udaipur. Table 1 showing the age and sex wise distribution of the patients. The age group of patients were ranged from 16-75 years. Majority of patients were in the age group of 46-60years. Out of 15 patients in the study group,9 patients were male (60%) and 6 were female (40%). The overall sex ratio was 1.5:1. All patients were laborers by occupation and nonvegeterian.
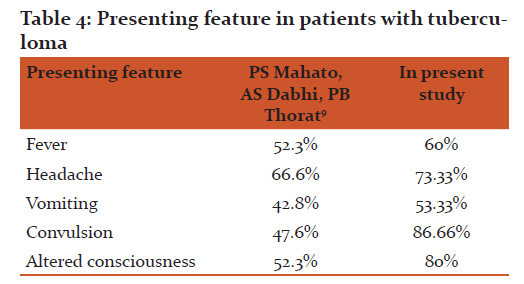
Clinical features of are summarized in Table 2.Seizure was the most common presenting feature. 13 patients (86.66%) out of 15 were presented with one or more episodes of seizure. The type of seizure was generalized tonic and clonic in all of them. History of altered consciousness was also present in 12 patients (80%). 11 patients (73.33%) were having complaint of headache.8 patients (53.33%) out of 11 who were having headache also have associated vomiting. History of fever was present in 9 patients (60%).

Past History
There was no previous history of pulmonary or extrapulmonary TB in any patient and none of them was diabetic.
Examination
11 patients (73.33%) had pallor. There was no lymphadenopathy, icterus, pedal edema or clubbing.
On CNS examination 2 patients were having cranial nerve palsy but none of patient have papiloedema. Neck stiffness was present in 1 patient.
Investigations
Mean hemoglobin was 9.6 g/dl and ESR 68 mm at end of first hour. None of patient was HIV positive. chest x-ray was done in all the patients and there was no any patch except in one patient, in which it was showing milliary shadows in bilateral lung fields. Cerebrospinal fluid analysis for protein, sugar, cell count and morphology shows no abnormality in any of the patient. Cerebrospinal fluid ADA, IgM toxoplasmosis antibodies, cryptococcal antigen were negative.
MRI brain was done in all the patients which was showing tuberculoma lesion in all the patients at different locations.
DIAGNOSIS AND TREATMENT
Probable etiological diagnoses were based on the presence of supportive findings detected after clinical evaluation and above mentioned battery of investigations. The diagnosis remained probable be cause in none of the patients histopathological verification was obtained. Patients were provided appropriate symptomatic treatment (corticosteroids, mannitol, antiepileptic drugs and/or analgesics if required). Appropriate specific treatment according to the diagnosis was given. Some of above mentioned laboratory investigations were periodically repeated during hospitalization and on outdoor follow-up to monitor the disease activity on modifying the ongoing treatment.
DISCUSSION
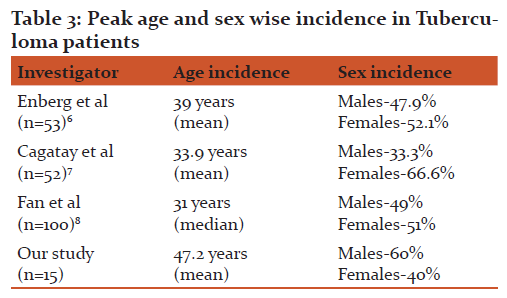
The mean age of patients was 47.2 years with 53.33% of patients between 46-60 years of age. The mean age obtained in various studies is as shown in Table 3which is in accordance with our observation. Males predominated in all age groups. The sex wise incidence in various other studies is as shown in Table 3.
In our study Seizure was the most common presenting feature which was present in 13 patients (86.66%), loss of consciousness in 12 patients (80%),headache in 11 patients (73.33%),vomiting in 8 patients (53.33%) and fever was present in 9 patients (60%). Table 4 shows comparison of presenting clinical feature of previous studies and our study.
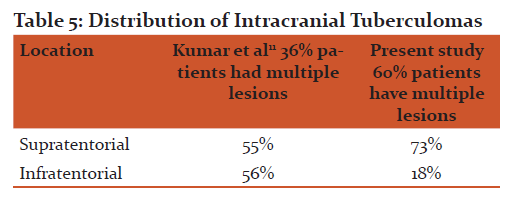
None of the patient was having history of tuberculosis. Chest X-ray shows milliary TB in only one patient. On neuroimaging, 60% shows multiple ring enhancing lesions. We use following criteria to differentiate tuberculoma from other causes of ring enhancing lesion in MRI10:-
- ring enhancing lesion in neurocysticercosis usually shows multiple lesions in different stages of evolution.
- ring enhancing lesions in abscesses are restrict on DWI.
- ring enhancing lesions in neoplasm shows elevated choline peak on MRS.
The distribution of these lesions compared with other studies is shown in Table 5.
CONCLUSION
Brain tuberculoma is one of the neurological manifestation of tuberculosis, usually occur in immunocompromised individuals due to haematogenous spread from a primary focus, mainly from the lungs. In this study we studied 15 patients, all of them immunocompetent and none of them was having past history of tuberculosis. Only 1 out of 15 patients had chest x-ray suggestive of milliary tuberculosis.
We emphasize here that tuberculoma can be occur in immunocompetent patients without past history of TB and without any active lesion in lungs. In past various studies have been done on tuberculoma but only few of them was suggesting tuberculoma without any immunocompromised status and without any active lung lesion. So we should suspect brain tuberculosis in patients presenting with above mentioned clinical features despite good immune status, without any active lung lesion or negative tubercular history of patient.
References:
1. Mario C. Raviglione chapter 202 page no.1102 Harrison 19th edition.
2. Rock RB, Olin M, Baker CA, Molitor TW, Peterson PK. Central nervous system tuberculosis: pathogenesis and clinical aspects. Clinical Microbiology Reviews2008;21(2):243e61.
3. Pimentel MLV, Alves SMV, Novis SAP, Brandão RZ, Neto EB. Intracranial tuberculomas developing during treatment of pulmonary tuberculosis: casereport. Arq Neuropsiquiatri 2000;58(2-B):572e7.
4. Hejazi N, Hassler W. Multiple intracranial tuberculomas with atypical responseto tuberculostatic chemotherapy: literature review and a case report. Infection1997;25(4):41e6.
5. Sahaiu-Srivastava S, Jones B. Brainstem tuberculoma in the immunocompetent: Case report and literature review. Clinical Neurology and Neurosurgery2008;110:302e4.
6. Enberg GM, Quezada B Mde L, de Toro VC, Fuenzalida LL. Tuberculous meningitis in adults: review of 53 cases. Rev Chilena Infectol 2006;23(2):134-9.
7. Cagatay AA, Ozsut H, Gulec L, Kucukoglu S, Berk H,Ince N, et al. Tuberculous meningitis in adults – experience from Turkey. Int J Clin Pract 2004;58(5):469-73.
8. Fan HW, Wang HY, Wang HL, Ma XJ, Liu ZY, Sheng RY.Tuberculous meningitis in Chinese adults: a report of 100cases. Zhonghua Nei KeZaZhi 2007;46(1):48-51.
9. Mahato PS, Dabhi AS, Thorat PB. Clinical and Investigative Profile of Ring-enhancing Lesions on Neuroimaging.
10. Osborn AG. Osborn's Brain: Imaging, Pathology and Anatomy. In: Tuberculosis Fungal, Parasitic and Other Infections, P.341.
11. Kumar N, Narayanaswamy AS, Singh KK. Ring enhancing CT lesions - a diagnostic dilemma. J Assoc Physicians India 1995;43(6):391-3.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License