IJCRR - 4(15), August, 2012
Pages: 37-42
Date of Publication: 15-Aug-2012
Print Article
Download XML Download PDF
UTERINE RUPTURE: 5 YEAR STUDY IN A TERTIARY CARE HOSPITAL OF WESTERN RAJASTHAN, INDIA
Author: Savitri Sharma, Ashok Sharma, Annapurna Mathur, MadhuSudan Swarnkar, D. S.Khangarot
Category: Healthcare
Abstract:Objective: To determine the frequency, predisposing, factors, maternal and fetal outcome in Uterine Rupture. Methods: This is a descriptive case series including all cases of uterine rupture who were either admitted with this complication or who developed it in the hospital were included in the study .Patients, who had rupture due to congenital abnormality were excluded from this study .Demographic data ,details of predisposing factors ,types of rupture ,the management ,maternal and fetal outcome were taken into consideration for analysis. Results: The total numbers of deliveries from Jan 2007 to Jan 2012 were28076.There were 22 cases of uterine rupture .Out of them most of the cases (55%) presented between age of 21 to 25 years. Majority of cases (54.54%) of uterine rupture occurred in 1 Para. All the cases were unbooked All cases had complete tear of anterior, lower part of uterus. Common cause (54.54%) of uterine rupture was previous caesarean section, second common because (22.72%) was prolonged obstructed labour .Sub total hysterectomy was performed in45 % cases and only repair was the management in remaining 55% cases. There was no maternal death in this study .live birth rate was 41%. There was still birth in 11(50%) and intra uterine death occurred 2(9%).3 cases had associated bladder injury with uterine rupture. Conclusion: This study showed that main cause of uterine rupture was previous caesarean section, followed by prolonged obstructed labour. Proper antenatal care and update training programme for health care providers is the need of time to prevent the catastrophic but avoidable complications.
Keywords: Uterine rupture, Caesarean section, Maternal and fetal outcome.
Full Text:
INTRODUCTION
Rupture of the gravid uterus is a grave obstetric complication. It is associated with high maternal and prenatal mortality rates. Even where the patient survives, their reproductive function is abruptly terminated, and recovery is often prolonged and turbulent1,2.Uterine rupture related with some instant hitches, such as shock, anaemia and a rupture of urinary bladder, may leave surviving patients with term complications like vesicovaginal fistula and inability to deliver children3 . The prevalence was found significantly high in underdeveloped countries of Asia and Africa in comparison to high income countries 4,5 . The incidence of uterine rupture has dropped significantly in developed countries and is most often encountered while attempting vaginal birth after caesarean section.6 The risk of experiencing uterine rupture during child birth is 50 times higher if the mother already had a caesarean
section.6 Most cases of uterine rupture that occur in developing countries are due to ignorance, quackery, and maladministration or nonavailability of essential medical supplies. Causes of uterine rupture are: grand multiparity, injudicious use of oxytocin particularly when it is not medically indicated and administered, neglected labour, previous caesarean section and myomectomy, uterine instrumentation and manipulation, labour induction, congenital abnormalities of uterus and uterine distension due to polyhydroamnios, multiple pregnancy and foetal macrosomia. The sign and symptoms of uterine rupture largely depend on timing, site and extent of uterine defect, severe haemorrhage, palpable fetal parts, recession of presenting foetal parts, loss of uterine contractility, rarely blood stained urine, appearance of placenta at vulva and prolapsed loops of gut into vagina.7. Hysterectomy is considered the treatment of choice in patients with intractable haemorrhage or when uterine rupture sites are multiple. Repair of ruptured uterus with or without tubal ligation is done in young and stable patient. Repeat caesarean section is done at 36 weeks of gestation in patients with previous uterine repair 8,9 . This study was done with the view that there is paucity of studies related to uterine rupture in Rajasthan even in India.
MATERIAL AND METHOD
This is retrospective hospital based observational study and it was conducted from January 2007 to Jan 2012 at Heera kunwar Ba zanana Hospital Jhalawar which is a tertiary care hospital of Jhalawar Medical College and having 500 bed capacity in General including 150 beds in Zanana hospital. Two units are regularly being run in this institution in Obstetrics and Gynae department. The data collected from the maternity ward and operation theatre registers as well as from the patient‘s case file at the Hospital Medical Record office. 22 cases of uterine rupture were recorded in this period. Various parameters studied were age, parity, distance travelled by patients, maternal and fetal outcome, operative procedure done, blood transfusion and study of immediate complications. History of Previous caesarean section, other uterine surgery, and causes of prolonged labour were recorded. Management was done in the form of sub total hysterectomy, repair of ruptured uterus or bladder with or without tubal ligation. Maternal outcome in the form of recovery, death, also perinatal deaths were recorded and data analyzed. Most cases were referred from periphery and a few suffered uterine rupture in the hospital. Delay in starting definite treatment was found due to long distances travelled by patients from her place to the hospital.
RESULTS
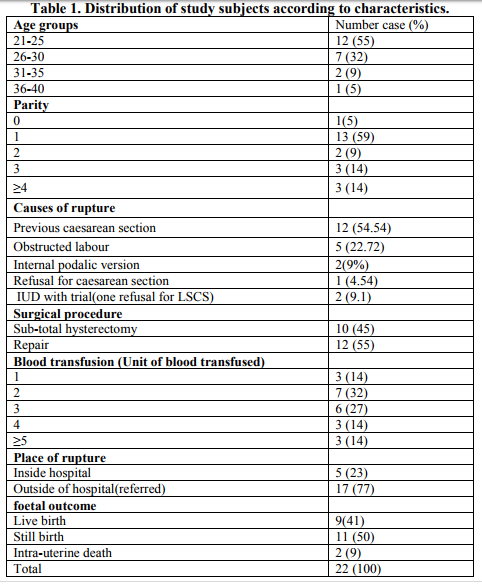
From January 2007 to January 2012, 28076 deliveries conducted and 22 cases of uterine rupture were recorded. The overall incidence rate found 0.0783% or 1 in 1276 deliveries. The age of patients varied between 20 years to 40 years. The highest incidence(55%) of rupture seen in the age group of 21-25 years and 7cases (32%) from 26-30 years, 2 cases(9%) belonged to age group 31-35 years while lowest incidence was observed in 36 - 40 years. In 12(54.45) cases making majority, cause of rupture was previous caesarean section scar ,while second cause noted was obstructed labour 5(9%) ,third important cause came out as manipulation( internal podalic version) in 2 cases. One case refused for caesarean section and was given trial resulted in rupture uterus. Also there were two cases with IUD in which trial was given and uterine rupture occurred. Most of the patients (77%) travelled more then 30 to 45 Kilometers from periphery to hospital and had ruptured uterus at home or with traditional birth attendants or at the level of primary health centre while remaining patients (23%) suffered rupture uterus during management in hospital.
In this study it was observed that highest(59%) cases of rupture occurred in women having one parity, 2 cases (9%) were seen in 2 parity females, 3 cases(14%) of rupture occurred in 3 para ladies while only 3 (14%)cases were seen in 4 or more than 4 para. One case of rupture was seen in nuliparous woman. An analysis regarding fetal outcome revealed that in 41% (9 cases)females delivered live babies, while in 50% (11 cases) there was still birth delivery, 2 cases(9%) suffered from intra uterine death. Regarding maternal mortality no death was seen during management because of rupture uterus. Surgical management was the only choice for saving life of mothers. 10 cases (45%) were managed by subtotal hysterectomy, while a quite good number of cases 12(55%) were treated by repairing uterus for preserving reproductive function. A single case was managed by repair with tubal ligation.
DISCUSSION
Uterine Rupture is one of most dangerous obstetric situation carrying an increased risk of maternal and perinatal morbidity and mortality, which is associated with poorly managed labour10, 11 . The incidence of ruptured uterus (1:1276 deliveries) in this series is lower than 1:167 and 1:110 reported earlier in Nigeria 12 and Ethiopia 13 , respectively, but higher than 1:6331 deliveries reported by chen et al from Singapore 14 . 77% cases were reached this institute either from home directly or from peripheral health institutions. This reflects that these patients try to deliver at home by traditional birth attendants or at remote health centers by health service providers. The majority of patients in this series did receive care neither in antenatal period and/or nor in intrapartum period at primary health care centers. In spite of recognizable risk factors present in almost all of them in the antenatal period, they continued to be dependent either on traditional birth attendants or they remain quite unattended and proceeded to labour. All had prolonged labour and yet this was either not recognized or recognized and managed erroneously by the administration of enormous doses of oxytocin intramuscular which was noticed as a trend adopted by traditional birth attendants and even by trained ANMs (Auxiliary Nurse Midwife) in this area. As 12 cases of uterine rupture had history of previous LSCS cases. If these cases could have been attended at community health centre level equipped with blood bank and if Gynaecologist or Surgeons have attended it there it self providing surgical facility number of still born/IUDs could have been less. In 5 cases (22.72%) prolonged and obstructed labour was the cause for uterine rupture due to injudicious use of oxytocin and delay in transport of patients to tertiary care centre. The injudicious use of oxytocin was found to be a significant predisposing factor in this series unlike reports by Konje et al 12 but similar to reports by chen et al 14, Chen and Hsieh 15 . Majority (54.54%) of patients in this study had a rupture of scarred uterus, similar to a report from Singapore by chen et al 13 in which over two-third of cases occurred in women with scarred uterus.In a retrospective review of 93 cases,P.Veena et al found that maximum number of uterine rupture occurred in younger age group (20-30 years) and 77% cases in her series had previous caesarean section depicting strong association of uterine rupture with previous scarred uterus .These observations match with our study 16 . In our study 2 cases of previous LSCS had uterine rupture during trial for vaginal delivery. In these two case one patient refused for LSCS and in another trial was given under supervision both suffered uterine rupture. In 2 cases internal podalic version for vaginal delivery was the cause for uterine rupture. This calls for caution, especially when some of these patients were subjected to induction or augmentation of labour 14,2. In a trial of labour in patients with scarred uterus, It is important that health workers supervise the labour closely and exercise caution before considering augmentation of the labour 2 . Refusal for LSCS in 1 case with one previous LSCS and other multi gravid with cephalo pelvic disproportion shows that in Indian society still there is big craze for vaginal delivery even when patient was in high risk, constituting cause for uterine rupture. Most patients (45%) had sub total hysterectomy done while 55% had repaired (bilateral tubal ligation in one case). Therefore 45% of patients lost their reproductive and /or menstrual function. The rest could have reproductive and or/ menstrual function maintained. They could only reproduce at risk. Ruptured uterus therefore has grave sociocultural implications, especially in a society where these functions are considered the very essence of womanhood.
In our study there was no maternal mortality, all women with uterine rupture recovered fully and discharged which was due to the fact that they were timely attended and treated as soon as they reached hospital. Also This could happen because of good support from blood bank as in majority of cases 3 or more than 3 units of blood was transfused with no delay. One more reason for better survival in this study appears to be related with the incidence of uterine rupture in younger age group i.e. 21 to30 years (total 87%) who sustained haemorrhagic shock and surgical trauma efficiently. In this study live birth rate was 41% which was higher than that seen in other study (31%) 16 .But a number of still birth 50% is quite worrying in this study which calls for attention.
CONCLUSION
Ruptures uterus is only one of the many preventable obstetric problems with grave consequences. Ruptured uterus remains a problem in our set up, with primary health centers and deliveries by traditional birth attendant being identified as major contributors to this condition. They primarily fail in the reorganization of abnormalities in the antepartum and /or intrapartum periods, with delays in referral and injudicious use of oxytocin. We recommend prohibition of the unsafe prescription of oxytocin. This is presently an over -the -counter drug and has been shown in this study, a dangerous drug in the hands of the unskilled. Health education of women in the reproductive age is also required. We recommend utilizing pyramidal health structure that is primary health centers would be directly responsible to secondary health centers, which in turn would be directly responsible to tertiary health centers. Also there is need that referral health centers at subdivision, tehsil levels need to be well equipped with blood banks and availability of operating surgeon/gynaecologist so patient in such a grave situation may not have to rush for more then 35 Km distance to avail facility at district level/tertiary level centers as happened with them in this series of study, because it puts detrimental effects on maternal as well as foetal outcome in this rural population dominated country.
References:
1. Elkady AA Bayomy HM. Bekhiet MT. Najib HS. Waliba AK. A review of 126 cases of ruptured gravid uterus.Int Surg 1993:78:231- 5.
2. Prasad RN, Rantan SS. Uterine rupture after induction of labour for intrauterine death using the prostaglandin E2 analogue sulprostone Aus N Z J Obstet Gynaecol 1992:32:282-3.
3. Philpott RH- obstructed labour. Clin obstet Gynaecol 1982; 625-40.
4. Saglamtas M, Vicdan K, Yalcin H,et al.- Rupture of the uterus.Int J Gynaecol Obstet 1995;49:9-15.
5. Lema VM, Ojwang SB, Wanajala SHRupture of the gravid uterus: a review: East Afr Med J 1991;68:430-41
6. Rashmi, Kirshan, Vaid NB – Rupture uterus changing Indian scenario. J Indian Med Assoc 2001; 99:634-7.
7. Khanum Z, Lodhis K-emergency Obstetric Hysterectomy;a lifesaving procedure.Ann King Edvard Medical College 2004; 10:292- 4
8. Bashir A-maternal Mortality in Faisalabad city-A longitudinal study.The Gynaecologist 1993; 3:14-20
9. Lim AC,Kwee A ,Bruinse HW-Pregnancy after uterine rupture:A report of 5 cases and review of theliterature,Obstet Gynaecol Surv 2005;90;16-37
10. Kwast BE, Liff JM-Factors associated with maternal mortality in Addis Ababa, Ethiopia .Int J Epidemiol 1988; 17:115-21
11. Kadowa I- Ruptured uterus in rural Uganda;prevalence,predisposing factors and outcomes.Singapore Med J 2010;51:35-38.
12. Konje JC Odukya OA. Ladipo OA. Ruptured uterus in Ibadan- A twelve-year review Int J Gynecol Obstet 1990:32:207-13.
13. Gessessew A, Melese M. Ruptred uterus – eight year restrospective analysis of causes and management outcome in Adigrat Hospital.Tigray region. Ethiop J Health Dev 2002:16-241-5.
14. Chen LH, Tan KH. Yeo GS. A ten years review of uterine rupture in modern obstetric practice. Anm Acad Med J Singapore 1995:24:830-5.
15. Chen KC, Hsieh TT. Rupture of grand uterus: an eight-year clinical analysis and review of literature .Chang Keng I Hsueh- Chang Keng I Hsueh-Chang Gung Med J 1992; 15:15-22.
16. P.Veena, S Habeebullah, and L.ChaturvedulaA review of 93 cases of ruptured uterus over a period of 2 years in a Tertiary Care Hospital in South India; April 2012: Vol 32- No 3; pages 260-263
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License