IJCRR - 9(22), November, 2017
Pages: 22-25
Print Article
Download XML Download PDF
Juvenile Psammomatoid Ossifying Fibroma - A Rare Entity
Author: Evelyn Elizabeth Ebenezer, Volga Harikrishnan, Chitra Srinivasan
Category: Healthcare
Abstract:Aim: Juvenile ossifying fibroma (JOF) is a rare fibro-osseous neoplasm in young children.
Case Report: 14 year old boy presented with a painless swelling over the palatal region for two months duration which was clinically diagnosed as pyogenic granuloma.
Discussion: JOF is defined as a variant of the ossifying fibroma, and latter includes juvenile psammomatoid ossifying fibroma (JPOF) and juvenile trabecular ossifying fibroma (JTOF). Both variants involve the craniofacial bones with the trabecular variant being more common in the jaws and the psammomatoid variant being more common in the paranasal sinuses. JPOF may exhibit erosion and invasion of the surrounding bone accompanied by rapid enlargement. JPOF can be distinguished from other maxillofacial fibro osseous lesions by its tendency to recur and its clinical mimicry of malignant bone tumors.
Keywords: Ossifying fibroma, Psammomatoid ossifying fibroma
DOI: 10.7324/IJCRR.2017.9225
Full Text:
INTRODUCTION
Fibro-osseous lesions are a group of diseases characterized by replacement of normal bone tissue by fibroblast, fibrous tissue, and variable quantities of mineralized material.[1]
Fibro-osseous lesions do not represent a specific diagnosis represent a group of disease such as: (1) Fibrous dysplasia, (2) osseous dysplasia and (3) ossifying fibroma[1].Thou they have similar clinical, radiographic and histopathological features but present different in biological behavior. Ossifying fibroma is a neoplasm while Fibrous dysplasia and osseous dysplasia are reactive lesions.[1]
Ossifying fibroma has been referred to as fibro osteomas, osteofibroma benign fibro-osseous lesion. Ossifying fibroma was first described by Menzel in 1872, but the term was coined in 1972 by Montgomery
Ossifying fibromas are classified into two groups based on the clinicopathological presentation as Conventional and juvenile. Conventional ossifying fibromas are usually present in the third and fourth decade of life and present as a slow growing mass. They can be treated with simple curettage and the recurrence is rare, but in contrast to the form seen at adults, the juvenile ossifying fibroma(JOF) occurs in much younger age and presents as a more aggressive mass with increased recurrence rate.[2]
JOF is further subdivided into two distinct histopathologic variants of as Trabecular juvenile ossifying fibroma (TrJOF) and Psammomatoid Juvenile ossifying fibroma (PsJOF).
The Psammomatoid variant was first reported in the year 1938 by Benjamin’s, who described it as osteoid fibroma with atypical ossification of the frontal sinus. Later, in 1949 Gögl, termed it as psammomatoid ossifying fibroma of the paranasal sinuses and nose. In 1952 Johnson et al further modified the term as juvenile active ossifying fibroma. Following a review of 86 cases by Makek, it was considered to be a variant of osteoblastoma and was termed as psammous desmo osteoblastoma.It was in the year 1985, Margo et al introduced the term psammomatoid juvenile ossifying fibroma.[2]
Other names that have also been considered are psammo osteoid fibroma, psammous desmo osteoblastoma, juvenile psammomatoid ossifying fibroma, and juvenile aggressive psammomatoid ossifying fibroma. [2]
The distinctive features of PsJOF are a predilection for the sinonasal complex and orbit of young people, with an aggressive, infiltrative growth pattern, and a high incidence of recurrence.[2]
Here we report a case of Juvenile ossifying fibroma involving the maxilla in a 14 year old boy.
CASE HISTORY
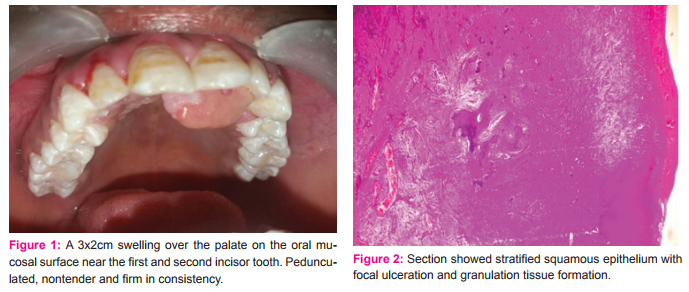
A 14 year old boy presented to the OPD of oral and maxilla facial surgery at Saveetha Medical College and Hospital, Chennai, India with complaints of a painless swelling over the palatal region for two months duration gradually progressive in size. No history of trauma or similar lesion noted. Other Medical and Dental history were not contributory .General physical examination revealed no abnormalities. Extraoral examination revealed mild facial asymmetry. On intraoral examination the swelling was 3x2cm over the palate on the oral mucosal surface near the first and second incisor tooth. It was pedunculated, nontender and firm in consistency (fig 1).The mouth opening of the patient was normal and there were no decayed teeth in the lesion are. Oral hygiene was good. With the above clinical features a Differential diagnosis of Traumatic fibroma or pyogenic granuloma was considered. Complete surgical removal of
The lesion (enucleation) was carried out under local anesthesia with conscious sedation. Post-operative course was favorable. The excised tissue was sent in 10% Neutral buffered formalin and subjected to histopathological evaluation.
MORPHOLOGY
Gross Examination: Received specimen measured 2.5 x1 cms, well defined, pale brown and firm in consistency, External surface was smooth. Cut surface was uniform pale brown. The tissue was all embedded and processed for microscopic examination.
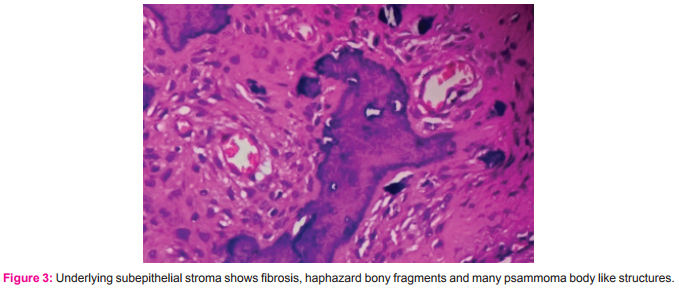
Microscopy: Hematoxylin and eosin stained slides were examined under light microscopy. Sections showed stratified squamous epithelium with focal ulceration and granulation tissue formation.(Fig 2).with underlying sub epithelial stroma shows fibrosis, haphazard bony fragments and many psammoma body like structures (Fig3).With the above features a Confirmatory diagnosis of Juvenile psammomatois ossifying fibroma was given.
DISCUSSION
Ossifying fibroma is a rare benign osteogenic neoplasm. It comprises of 2% of oral tumors in children. This rare neoplasm can present as a clinical enigma and a pathological dilemma, due to its overlapping clinical and morphological features. There are persistent differences in terms of classification and diagnosis of fibro-osseous lesions in craniofacial area, a dilemma does exist amidst these lesions. All present as a replacement of normal bone tissue with fibroblast and collagen fiber tissue along with varying quantities of mineralized material.[3]
JOF has a slight male predominance. [3] The average age of occurrence for trabecular JOF is 8 1/2 to 12 years, while the psammomatoid variant occurs during 16-33 years. Our patient was 14 years old. 75% of PsJOFs predominantly occur in the orbit, paranasal sinuses and calvaria, and 25% involve the maxilla or mandible, as in our case. The TrJOF predominantly involve the jaws, with a predilection for the maxilla.[4]
Although the underlying cause is unclear, there are been few articles reporting trauma as a causative factor in areas of the lesion. Postulating a connective tissue reaction rather than a neoplasm.
Suggested hypothesis include:
According to Kempsoh[5] — bone deposition and resorption occurring on the same spicules of the bone. It was postulated that ossifying fibroma resulted from excessive resorption of bone with fibrous repair of the defect.
• Hammer suggested ossifying fibroma — considered as tumor of periodontal ligament origin (mesenchymal blast cells).[6]
• Trauma induced stimulation of progenitor cells has been suggested by Weing.[3]
It also occurs in the jaws due to maldevelopment of basal generative mechanism that is essential for root formation.[7]Ossifying fibroma are sporadic , but incidence of familial inheritance by the presence of nonrandom chromosomal breakpoints at Xq26 and 2q33 resulting in (x,2) translocation have been reported in few instances.[8]
Clinically the tumor evolves as an asymptomatic tumor that reaches a point causing a painless swelling of the involved bone, as seen in our cases, few cases present with functional and cosmetic deformities such as displacement of the teeth with intact overlying mucosa. Centrifugal growth of the tumor causing bowing of the inferior border of the mandible.
Radiologically, JOF presents as a well-defined, concentrically expanding solitary mass with bone density or unilocular to multilocular lesion with central opacification or ground glass appearance.[10] This variation is due to stage, duration and histology of neoplasm. The circumscribed nature of ossifying fibroma distinguishes it from fibrous dysplasia.[9]
Histologically, they present as a benign lesion, composed of highly vascular and fibroblast rich connective tissue, which produce calcified substance either a cementum or bone. Clumps of osteoblast are also present. Psammomatoid type of JOF shows highly cellular fibrous stroma often with whorled pattern containing closely packed spherical ossicles resembling psammoma bodies
Complication includes intracranial extensions, cysts, recurrences and ocular disturbances. Complete surgical excision is the treatment of choice. [9]. The incidence of JOF is unknown. A literature review revealed 17 cases reported between the year 2003 and 2010.[11]
CONCLUSION
Juvenile psammomatoid ossifying fibroma requires early detection, complete surgical excision and a long term follow-up bears importance in clinical management due to their aggressive nature and high recurrence rate. In the case examined, surgical excision of the lesion was carried out. Patient was recalled at regular intervals. No evidence of recurrence was seen
ACKNOWLEGMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Ethical Clearance: N/A
Informed Consent: N/A
Source of Funding: Nil
Conflict of interest: Nil
References:
- Márcia de andrade et al. Ossifying fibroma of the jaws: A clinicopathological case series study. Brazilian dental journal.2013; 24(6): 662-666
- Keles B. Juvenile ossifying fibroma of the mandible: a case report. J oral maxillofac res. 2010(apr-jun);1(2):e5
- Khaji SI, Shah S, Baheti MR. Ossifying fibroma of the maxilla: an uncommon tumor presenting diagnostic and management dilemma for the clinician: a rare case report. J dent allied sci.2014;3:53-7
- Malathi N et al. Psammomatoid juvenile ossifying fibroma of the jaws. J oral maxillofac pathol.2011;15:326-9.
- Hahn SB, Kang ES, Jahng JS, Park BM, Choi JC. Ossifying fibroma. Yonsei med j.1991;32:347-55.
- Hamner JE 3rd, Scofield HH, Cornyn J. Benign fibro-osseous jaw lesions of periodontal membrane origin. An analysis of 249 cases. Cancer.1968;22:861-78.
- Solomon MC, Khandelwal S, AR, Carnelio S. Psammomatoid juvenile ossifying fibroma of the mandible – A Histochemical insight!. Internet j dent sci.2009;7
- Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology.2009 3rd ed. India: Elsevier publishers; P. 648
- Moghe S et al. Juvenile psammomatoid ossifying fibroma. IOSR. Journal of dental and medical sciences (IOSR-JDMS). Jun.2014. Volume 13; 6: 43-45
- Jithender Reddy Kubbi , Navadeepak Kumar K , Vivekanandh Reddy , Ramlal G. Juvenile ossifying fibroma. Journal of dental sciences and research.2011. vol. 2, issue 2, pages 1-5
- Breheret et al. R. Juvenile ossifying fibroma of the maxilla, european annals of otorhinolaryngology, head and neck diseases. 2011. 128, 317- 320.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License