IJCRR - 9(21), November, 2017
Pages: 54-57
Print Article
Download XML Download PDF
A Study of Adult Onset Generalized Eruptive Langerhans Cell Histiocytosis with Rare Association of Nail Pterygium
Author: Sunanda Mahajan, Vikram Lahoria, Vidya Kharkar, Uday Khopkar
Category: Healthcare
Abstract:Background: Langerhans cell histiocytosis(LCH) is a rare proliferative disease which generally affects children and rarely, adults. LCH in adults first presenting in the skin is very rare and often it is misdiagnosed as it mimics number of common skin conditions. Nail changes are another cutaneous feature which is not frequently described in adults.
Objectives and Methods: To present two new cases of adult LCH and a review of the literature of generalized cutaneous LCH in adults.
Results: Two adults with widespread papulo-nodular cutaneous eruptions in seborrheic distribution. Both the cases had palmoplantar purpuric papules and involvement of nails with pterygium formation, which is a rare finding not frequently reported in LCH. There was pituitary involvement in the form of diabetes insipidus in both the cases though it was clinically symptomatic in only first case. Diagnosis of both the patients was established on the basis of histopathology and immunohistochemistry.
Conclusions: Extensive cutaneous and nail involvement (nail dystrophy and pterygium) is possible in adult onset LCH. Thus, high index of suspicion is necessary to make the diagnosis.
Keywords: Adult onset, Generalised, Pterygium, Langerhan cell histiocytosis
Full Text:
Introduction
Langerhans cell histiocytosis (LCH) is a rare disorder which is characterized by clonal proliferation of dendritic cells and mainly affects children under 10 years of age, although it can occur at any age, it is rarely reported in adults (1). It comprises a wide range of clinical presentations depending upon the organs it affects. The clinical course and prognosis of LCH is diverse which ranges from a spontaneously regressing single lesion to a life-threatening multisystem disease with rapid progression and sometimes even death. In adults, lungs are the most commonly involved system followed by bones and skin (2,3). Cutaneous lesions in LCH can be the great pretender and mimics number of common dermatoses(4) it creates more confusion when it is the presenting feature , which is rarely seen in adults. Nail changes are another cutaneous feature which is not frequently described in adults(9).
Objectives and Methods: Two new cases of adult LCH were studied with their complete workup and a review of the literature of generalized cutaneous LCH in adults.
Results: Two adults presented with widespread papulo-nodular cutaneous eruptions in seborrheic distribution of 2 years and 5 years duration respectively. Both the cases had palmoplantar purpuric papules and involvement of nails with pterygium formation, which is a rare finding not frequently reported in LCH. There was pituitary involvement in the form of diabetes insipidus in both the cases though it was clinically symptomatic in only first case. Diagnosis of both the patients was established on the basis of histopathology and immunohistochemistry.
Case 1
A 22 year old unmarried male presented with sudden onset of skin coloured to red raised itchy lesions over face which progressed gradually to become generalized over the next 2 years which showed ulcerations over the flexures since last 6-8 months. The patient had loss of appetite with recent weight loss (5 kgs in last 6 months) and increase in thirst and frequency of micturition.
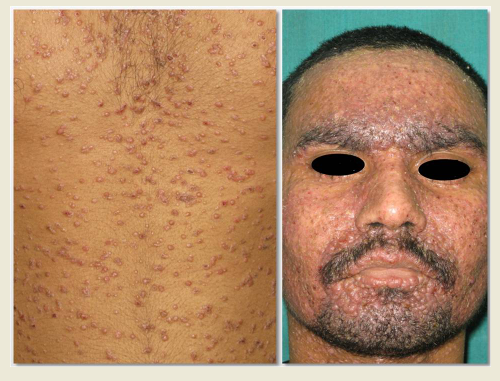
Examination revealed multiple erythematous and translucent umbilicated papules coalescing to form plaques intermixed with hemorrhagic papules, crusts and pustules distributed in seborrheic pattern. Dirty greasy scales matted with purulent discharge were seen over the scalp. Both palms and soles showed punctate purpuric micropapules. All twenty nails were dystrophic with erythematous papules and pustules periungually. Two finger nails of left hand showed pterygium (figure 1a and 1b). Papular lesions were seen over the lips and hard palate. Systemic examination was uneventful.
Complete blood counts with biochemical tests were within normal limits. Urine osmolality was low 195 mosm/kg while serum osmolality was slightly high, 303mosm/kg. Water deprivation test was positive indicating central diabetes insipidus. Serum FSH, LH and serum testosterone levels were lower than normal limits.
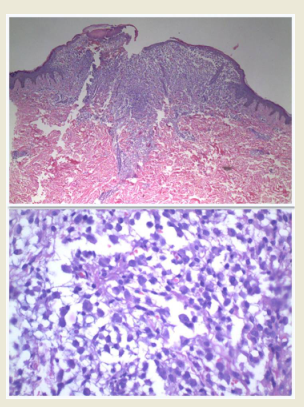
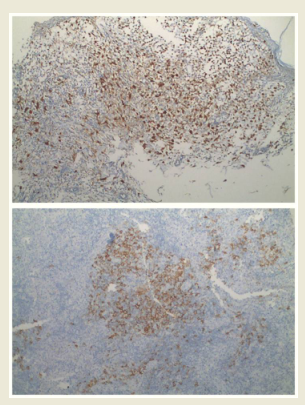
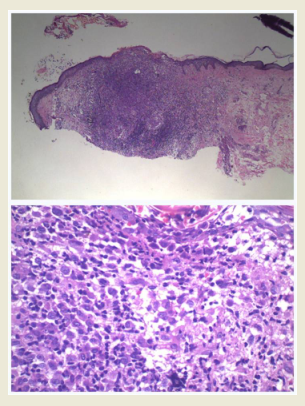
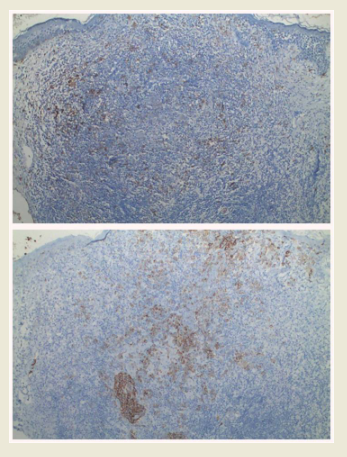
Biopsy done from one of the papules showed lichenoid infiltrate in upper dermis and infiltrate consisting predominantly of large histiocytes with kidney shaped nucleus with few lymphocytes. The cells stained positively with CD1a and S100 (figure 1c and 1d).
X-ray skull showed enlarged sella turcica which was supported by MRI and CT (plain) scan brain, suggestive of hypophysitis. Bone scan showed no evidence of skeletal involvement.PET scan showed hyper metabolism in the axilla, groin and perianal region with focal hyper metabolism in the spleen.
A final diagnosis of adult onset langerhans cell histiocytosis with pituitary and spleen involvement (multisystem disease with high risk group) was made.
The patient was started on Cytarabine, but showed no improvement after 4 cycles. Hence was switched to Cladiribine chemotherapy, following which significant improvement was seen after 6 cycles. Maintenance therapy was given in the form of 6-mercapto-purine(50mg) daily with methotrexate (25mg) once weekly for 1 month. PET-CT scan done after 11 months of chemotherapy showed no evidence of any metabolically active lesion (figure 1e).
For central diabetes insipidus patient was started with intranasal desmopressin daily at night which has to be maintained lifelong.
Case 2
A 48 year old male patient presented with minimally itchy multiple red raised lesions over legs since 5 years which gradually spread to become generalised over the next 3 years. Examination revealed multiple erythematous papules, pustules and nodules intermixed with umbilicated translucent papules over seborrheic distribution with few of them showing haemorrhagic crusts. Periungual region showed pustules and haemorrhagic crusts with dystrophic nails and toe nails showing pterygium formation. Multiple punctate purpuric papules with pustules and few keratotic papules were seen over soles (figure 2a and 2b). An erosive plaque with a few papules was present over the hard palate. Systemic examination was normal.
Complete blood counts and biochemical tests were within normal limits. Urine osmolality was low, 221mosm/kg while serum osmolality was normal, 289mosm/kg. Water deprivation test was positive indicating central diabetes insipidus, although the patient was asymptomatic. Serum FSH, LH and serum testosterone levels were lower than normal limits.
Biopsy from the papular lesion showed dense and diffuse nodular infiltrate in the dermis consisting of histiocytes having reniform nuclei and abundant cytoplasm with lymphocytes and a few eosinophils. On immunohistochemistry CD 1a and S100 were positive (figure 2c and 2d).
X-ray Skull, X-rays long bones, MRI (Brain), bone scan and PET-CT scan were normal.
The diagnosis of adult onset Langerhans cell histiocytosis with pituitary involvement (multisystem disease low risk group) was established. The patient was started on oral Thalidomide(150mg) per day
Discussion
Langerhans cell histiocytosis (LCH) is characterized by proliferation and infiltration of organs by pathological Langerhans cells. The aetiology and pathogenesis of LCH still remains largely undefined. The clinical manifestations of the disease are largely related to the pattern of infiltration of the organs and organ systems involved which includes bone, skin, hypothalamus, liver, lung and lymph nodes(6). It generally affects children with peak incidence at the age of 1-3 years and annual incidence of 4-5 cases per million. However, adult onset LCH is rare with annual incidence rate of 1-2 cases per million (1).
Although the features of this disease are well described in children, they remain poorly defined in adults, due to the rarity of this condition in adults. Thus the optimal treatment is not yet established (3).
According to the report of the International Registry of the Histiocyte Society on adult LCH (IRHSA), which studied the clinical characteristics of 274 cases across 13 nations, single-system disease accounts for 31.39% while multisystem disease was seen in 68.61%. Most common presenting symptoms were local pain(34%), particularly due to bone involvement, weight loss (11%), and fever (10%). Lung was the most frequently involved organ system followed by bone and then the skin(3).
Langerhans cell histiocytosis (LCH) in adults first presenting in the skin is very rare(5), and often it is misdiagnosed as it mimics number of common skin conditions, as seen in both our patients. The development of systemic findings may occur months to years after the initial presentation of skin manifestations. Both the patients had long standing skin eruptions, 2 years in first case and 5 years in second case before presenting to us. Predominant sites of cutaneous involvement typically include the seborrheic pattern with translucent papules being the typical lesions. These lesions frequently show scaling or crusting (4). Generalised skin eruptions are commonly seen in childhood LCH, but it is rarely seen in adults. However both our patients had extensive skin eruption, which is not yet reported in India to best of our knowledge. Various nail changes are well reported in childhood LCH and are considered as bad prognostic factor (7).It includes paronychia, onycholysis, subungual hyperkeratosis and purpuric striae of the nail bed. However in adults it is rare to observe such nail changes, especially pterygium formation, which is seen in both of our patients. Only one case of adult onset lch with pterygium formation has been reported so far (8).
Originally classified into Hand-Schuller-Christian disease, Letterer-Siwe disease, and Eosinophilic Granuloma, is not used anymore. The current classification which is developed by the Histiocyte Society provides uniform criteria for the diagnosis and clinical evaluation of patients. According to the current classification it is divided into a single system LCH (SS-LCH), in which one of the organs is affected and multisystem LCH (MS-LCH) involving at least two organs. The MS-LCH is subdivided into 'low-risk' and 'high-risk' ones. Low-risk patients have no involvement of 'high-risk' organs (liver, lungs, spleen, hematopoietic cells) (10)
Diabetes insipidus (DI) is one of the most peculiar endocrine complications of LCH that can predate the diagnosis or develop anytime during the course of the disease and is found in up to 30% of patients. The risk of development of diabetes insipidus among adults with LCH is probably equal to or even greater than that of children with LCH. Anterior pituitary dysfunction (APD) is found in up to 20% of patients, almost always with DI (4).
Growth hormone deficiency (GHD) is the most frequent disease-related APD found in up to 50% of patients with DI. While gonadotropin deficiency is the second most common deficiency, presenting with menstrual disturbances in women and decreased libido in men (4).Both our cases had DI with APD, although there was no symptoms of DI in the second case.
Conclusion
These cases illustrate that extensive cutaneous and nail involvement (nail dystrophy and pterygium) is possible in adult onset LCH. Thus, high index of suspicion is necessary to make the diagnosis.
Even though asymptomatic, all patients should undergo a careful multidisciplinary evaluation and periodic follow-up to screen for possible asymptomatic localisation that could warrant prompt treatment and may prevent progression to systemic disease.
Such patients need to be treated at tertiary centre because the management is multidisciplinary which require care of oncologists, dermatologists and endocrinologists
Acknowledgement:
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Source of Funding : none
Conflict of interest : none




References:
- Abla O, Egeler RM, Weitzman S. Langerhans cell histiocytosis: current concepts and treatments. Cancer Treat Rev 2010;36:354-9
- Götz G1, Fichter J. Langerhans'-cell histiocytosis in 58 adults. Eur J Med Res2004; 9(11):510-4.
- Aricò, M. et al. Langerhans cell histiocytosis in adultsReport from the International Registry of the Histiocyte Society. European Journal of Cancer 2003;Volume 39,Issue 16:2341 - 2348,.
- Girschikofsky M, Arico M, Castillo D. Management of adult patients with Langerhans cellhistiocytosis: recommendations from an expert panel on behalf of Euro-Histio-Net. Orphanet J Rare Dis 2013;8:72
- Edelbroek, J.R. et al. Langerhans cell histiocytosisfirst presenting in the skin in adults: frequent association with a second haematological malignancy. British Journal of Dermatology 2012;167:1287-1294
- Arico` M, Egeler RM. Clinical aspects of Langerhans cell histiocytosis. Hematol/OncolClin North Am 1998; 12:247-258.
- Penwadee Timpatanapong, Phongjan Hathirat, Parttraporn Isarangkura; Nail Involvement in Histiocytosis XA 12-Year Retrospective Study. ArchDermatol 1984;120(8):1052-1056.
- Moravvej, Hamideh,Yousefi, MaryamandBarikbin, Behrooz. An unusual case of adult disseminated cutaneous Langerhans cell histiocytosis. Dermatology Online Journal 2006; 12(6):13.
- Jain, S., Sehgal, V. N. and Bajaj, P. Nail changes in Langerhans cell histiocytosis. Journal of the European Academy of Dermatology and Venereology 2000; 14:212-215.
- Histiocyte Society 2009. Langerhans cell histiocytosis evaluation and treatment guidelines. Histocyte Society online. 2009. cited 2010-02.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License