IJCRR - 9(20), October, 2017
Pages: 10-13
Print Article
Download XML Download PDF
Methotrexate a Double Edged Sword - Effect of Methotrexate in patients of Psoriasis due to Medication Errors
Author: Yogesh Kalyanpad, Vidya Kharkar, Uday Khopkar, Sarvesh Thatte
Category: Healthcare
Abstract:Methotrexate is one of the most commonly used anti-neoplastic and disease modifying drug today. Side effects of methotrexate at high dose may be life threatening; however, these side effects oral dosing are variable because of the inter-individual variability of gastrointestinal absorption of this drug. Because of confusing nature of its dosing schedule and different routes of administration there are high chances of misinterpretation of prescription. Medication errors involving methotrexate revealed that errors occurred during all phases of use, often resulted from confusion about dosage, and often caused death or other serious adverse effects. Here we present three cases of toxicity due to methotrexate medication error. All cases presented with multiple erosions and ulcers on skin and mucous membrane, organ failures, bone marrow suppression.
Keywords: Medication error, Methotrexate, Toxicity
Full Text:
Introduction
Methotrexate is an anti-folate first developed to treat certain types of cancers including acute lymphoblastic leukaemia, osteosarcoma and non-Hodgkin's lymphoma. But recently it has been used commonly to treat certain non-malignant diseases like rheumatoid arthritis, psoriasis, other autoimmune diseases and ectopic pregnancy. Doses of methotrexate for rheumatoid arthritis can be as low as 2.5 mg, while 15 g/m2 can be used along with leucovorin rescue therapy in osteosarcoma with a staggering 10,000-fold difference. Scheduling of doses also varies widely, from cyclical protocols for cancer chemotherapy to weekly for rheumatoid arthritis and sarcoidosis. Methotrexate can be administered orally, intravenously, intramuscularly or intrathecally which further adds to this complexity.1
Side effects of high dose of methotrexate may be life threatening, however these side effects of oral methotrexate are variable because of the inter-individual variability of gastrointestinal absorption of this drug. Since folic acid plays a major role in cell division, its inhibition is directly associated with major toxicity. Bone marrow, gastrointestinal mucosa, skin and hair are particularly vulnerable to the effects of methotrexate, secondary to their high rate of cellularturnover.2
Frequent serious medication errors involving methotrexate have been reported and some patients have died. The errors have involved some aspect of the dosage regimen and patient negligence3, 4. We report three cases of methotrexate induced fatal drug reactions which were associated with medication errors.
Methods and materials
Patient presenting with history of methotrexate consumption for skin condition (psoriasis) and developing a skin rash, oral lesions and systemic symptoms were selected. Detailed history along with a thorough clinical examination was carried out. Investigations included all routine tests like complete blood count, liver function tests, renal function test serum electrolytes, X-ray chest, urine and stool examination. A skin biopsy was performed for all the patients.
Results
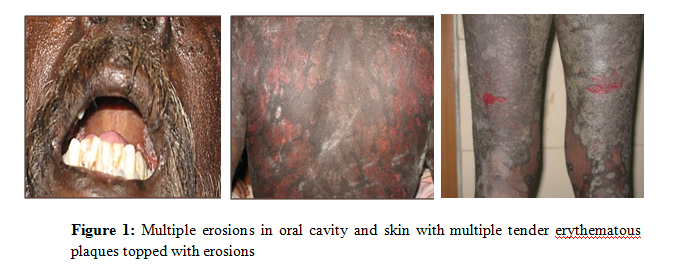
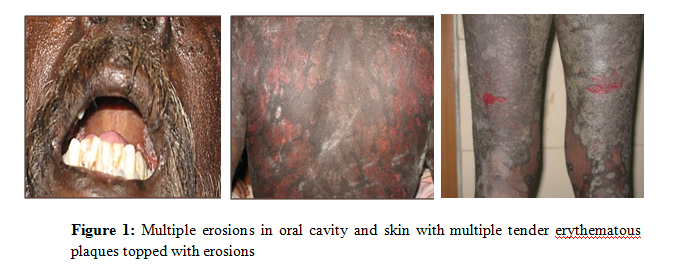
First case wasa62-year-oldmalepresented with multiple erosions in the oral cavity, trunk and extremities of duration four days(Fig 1). There was gradual worsening of his symptoms with odynophagia, dysphagia and diarrhoea. Patient was diagnosed as psoriasis and treated by an Ayurveda practitioner since one and half years. Patient also gave history of start of new medication since last two weeks
On enquiry patient was taking oral methotrexate 2.5 mg once daily for 10 days. Then to reduce itching patient himself increased dose to 5 mg two times a day for last 4 days.
The haematological examination showed severe neutropenia, thrombocytopenia and elevated liver enzymes (SGPT & SGOT), serum creatinine and blood urea nitrogen levels (Table 1).
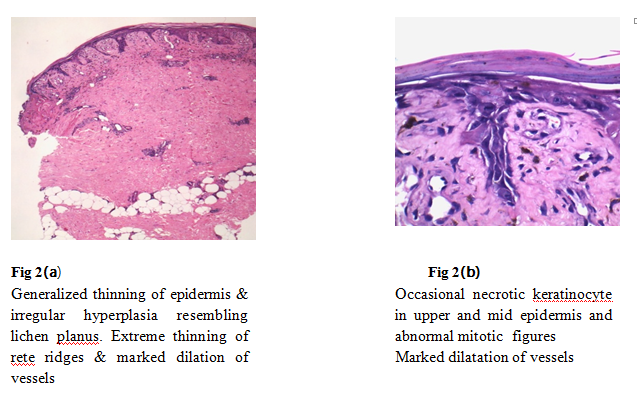
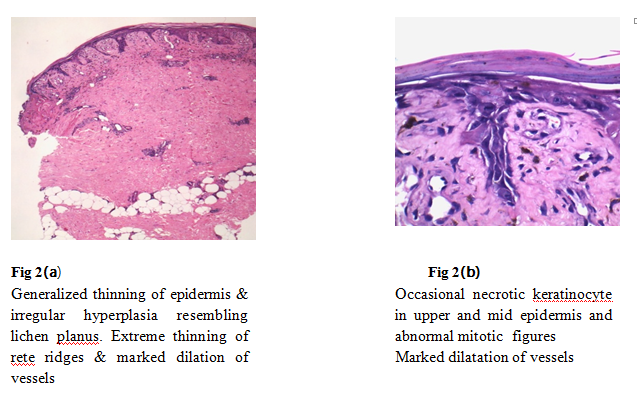
A skin biopsy sample was taken from erythematous tender plaque. Histopathological examination showed generalized thinning of epidermis & irregular hyperplasia. Extreme thinning of rete ridges and marked dilation of vessels, on higher magnification occasional necrotic keratinocyte and abnormal mitotic figures seen.On clinic-pathological correlation the patient was diagnosed as a case of methotrexate toxicity (Fig 2). Patient was admitted in medicine ward and started on Inj. Folinic acid 150 mg 6 hourly, Inj. GCSF 300 mg once daily, Inj. vancomycin 1 gm once daily, Inj. fluconazole 200mg once daily, Inj. metronidazole 400 mg three times daily, with adequate hydration and alkalization of urine.
Repeated haematological investigation showed no significant improvement. The same day patient succumbed to death due to septic shock with acute renal failure secondary to febrile neutropenia because of methotrexate toxicity.
Second case was a 45 year old female presented with psoriatic erythroderma, pustules with arthropathy and was admitted for the same.(Fig 3) The haematological investigations showed blood cell counts including white blood cells and platelet count within normal limits. After investigations, patient was started on oral acitretin 25 mg once daily along with tablet methotrexate 7.5 mg once a week which was increased to 15 mg once a week after two weeks.
Despite intensive treatment no improvement was seen and pustules continued to occur. Hence Cyclosporine 100 mg twice daily was added for quick response. Patient responded well to the treatment with clearance of erythema and scaling. With all normal haematological parameters, patient was discharged with tapering doses of cyclosporine 100 mg once daily along with capsule acitretin 25 mg once daily and methotrexate 15 mg once a week orally.
After 10 days of discharge, patient presented with fever with chills, odynophagia, oral ulcers, congestion of eyes, epistaxis and crusted lips. In spite of proper counselling at the time of discharge patient had followed advice from local chemist and had taken methotrexate 15 mg once daily for last 10 days except on Sunday when she took folic acid.
On investigation patient had severe anaemia, leukopenia, thrombocytopenia, slightly raised liver enzymes (SGPT), markedly raised serum creatinine, blood urea nitrogen and PT/INR (17.7/1.4) values. On clinico-histological evidence, the case was confirmed as methotrexate toxicity.
Patient was admitted in medicine ward and started on treatment similar to patient described as case 1. Patient went into septic shock with peripheral circulatory failure. Patient similarly succumbed to death.
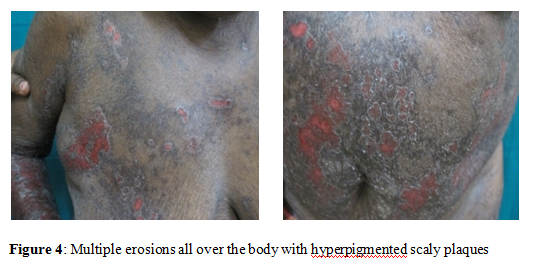
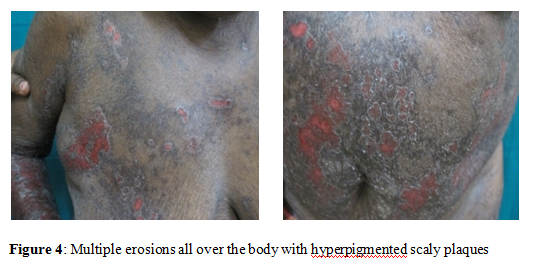
Third case was a55-year-old female came with complaints of painful erosions all over body and fever with chills for 4 days(Fig 4). On examination she had pallor and blood pressure was 84/60 mm of Hg at the time of admission. She was diagnosed as psoriasis and started on methotrexate by physician. On enquiry instead of taking methotrexate 7.5 mg in three divided doses as prescribed by physician patient took 7.5 mg three times a day that is 22.5 mg per week, for three weeks.
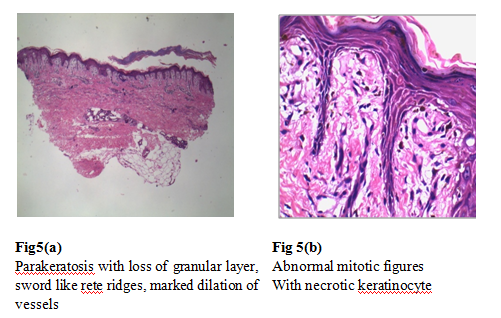
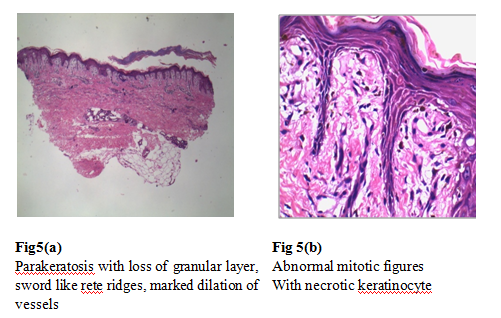
On haematological investigation patient was found to have anaemia, sever leukopenia and thrombocytopenia, raised liver enzymes (SGPT) and serum creatinine (Table 1). Skin biopsy showing extreme thinning of rete ridges appearing like swords with abnormal keratinocyte and mitotic figures. On clinic-pathological correlation with patient history, diagnosis of methotrexate toxicity was made (Fig 5).
Patient succumbed to death due to septic shock with acute renal failure and febrile neutropenia due to methotrexate toxicity.
Discussion:
The National Coordinating Council for Medication Error Reporting and Prevention defines a "medicationerror as any preventable event that may cause or lead to inappropriate medication use or patient harm, while the medication is in the control of the healthcare professional, patient or consumer.5
Methotrexate is one of the most commonly used anti-neoplastic and disease modifying drug today. It is also one of the most toxic drugs. In 1951 Gubner et al recognised methotrexate was effective for the treatment of psoriasis. In all the cases described above, patients were taking methotrexate for their primary disease. All of them presented with extensive erosions in oral cavity and all over body. Excess ingestion of multiple doses of methotrexate was found due to medication error. Signs of acute organ failure and myelosuppression were also observed.
Therefore, in the literature, most cases of cutaneous lesions showed some form of pre-existing cutaneous pathology, i.e. either physical insults or underlying dermatosis. This is seen with almost all the cases described above.6
A study by Moore TJ et al had showed that total of 106 cases of reported medication errors associated with methotrexate were identified over a period of 4 years7. The medication errors resulted in 25 deaths (24%) and 48 other serious outcomes (45%). The most common types of errors involved confusion about the once-weekly dosage schedule (30%) and other dosage errors (22%). Hence medication errors seen with use of methotrexate can be due to many drug related factors. The problem can beginat the level of physician which could be due to inadequate counselling about drug dosage, lack of re-emphasis about weekly dosage system or use of confusing brand names. This can also be seen at pharmacy level when modified dosage forms are prescribed or when medications provided over the counter. Finally, and most commonly it can be because of patient related factors like confusion among various drugs, misinterpretation about dosage, for faster relief self-administration of larger dosage or forgetfulness of ingested dosage in old patients.7
One of the best preventive practices while using drugs like methotrexate is to educate the patient about their medications. Illiterate patients should be asked to verify the dispensed drug with the doctor or any literate person at home or in the neighbourhood. They should also be educated about the outcomes of pharmacotherapy by written handouts and audio-visual teaching aids onmedication.8Involvement of close relative during counselling and creating awareness among patient as well relatives about possible side effects can be crucial.
Conclusions
Medication errors in methotrexate consumption can lead to serious complications and even death can occur. Our three patients despite the timely right diagnosis of methotrexate toxicity and treatment unfortunately succumbed to death. These medication errors can be prevented not only at the physician and pharmacist level but most importantly at patients level with adequate counselling and creating awareness about side effects.
Acknowledgement
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Table 1: Laboratory investigation of patients at the time of admission
|
|
Values on admission
|
|
Case 1
|
Case 2
|
Case 3
|
|
Hb (gm %)
|
11.2
|
6.5
|
9.2
|
|
WBC (cells/ml)
|
300
|
300
|
300
|
|
Platelet (cells/ml)
|
20000
|
60000
|
60000
|
|
SGPT (IU)
|
99
|
42
|
55
|
|
SGOT (IU)
|
38
|
05
|
32
|
|
Sr.creatinine (mg/ml)
|
2.2
|
6.2
|
1.2
|
|
BUN (mg/ml)
|
96
|
87
|
-
|

References:
- Baughman RP, Lower EE. A clinical approach to the use of methotrexate for sarcoidosis. Thorax 1999; 54:742-6.
- Gaies et al., Methotrexate Side Effects: Review Article. J Drug MetabToxicol 2012, 3:4.
- Lomaestro BM, Lesar TS, Hager TP. Errors in prescribing methotrexate. JAMA 1992; 268:2031-2.
- Sweet JM, Holstege CP. Bone marrow failure from medication error: diagnosis by history, not biopsy. Arch Intern Med 2001; 161:1911-2.
- National Coordinating Council for Medication Error Reporting and Prevention Medication ErrorIndex. Updated c1998-2011. Cited 2014 Dec 17. Available from: http://www.nccmerp.org/aboutMedErrors.html.
- Lee HJ, Hong SK, Seo JK, Lee D, Sung HS. A Case of Cutaneous Side Effect of Methotrexate Mimicking Behçet's Disease. Ann Dermatol. 2011; 23:412-4.
-
Moore TJ, Walsh CS, Cohen MR. Reported medication errors associated with methotrexate. Am J Health Syst Pharm 2004; 61:1380-4
-
Malhotra K, Goyal M, Walia R, Aslam S. Medication Errors: A Preventable Problem. Indian Journal of Clinical Practice 2012; 23:17-21.







 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License