IJCRR - 8(13), July, 2016
Pages: 28-30
Date of Publication: 12-Jul-2016
Print Article
Download XML Download PDF
THE ROLE OF DECOY CELLS IN URINE CYTOLOGY IN DETECTION OF POLYOMAVIRUS INFECTION IN POST RENAL TRANSPLANT PATIENTS
Author: Pavithra P., Praveen S. Kumar
Category: Healthcare
Abstract:Objective: To assess the role of urine cytology as a simple and noninvasive tool in assessment of post renal transplant polyoma virus infection
Case Report: Polyoma virus BK can infect the renal transplant patients on immunosuppressive therapy resulting in progressive renal allograft dysfunction and graft loss. We report a case of 42 year old male who underwent renal transplant six weeks ago followed by immunotherapy, had signs of rejection in the immediate post- transplant period for which he was put on antithymocyte globulin. He now presented with dysuria and urine cytology was done. Viral cytopathic effect in the form of enlarged nucleus with basophilic viral intranuclear inclusions and ground glass chromatin known as \"decoy cells\" were seen.
Conclusion: Urine cytology can be used as a simple and cost effective screening method for monitoring the renal transplant patients for polyoma virus allograft nephropathy
Keywords: Polyoma virus, Decoy, Renal transplant, Urine cytology
Full Text:
INTRODUCTION
Renal allograft recipients are at risk of reactivation of polyoma virus (PV) BK leading to derangement of renal function and allograft loss.[1] Since the pioneering study conducted by Coleman et al, urine cytology has been used as an inexpensive and efficient screening method to detect the cytopathic effect of PV BK in renal transplant patients. [2] The term “decoy cells”was coined for epithelial cells with polyoma viral inclusions in urine cytology specimens to avoid their misinterpretation as malignant cells.[3, 4] We present a case of polyoma viral changes in the epithelial cells of urine in a middle-aged male who underwent renal transplantation.
CASE REPORT
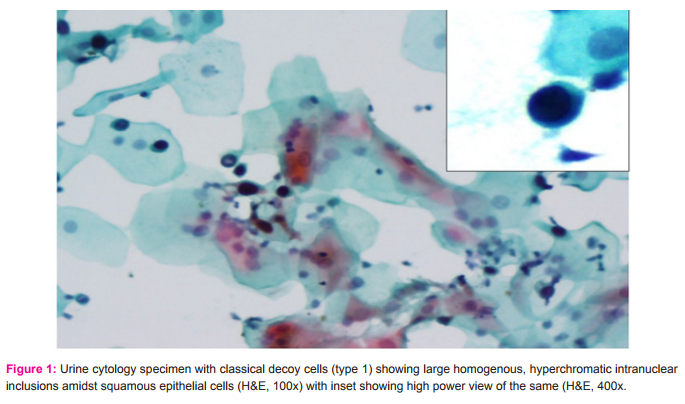
A 42 year old male underwent renal transplantation six weeks ago and was started on immunotherapy with triple immunosuppressants including tacrolimus, mycophenolate mofetil and steroids. Patient presented with signs of rejection in the immediate post- transplant period, for which he was put on antithymocyte globulin (ATG). The patient presented with dysuria and urinary tract infection. Urine samples were collected to rule out possible viral infection. Fresh urine sample was collected, cytospin smears were made, alcohol fixed and stained with Papanicolau stain. Smear showed epithelial cells with high nuclear cytoplasmic ratio, large intranuclear, smudgy ground- glass like viral inclusions characteristic of type I decoy cells ( > 10 decoy cells/ cytospin smear).(Figure 1) No cytoplasmic inclusions were seen. Serological tests for cytomegalovirus and adenovirus were negative. Polyoma virus infection was suspected, following which the dose of immunosuppressants was decreased along with a course of antibiotic and the patient showed improvement.
DISCUSSION
Primary polyomavirus infection occurs in early childhood and the virus remains latent in the urinary tract epithelium.
Three species, BK virus, JC virus and Simian virus (SV40) causes disease in humans. Immunosuppression of the allograft recipient can lead to reactivation of the infection and development of nephropathy resulting in allograft failure in 1- 5% of kidney transplant recipients. When reactivated, the virus proliferates within the nuclei of renal tubular and urothelial cells producing viral cytopathic effect manifested with nuclear enlargement and basophilic intranuclear inclusions. Such cells known as decoy cells can be identified by urine cytology. [5] Four morphological types of “Decoy cells” have been described in literature: Type 1- classic decoy cells characterized by large, homogenous, amorphous ground-glass like intranuclear inclusion bodies and a condensed rim of chromatin; Type 2- granular intranuclear inclusions surrounded by a clear halo, i.e., cytomegalovirus (CMV)-like; Type 3- multinucleated decoy cells with granular chromatin; Type 4- vesicular nuclei with clumped chromatin and nucleoli.[6] The urine samples can be classified semi quantitatively as: 1-4 infected cells per cytospin (1+), 5-10 infected cells per cytospin (2+), 11 infected cells per cytospin, but still representing a minority of the total cells in sediment (3+), and too many infected cells to count representing the majority of the cells in the sediment (4+).[7] Urine with large numbers of decoy cells (>10/cytospin), inflammatory sediments and biopsy proven PVN have been noted to have significantly greater decay in renal function than patients with no evidence of PVN. [8] Decoy cells should not be mistaken for malignant cells. Decoy cells are medium sized basophilic cells with cytoplasm like tail of a comet and nuclei with clumped ground glass like homogenous chromatin, where as malignant tumor cells have evenly distributed hyperchromatic chromatin with irregular nuclear membrane and little cytoplasm. [9,1] Drachenberg et al. observed that urine samples seem to be the most sensitive and cost effective screening method for PV infection. They also found that immunohistochemical stains are useful to confirm the presence of PV, but do not increase the sensitivity of diagnosis, hence should be used only after detection of decoy cells in urine. [8]
CONCLUSION
Urine cytology can be used as a simple and cost effective screening method for monitoring the renal transplant patients for polyoma virus allograft nephropathy. It can be conveniently used in centres lacking immunohistochemistry and molecular biology services.
ACKNOWLEDGEMENT
We acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. We are also grateful to the authors, editors and publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Fogazzi GB, Cantu M, Saglimbeni L. Decoy cells in the urine due to polyoma virus BK infection: easily seen by phase contrast microscopy. Nephrol Dial Transplant 2001; 16: 1496-8.
2. Coleman DV, Mackenzie EF, Gardner SD, Poulding JM, Amer B, Russel WJ: Human polyoma virus BK infection and ureteric stenosis in renal allograft recipients. J Clin Pathol 1978; 31: 334- 8
3. Koss LG. On decoy cells. Acta Cytol 2005;49:233-4. [PUBMED]
4. DeMay RM. Urine: The art and science of cytopathology, Exfoliative Cytology. Chicago: American Society of Clinical Pathologists (ASCP);1996. p. 394-5
5. Vidas Z, Misic M, Pacic A, Jurenec F, Knotek M, Skelin IK. The value of urinary decoy cells finding in patients with kidney transplantation. Coll Anthropol 2010; 34(1): 153-7
6. Colvin RB, Nickeleit V. Renal transplant pathology. In: Jennet JC, Olson JL, Schwartz, Silva FG, editors.Heptinstall’s Pathology of the kidney. 6th ed. Philadelphia: William and Wilkins; 2007. pp. 1441–8.
7. Geetha V, Rao L, Monappa V, Susmitha MS, Prabhu R. Decoy cells in urine cytology: A useful clue to post-transplant polyoma virus infection. J Cytol. 2012 Apr-Jun; 29(2): 133–134.
8. Drachenberg CB, Beskow CO, Cangro CB, Bourquin PM, Simsir A, Fink J, et al. Human polyomavirus in renal allograft biopsies: Morphological findings and correlation with urine cytology. Hum Pathol. 1999;30:970–7.[PubMed]
9. Drachenberg CB, Hirsch HH, Ramos E, Papadimitriou JC: Polyomavirus disease in renal transplantation – review of pathological findings and diagnostic methods. Hum Pathol 2005; 36: 1245-55.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License