IJCRR - 4(17), September, 2012
Pages: 80-84
Date of Publication: 14-Sep-2012
Print Article
Download XML Download PDF
DRUG- RESISTANCE PROFILE OF NEW PTB PATIENTS WITH OR WITHOUT HIV INFECTION
Author: Niladri Sekhar Das
Category: Healthcare
Abstract:Tuberculosis is the commonest opportunistic infection in persons infected with human immunodeficiency virus (HIV). HIV is the most powerful risk factor for reactivation of latent tuberculosis infection to active disease. Emergence of drug resistant isolates of M. tuberculosis (Mtb) highlights the need for continuous monitoring of drug resistance to anti tuberculosis drugs. The aim of our study was to see the anti tubercular drug resistance profile of M.tb in HIV seropositive and seronegative patients. Material and methods- We enrolled 100 new pulmonary tuberculosis (PTB) patients. This study was carried out at Department of Microbiology MGIMS, Sevagram, Wardha Maharashtra from 2007-2009. For every patient staining and culture was done from sputum sample by conventional method. After the identification of isolates as M.tb drug sensitivity testing was done. HIV antibody status was identified in every patient by using rapid and ELISA test. Results were analyzed using SPSS software. Results: There were 8 patients who were HIV seropositive out of total 35 culture positive cases. No resistant patterns were detetected in case of HIV +ve patients with TB infection. Out of 27 HIV seronegative cases with TB infection, 4 cases showed mono-resistant to streptomycin. No multi drug resistant (MDR) strain was detected neither in HIV positive nor in HIV negative cases. Conclusion: HIV infection may not be associated with drug resistant tuberculosis. However due to high prevalence of HIV\?TB infection in the country, monitoring of drug resistance in M. tuberculoisis isolates needs prioritization to ensure success in national tuberculosis control programme.
Keywords: Human immunodeficiency virus (HIV), Pulmonary tuberculosis (PTB), Mycobacterium tuberculosis (Mtb), Multi drug resistant (MDR)
Full Text:
INTRODUCTION
Tuberculosis (TB) is one of the most serious diseases that physicians have recognized and grappled with through the millennia due to its high risk of person to person transmission, morbidity, and mortality. Currently there are 9.2 million new cases of tuberculosis every year with 1.7 million deaths occurring worldwide1 . Despite the discovery of the tubercle bacillus more than a hundred years ago, and all the advances in our knowledge of the disease made since then, tuberculosis still remains one of the major health problems facing mankind, particularly in developing countries. In India each year, 1.9 million new cases of TB occur in the country, of which about 0.8 million are infectious new smear positive pulmonary TB cases2 . The situation is expected to worsen due to the emergence of multi-drug resistant tuberculosis (MDRTB).
Development of drug resistance in M. tuberculosis isolates may adversely impact the management of the disease. Inadequate therapies and indiscriminate use of antibiotics causes such emergence of multi drug resistant bacilli and HIV/AIDS pandemic resulting in accumulation of pool of individuals who are more susceptible to TB have worsened the TB scenario. A High HIV seroprevalence among newly diagnosed TB patients has been reported in India.3, 4 . On the global situation of drug resistance in M.tb , first comprehensive study was conducted by the Research and Surveillance unit, Global TB Programme, WHO5 and was observed that, the rates of acquired resistance were invariably higher than primary resistance for each drug and multi drug resistance was more common when resistance was acquired rather than when it was primary. The increasing prevalence of multidrug resistance in several parts of the world including India has been one of the major reasons for declaring tuberculosis control as a global emergency by WHO6,7 . Several outbreaks of MDR-TB showed the importance of continuous monitoring of drug resistance for treatment of TB patients and initiating adequate public health measures. The present study was undertaken with the objective of comparing the anti TB drug resistance profile of MTB isolates in new PTB patients with or without HIV infection.
MATERIAL AND METHODS:
Among 100 suspected tuberculosis patients study was done at Microbiology Laboratory in MGIMS, Sevagram between 2007 to 2009 with due permission from the institutional ethical committee. Sputum was collected from each individual, smear was made and staining was done by Ziehl–Neelson method. For isolation rest of the sample was decontaminated by NALC-NaOH method8 and inoculation was done on 2 LJ slopes. LJ bottles were observed weekly till the colonies grew sufficiently for identification whereas negative LJ culture was noted if there was no growth after incubation at 370 c for 8 wks. Isolates were identified later by conventional biochemical methods9 After the identification of the strain as MTB, drug sensitivity testing was performed against 1st line drugs by LJ proportion method described by Canetti et al 1969 10. For Drug sensitivity testing stock and working concentration of drugs were made according to Guidelines of TRC manual 200611. The concentration of drugs used were Streptomycin 4 µg/ml, INH 0.2 µg/ml, Rifampicin 40 µg/ml and Ethambutol 2 µg/ml. Before drug sensitivity testing by LJ proportion method, drug containing LJ slopes was made. At first preparation of standard suspension 11 and dilution was made. 0.1 ml of each of the two bacterial dilutions, 10–3 mg/ml and 10–5 mg/ml were inoculated on two slopes of LJ medium without drug and one slope of medium with drug. The standard strain of M.tuberculosis, H37Rv was tested with each batch of sensitivity testing. All the LJ slopes for DST were placed in the incubator at 37 °C. Reading and reporting of the LJ slopes were done according to the reference10 Detection of HIV status in every patient was done by rapid method (TRIDOT) using serum which was collected in a plain bulb. If any sample was found to be positive by rapid method, confirmation was done by ELISA (Vironostika) confirmed by second ELISA at NARI Pune.
RESULTS:
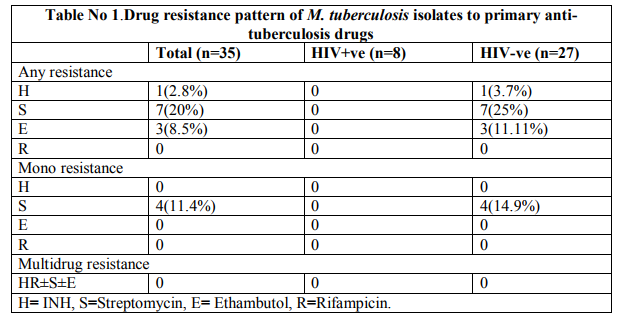
We got 35 total MTB isolates no NTM (Non tubercular mycobacterium) was isolated. Among 35 MTB isolates 87.9 percent (29/33) from smear positive and 9 percent (6/67) from smear negative patients were obtained. Of these 8 isolates were HIV seropositive and 27 HIV seronegative (Table no 1). Among the 35 total MTB isolates, monoresistant was found with Streptomycin that was 11.4% only in HIV seronegative patients (Table no 1). Resistance to any 1st line drug was seen (7/35), in 20% isolates. Drug resistance to at least one drug was found in (7/27), 25.9% isolates in HIV seronegative cases whereas no resistant strain was isolated even for a single drug in HIV+ve cases however in HIV seropositive cases we got (8/8), 100% isolates sensitive to all four drugs. The prevalence of polyresistance (resistance to two or more drugs, but not both isoniazid and refampicin) was found to be (3/27), 11.11% only in HIV seronegative with TB infective patients. Neither individual drug resistance nor the MDR or polyresistance was found to differ significantly in the HIV infected and uninfected TB patients.
DISCUSSION
Emergence and spread of drug resistance in M.tuberculosis is a serious threat to tuberculosis control programme because patients with drug resistance bacilli respond less readily to therapy than those with sensitive bacilli, resulting in preferential spread of the drug resistant bacilli in the community. Drug resistance develops either due to infection with a resistant strain, or as a result of inadequate treatment such as when a patient is exposed to a single drug, or because of selective drug intake, poor compliance, use of inappropriate non-standardized treatment regimens, irregular drug supply, poor drug quality, or rarely erratic absorption of medications 12 . Though the development of drug resistance in India was noted since the beginning of the chemotherapeutic era, it was based on clinical perception and several isolated reports, which failed to give an idea of the national situation as a whole. In this direction the first definite step was taken in 1965-67, when the ICMR conducted two surveys to estimate the prevalence of drug resistance13 . In this study resistance to Isoniazid ranged from 11-20 per cent, to Streptomycin 8- 20 per cent and to both drugs 4-11 per cent. The second study showed resistance to Isoniazid from 15-69 per cent, to Streptomycin 12-63 per cent and to both drugs from 5-58 per cent. However these studies were carried out in the pre-Rifampicin era. Subsequently after about two decades (1980?s), 11 other studies from different parts of the country reported similar resistance to Isoniazid and Streptomycin like those in the earlier studies with the notable exception of Rifampicin resistance being observed in 10 of the 11 publications and the level of MDRTB in all the centers was observed but it was less than 5 per cent. According to third Global Report total prevalence of drug resistance among new cases in India (Wardha) was 19.8% and MDR was 0.5 %. Several small surveys conducted across the country have shown the prevalence rates of MDR-TB in the country at around 3% among new cases, and 12% among retreatment cases. A large scale population based survey in the states of Gujarat and Maharashtra has also indicated similar resistance levels (new- 3% and retreatment- 12- 17%) 13. We found that prevalence of resistance to isoniazid and streptomycin was 0 and 11.4 percent and that to both drugs were 2.8%. The issue of whether infection with HIV is a risk factor for drug resistant tuberculosis still remains unanswered since results of some studies supported this hypothesis while some did not. A study conducted in newyork city 14 revealed that HIV infected TB patients were significantly more likely to develop resistance to at least one drug and MDR than those without HIV infection. No significant difference was found in drug resistance between HIV seropositive and HIV seronegative tuberculosis patients in our study, which is in accordance with the findings from other studies in Europe 15, 16 . In conclusion, we didn?t find any kind of drug resistance in anti-tubercular drug especially in case of HIV seropositive cases. In view of the conflicting results from other studies and high prevalence of HIV-TB in our country, we feel that time to time monitoring of anti-tuberculosis drug resistance pattern in TB patients in general and HIV seropositive tuberculosis patients in particular would provide important data, which may be crucial for the control of tuberculosis.
References:
1. Global tuberculosis control: surveillance, planning, financing: WHO report 2008. Geneva: World Health Organization (WHO/HTM/TB/2008.393).
2. TB India 2008. RNTCP Status Report.
3. Paranjape R S ,Tripathy SP, Menon PA, Mehendale SM, khatavkar P, Joshi DR.et al. Increasing trend of HIV seroprevalence among pulmonary tuberculosis patients in Pune, India .indian J Med res 1997;106: 207- 11
4. Tripathy S, Joshi DR, Mehendale SM , Menon P, Joshi AN, Ghorpade SV, et al.Sentinel surveillance for HIV infection tuberculosis patients in India. Indian J tuberc 2002; 49: 17-20.
5. Cohn DL, Bustreo F, Raviglione MC. (1997). Drug resistant tuberculosis: review of the worldwide situation and the WHO/IUATLD global surveillance project. Clin Infect Dis 1997; 24(1): 121-130.
6. Anti tuberculosis drug resistance in the world. The WHO/ WATLD global project on anti tuberculosis surveillance .Geneva,Switzerland;1997.WHO/TB/97.229.
7. Anti tuberculosis drug resistance in the world ,report No.2.WHO/CDS/TB/2000.278
8. Procedure for isolation and identification of mycobacterium CDC manual1975.
9. Laboratory services in tuberculosis control .Part 3-Culture /WHO/98.258,1998.
10. Canetti, G., Fox, W., Khomenko, A., Mahler, H.T., Menon, N.K., Mitchison, D.A., et al. Advances in techniques of testing mycobacterial drug sensitivity, and the use of sensitivity tests in tuberculosis control programmes. Bulletin of the World Health Organisation, 1969. 41, 21-43.
11. Bacteriological methods and Laboratory diagnosis of Tuberculosis TRC Chennai 2006.
12. Behera D. Drug Resistant Tuberculosis In India – Is it a matter of concern? Ind J Tuberc 2007; 54:105-109.
13. Multi-drug resistant and Extensively drug resistant TB in India, Consensus statement on the problem, prevention, management and control, From the consultative meeting of national experts organized by the TB Research Centre, ICMR, Govt. of India, on 14-15 September 2007.
14. Gordin FM, Nelson ET,Matts JP, Cohn DL, Ernst J,Benator D,et al. The impact of human immunodeficiency virus infection on drug resistant tuberculosis . Am J.Respir Crit care Med 1996; 154: 1478-83.
15. Migliori GB, Centis R, Fattorini L, Besozzi G, Saltini C, Scarparo C, et al. Mycobacterium tuberculosis complex drug resistance in Italy. Emerg Infect Dis 2004;10:752-3
16. Shafer RW, Chirgwin KD, Glat AE, Dahdouh MA, Landesman SH, Suster B. HIV prevalence , immunosuppression , and drug resistance in patients with tuberculosis in an area endemic for AIDS.AIDS 1991;5:399-405.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License