IJCRR - 2(8), August, 2010
Pages: 25-32
Print Article
Download XML Download PDF
STRENGTHENING AND UPGRADING OF SUB-CENTERS IS ESSENTIAL IN THE EXISTING PUBLIC HEALTH CARE SYSTEM: A STUDY CONDUCTED IN A BLOCK OF WARDHA DISTRICT
Author: Abhay Bhausaheb Mudey, Mehiliquea S, Ramchandra C. Goyal, Vasant V Wagh
Category: Healthcare
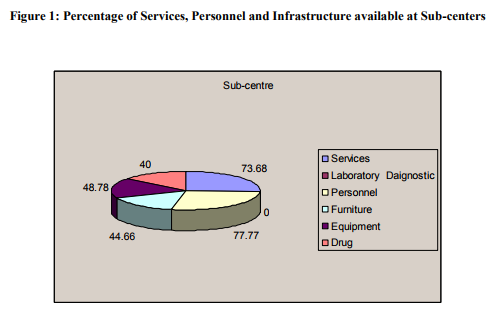
Abstract:Background: Indian Public Health Standards (IPHS) have prescribed certain standards providing basic primary health care services to the community. Sub-centers are still snowed under certain problems like non-availability of required staff, inadequate physical infrastructure and insufficient quantity of drugs and lack of community participation. Hence the present study was undertaken with the objectives to assess the availability and adequacy of paramedical and supporting staff, infrastructure facilities and their extent of utilization . Methods: This cross-sectional multistage sampling study which was carried out in 31 sub-centers of a Block of Wardha district, Maharashtra. IPHS assessment tool was used to collect information/data by interviews and observations technique. Face-to-face interviews were conducted with all the staff. Observations and responses were recorded in the prescribed IPHS format. Results: The study reveals that adequate Immunization, Ante-natal and Family planning services were available at all Sub-centers. Health Workers (female) were available (100%), Voluntary worker (51.61%) whereas Health Workers (male) were not available at any of the sub-centre. In majority of Sub-centers Drugs (40%), Equipments (48.78%), Furniture (44.66%), Basic sanitation and Infrastructure are inadequate and was fall short of IPHS expectations.
Conclusion: Hence balancing Infrastructure, pooling resources, Intersectoral co-ordination, optimization of health manpower, decentralization of Health Programmes is necessary to fulfill the criteria of IPHS of sub-centers in each Block.
Keywords: NRHM, IPHS, Sub- Centers, Block of District, Public health infrastructure.
Full Text:
Introduction:
It was recognized that in both developed and developing countries the standard of health services that the public expected was not being provided [1]. At the Joint WHO-UNICEF International Conference in 1978 at Alma-Ata (USSR) proclaimed Primary Health Care as a way to achieve the goal of Health for All. The Alma-Ata Declaration called on all governments to formulate national policies, strategies and plan of action to launch and sustain primary health care as part of a National Health System[2]. In India the first formal National Health Policy was formulated in 1983 and since then there has been marked changes in the determining factors relating to the health sectors and health status.
India is the second largest country in terms of population. In the public sector of rural India, health care services are provided through a network of Sub-Health Centers (sub-centers), Primary Health Centers (PHC), and Community Health Centers (CHC). The Health Care System in India has expanded considerably over the past few decades. There are 1, 44,988 Subcentre, 22,669 PHCs and 3,910 CHCs functioning in the country [3]. The subcentre provides interface with the community at the grass root level providing primary health care services [3].
Though such a vast network of health centers in rural areas looks impressive, sub-center area is still plagued by certain problems like non-availability of required staff and even if they are posted there is always, lack of training programmes in skilled works like family planning and immunization, inadequate physical infrastructure and facilities, insufficient quantity of drugs, and lack of community participation. Upgrading Public Heath Infrastructure in rural areas to measurable standards of quality is being introduced in order to improve the quality of services in these health care centers is a key strategic intervention under the National Rural Health
Mission (NRHM)[4]. A task group under the chairmanship of Director General of Health Services, Government of India, was constituted to recommend the standards to be called as Indian Public Health Standards (IPHS). The overall objective of IPHS is to provide health care that is quality oriented and sensitive to the needs of the community. These are a set of standards envisaged to improve the quality of healthcare delivery in the country under the National Rural Health Mission[5].
Sub-centre are accountable for Assured services like MCH and Family Planning services in which Ante-natal, intranatal, post-natal, new born and child care including immunization, contraception, adolescent health care, assistance to school health services, Janani Suraksha Yojana, treatment of minor ailments and First aid services whereas the specific services of SC includes visit of the doctor at Sub-centre at least once in a month at fixed day and time, Visit of the Health Assistant (male) or LHV to the Sub-Centre at least once a week, facility for referral of complicated cases of pregnancy / delivery available at Sub centre for 24 hours, the ANM/any trained personnel accompany the woman in labour to the referred care facility, the facility for Peripheral blood smear in fever cases and availability of DOTs at the sub-centre. As sub-centers are the first contact point between the health facility and community, the success of any country would depend on well functioning of sub-centers providing services of acceptable standard to the people. Hence it was felt necessary to assess the availability and adequacy of Paramedical staff, support manpower, infrastructure facilities and their extent of utilization at various Sub-centers in a Block of Wardha district, as per IPHS.
Material and Methods The present study was carried out with the aim of an assessment of Public Health Infrastructure at various Subcenters in a selected block of Wardha district using Indian Public Health Standards stated under National Rural Health Mission.
This is a cross-sectional study which was carried out during January 2008 to March 2008 at Sub-centers of Six Primary health care centers (PHC) of one Block of a Wardha district (MS) of Central India, which is also a field practice area of research institute and a medical college.
There are eight blocks in this district from which the study block was selected by simple random sampling. The selected block contains six PHCs with cumulative population of 1, 83,583. All the 31 sub-centers of these six PHCs were further selected for study by Purposive sampling.
An assessment of Sub-Centers was done against Indian Public Health Standards (IPHS) recommended by Director General of Health Services, Government of India. At all sub-centers data was collected by observations and face to face interview with Health Workers. Observations and responses were entered in the prescribed IPHS format for sub-centre[3].
Study tool: Indian Public Health Standards (NRHM) assessment tool/ check list was used to conduct the interviews at the facility level. The check lists were comprised mainly of location, average daily OPD attendance, services availability, staffing pattern, physical infrastructure, equipments, water supply, sewerage, waste disposal, electricity, communication facilities, drugs, equipments and furniture of subcenters.
Data entry and analysis: The collected data was entered into Microsoft office excels for analysis. Mean as a statistical technique was used to calculate the average percentage of the services, staffing pattern, physical infrastructure equipments and drugs in Sub-centers.
Results Assured services like adequate immunization, ante-natal, and family planning services were available at all Sub-centers. All sub-centers of five PHCs were existed in designated government building except one sub-centre (16.66%) existed on shared basis with Anganwadi and one sub-centre (16.66%) existed on shared basis with Zilla Parishad building . The five subcenters (83.34%) of the 6th Waifad PHC were existed in designated-government building except one sub-centre (16.66%) which was on rent.
At fifteen sub-centers (48.38%) the ANM do not reside at the sub-centre staff quarters and at six sub-centers (37.5%) ANMs, who resides at subcentre quarter has occupied even the clinical space for their residential use. Health Worker (female) was available at all the 31 sub-centers, whereas Health Worker (male) was not available at any of the sub-centre. Voluntary worker to keep the Sub-Centre clean and assisting ANM was not available at sixteen sub-centres (51.61%). Equipments available at Sub-centers of five PHCs were between 49-52% except at sub-centers of Deoli PHCs where availability is (41.81%). Furniture availability at sub-centers of Giroli PHC was (52.7%) whereas in the other PHCs sub center it was less than 50%. Drugs Kit A was available (50%) at sub-centres of Deoli PHC; (83.33%) of Giroli PHC; (50%) of Vijaygopal PHC; (50%) of Nachangaon PHC, (83.33%) of Gaul PHC and (66.66%) of Waifad PHC. Drug Kit B was partially available at all sub-centers of all six PHCs. Contraceptive Nirodh and oral pills were available at 18(58.06%) sub centers whereas Copper T was available at only 8(25.80%) sub centers. Emergency contraceptive pills were not available at any sub-centre. Toilet facility was not available at twenty nine sub-centers (93.54%).
Discussion
MCH and Family Planning services like Ante-natal , intra-natal, post-natal, new born and child care including immunization, contraception, adolescent health care, assistance to school health services, Janani Suraksha Yojana, treatment of minor ailments and First aid services were available at all Sub-centers. All sub-centers of six PHCs were existed in designated government building except three sub-centers (09.67%) which are existed on shared basis with Anganwadi, Zilla parishad and one SC was on rent basis whereas Khan M.E et al. (1999)[6] in a situation analysis report of Sitapur district done in 1999 in five block level PHCs found that
out of 54 sub-centers only a few sub-centers were situated in government- owned buildings whereas most of the sub-centers were functioning in a small room with no electricity or toilet facilities.
Toilet facility was not available at twenty nine sub-centers (93.54%), the same findings are noted in Social Audit in NRHM (2007)[7] where not all of the centers are running in a Pakka Makan (brick houses) and most of the centre do not have toilet facility.
At fifteen sub-centers (48.38%) the ANM do not reside at the sub-centre staff quarters and at six sub-centers (37.5%) ANMs, who reside at subcentre Quarter, have occupied even the clinical space for their residential use. Kumar BL (1995) [8] in his study in Gujarat in 1995 has found that about 80% of the sub-centre staff does not stay at the headquarters.
Health Worker (female) was available at all the 31 sub-centers, whereas Health Worker (male) was not available at any of the sub-centers. Voluntary worker to keep the Sub-Centre clean and assisting ANM was not available at sixteen sub-centers (51.61%).but Social Audit in NRHM (2007) [7] revealed that not every Sub-centre has a female health worker.
Furniture availability at sub-centers of Giroli PHC was (52%) followed by Deoli PHC (48%), Waifad PHC (48%), Nachangaon PHC (40%), Vijaygopal PHC (36%) and Gaul PHC (32%).But Foo and Gillian H.C.(1996)[9] in his report on the furniture in four states reported that examination table, chairs for clients, benches for waiting patients were available in all the sub-centers of the states of West Bengal, Bihar, Tamil Nadu and Karnataka.
Equipments available at Sub-centers of five PHCs were between 49-52% except at sub-centers of Deoli PHCs where availability is (41.81%) Agrawal Monica et al (2001) [10] in a study in Lucknow stated that all the centers were well equipped whereas Ramana GNV, Devi R, Praksamma et al (1995) [11] in a baseline survey in Shamirpet PHC of Andhra Pradesh in 1995, it was found that many health workers lacked Stethoscopes, Blood Pressure cuffs or both because of which BP was generally not checked at the subcenters. Weighing scale, examination table and chairs for clients, benches for waiting patients were also not available. Drugs Kit A was available at (83.33%) sub-centers of Giroli and Gaul PHC; (66.66%) of Waifad PHC; (50%) subcenters of Vijaygopal, Deoli and Nachangaon PHC whereas Drug Kit B was partially available at all sub-centers of six PHCs. Gandotra et al (1997)[12] in a case study from Gujrat reported that all sub-centers were always short of medicines and contraceptives. Population Council, Sitapur Report (1995) [5] stated that Autoclaves and sterilizers were seen in 12% of the subcenters whereas examination table, stethoscope, and weighing scale were available at only 5-25% sub-centers It is concluded that majority of subcenters fall short of IPHS expectations. Paramedical staff, basic equipments, furniture, drugs and Infrastructure are inadequate whereas facilities for sanitation and cleanliness are lacking at many centers and where it is present was not up to the mark and satisfactory.
Conclusion and Recommendations
? Hence balancing Infrastructure, pooling resources, Intersectoral Coordination, optimization of health manpower, decentralization of health programmes is necessary to fulfill the criteria of IPHS of sub-centers in each Block.
? Recruitment or contractual appointment of sub-center staff has to be done
? All the Sub-centers should run in government-owned building with adequate space, Drugs, Equipments and furniture should be provided.
? Every centre should maintained cleanliness specially toilets.
? Improvement in drug supply chain is extremely important to improve extent of utilization of services.

References:
1. Kleczkowski, B.M. „ Health care facilities in developing countries? WHO Chronicle 30: 363-9, September 1976.
2. WHO (1978) Health for All Sr.No.1.
3. Indian Public Health Standards (IPHS) for Sub-centre, Director General of Health Services, Ministry of Health and Family Welfare, Government of India, February, 2007
4. Mission Document, National Rural Health Mission, Ministry of Health and family Welfare, Government of India, April, 2005
5. Population Council, 1995. Situational analysis of Family Welfare Programme in Sitapur district of U.P., New Delhi: Population Council, New Delhi 1995
6. Khan M.E., Patel Bella C. and Gupta R.B., The Quality of Family Planning Services in Uttar Pradesh from the Perspective of Service Providers. : In Improving Quality of Care in India?s Family Welfare Programme edited by Micheal A., Koenig and M.E.Khan. Population Council, 1999; p.238-269
7. Social Audit of NRHM in two states, Empowering the poor for claiming their health rights, a report of Utter Pradesh and Uttarkhand, Centre for Health and Social justice-New Delhi,
8 August 2007 8. Kumar BL. Primary Health Care in Gujrat: Evidence on Utilization, Mismatches and Wastage; GIDR Working Paper No: 149, October 2004
9. Foo, Gillian H-C. A synthesis of research finding on quality of service in Indian Family Welfare Programme, Proceedings from a National Workshop on Operational Research for improving quality of services. Bangalore, Karnataka; 1996
10. Ranjeeta Kumari, MZ Idris, Viddya Bhushan and et al; Study on patient satisfaction in the government allopathic health facilities of Lucknow district: Indian Journal of Community Medicine; Volume: 34; Issue:1; Year: 2009; Page: 35-42
11. Ramana GNV, Devi R, Praksamma et al (1995) Improving Quality of care at Shamirpet Primary Health Center, Andhra Pradesh, Population Manager, Vol.5, 1997
12. Gandotra MM, Khan ME, Shah U et al. Quality of Family Welfare services in India: A case study of Gujarat Population Research Center, Baroda and Population Council, New Delhi, 1997
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License