IJCRR - 3(1), January, 2011
Pages: 28-38
Print Article
Download XML Download PDF
SELF EMULSIFYING FORMULATION, PLATFORM FOR SOLUBILITY ENHANCEMENT: A REVIEW
Author: Panner Selvam R, Kulkarni P.K, Mudit Dixit
Category: Healthcare
Abstract:Poor drug solubility remains a significant and frequently encountered problem for pharmaceutical scientists. Lipid formulations are one of the approach to enhance rate and extent of oral absorption for poor drug soluble drugs, because along with drug solubility it enhances drug permeability. Self emulsifying drug delivery system (SEDDS) composed of oils, surfactants and cosolvents which emulsify under conditions of gentle agitation, similar to those which would be encountered in the gastro-intestinal tract. But the solubility of the drugs in these medium and
the proportion of ingredients taken are the most important criteria to have a proper, stable SEDDS. Thus, only very specific pharmaceutical excipients combinations will lead to efficient self-emulsifying systems. This review provides a comprehensive summary of the mechanism, development, characterization of SEDDS. SEDDS appears to be a unique and industrially feasible approach to overcome the problem of low oral bioavailability associated with the lipophillic drugs.
Keywords: Self emulsifying drug delivery system, surfactants, bioavailability.
Full Text:
INTRODUCTION
Although oral delivery is the most preferred method of drug administration, this is not possible for roughly 50% of currently marketed drug compounds due to their low solubility in water and low oral bioavailability1,2. In drug discovery, about 40% of new drug candidates display low solubility in water, which leads to poor bioavailability, high intrasubject/intersubject variability and lack of dose proportionality3,4. Thus, for such compounds, the absorption rate from the gastrointestinal (GI) lumen is controlled by dissolution5 .There are various techniques available to improve the solubility of poorly soluble drugs6,7. Self-emulsifying drug delivery systems (SEDDS) are mixtures of oils and surfactants, ideally isotropic, and sometimes containing co-solvents, which emulsify spontaneously to produce fine oil in-water emulsions when introduced into aqueous phase under gentle agitation8,9 . Therefore, an SEDDS can be an efficient vehicle for class II to IV molecules of the Biopharmaceutical Classification System (BCS) drugs10. Currently the market value of the lipid formulation comprises an estimated 2-4% of the commercially available drug products surveyed in three markets (UK- 2%, US- 3%, and Japan- 4%) worldwide11, 12. The concept of using these systems for pharmaceutical purpose was initially developed by group of Groves. Therefore aspect of formulation of the SEDDS is to improve the bioavailability of the pharmaceutical product13. In this article SEDDS is a general name that includes all self-emulsifying formulations regardless of size.
LIPID FORMULATION CLASSIFICATION SYSTEM (LFCS) 14, 15
LFCS was established by Pouton in 2000 and recently updated in 2006 to help stratify formulations into those with similar component parts. The LFCS briefly classifies lipid-based formulations into four types according to their composition and the possible effect of dilution and digestion on their ability to prevent drug precipitation and they are shown in Table I. Type I are Nondispersing systems, Type II lipid formulations, referred as a self-emulsifying drug delivery systems, Type III lipid-based formulations, commonly referred to as selfmicroemulsifying drug delivery systems. Type IV is dispersion systems: non-oil micellar Systems.

ADVANTAGES 16-20
1. Fine oil droplets formed will pass rapidly from the stomach and promote wide distribution of the drug throughout the GI tract, thereby reduces the irritation.
2. Bioavailability enhancement results from the increased surface area by finely dispersed state of the drug containing lipid globules which leads to increased dissolution. The emulsion globules are further solubilized in the gastrointestinal tract by bile fluids. The surfactants in the formulations enhance absorption by membrane induced permeation changes. The droplets formed are either positively charged or negatively charged. A cationic emulsion has greater bioavailability than an anionic emulsion. As the mucosal lining is negatively charged it was observed that positively charged particles penetrated deeper into the ileum.
3. Enhanced oral bioavailability enabling reduction in dose.
4. More consistent temporal profiles of drug absorption.
5. Selective targeting of drug(s) toward specific absorption window in GIT.
6. Protection of drug(s) from the hostile environment in gut
. 7. Control of delivery profiles.
8. Protective of sensitive drug substances.
9. High drug payloads.
10. Solid, semisolid or liquid dosage forms.
11. Thermodynamically stable when compared to the simple emulsions.
DISADVANTAGES
The main drawbacks of this system include chemical instabilities of drugs and high surfactant concentrations. The large quantity of surfactant in self-emulsifying formulations (30-60%) irritates GIT. Consequently, the safety aspect of the surfactant vehicle had to be considered. Moreover, volatile cosolvents in the conventional self-emulsifying formulations are known to migrate into the shells of soft or hard gelatin capsules, resulting in the precipitation of the lipophilic drugs 21 . One of the another obstacles for the development of SEDDS is the lack of good predicative in vitro models for assessment of the formulations 22-25 .
MECHANISM OF SELF EMULSIFICATION
There are many mechanisms proposed in emulsion formation, are as follows Self emulsifying process are related to the free energy, ΔG given by
ΔG = Σ N π r2 σ
Here, N is the number of droplets with radius r and σ the interfacial energy 26. It is clear from the equation that the spontaneous formation of interface between the oil and water phase is energetically not favorable. The system commonly classified as SEDDS have not yet been shown to emulsify spontaneously in the thermodynamic sense. Mustafa and Groves developed a method using phosphated nonylphenoloxylate (PNE) and phosphated fatty alcohol ethoxylate (PFE) in n?hexane. The results suggested that the emulsification process may be associated with the ease with which water penetrates the oil?water interface, with formation of liquid crystalline phase resulting in swelling at the interface, thereby resulting in greater ease of emulsification27 . Consequently, the authors were able to relate the phase behavior to the spontaneity of emulsification, with liquid crystals formation, tending to form emulsion more readily, as indicated by the lower equilibration times28 . Pouton has argued that the emulsification properties of the surfactant may be related to phase inversion behaviour of the system29 . For example, if one increases the temperature of the oil in the water system stabilized by using non?ionic surfactants, the cloud point of the surfactant will be reached followed by phase inversion30. Pouton has suggested that the specificity of surfactant combination required to allow spontaneous emulsification is associated with a minimization of phase inversion temperature, there by increasing the ease of emulsification29
FORMULATION ASPECTS
Ideal properties of drug:
The poorly soluble drugs having high/low permeability, in association with low melting point, critical stability, and low dose (highly potent) are suitable candidates31, 32 .
Composition of SEDDS:
1. Oil: Both long and medium-chain triglyceride (MCT) oils with different degrees of saturation have been used for the design of SEDDS. Unmodified edible oils provide the most ?natural' basis for lipid vehicles, but their poor ability to dissolve large amounts of hydrophobic drugs and their relative difficulty in efficient self emulsification33, 34. MCT were preferred in the earlier SEDDS because of its higher fluidity, better solubility properties and self emulsification ability, but evidently, they are considered less attractive compared to the novel semi-synthetic medium chain derivatives which can be defined rather asamphiphilic compounds exhibiting surfactant properties. Polyglycolyzed glycerides (PGG) with varying fatty acid and polyethylene glycol (PEG) chain lengths giving them a varied hydrophile-lipophile balance (HLB) value, in combination with vegetable oils have been used to solubilise poorly water-soluble drugs and improve their bioavailability35 .
2. Surfactants: Non-ionic surfactants with a relatively high hydrophilic lipophilic balance (HLB) were advocated for the design of self dispersing systems, where the various liquid or solid ethoxylated polyglycolyzed glycerides and Tween 80 are the most frequently used excipients. Nonionic surfactants are known to be less toxic compared to ionic surface-active agents, but they may cause moderate reversible changes in intestinal wall permeability. The usual surfactant concentration in self-emulsifying formulations required to form and maintain an emulsion state in the GI tract ranged from 30 to 60% w/w of the formulation36 .
3. Co-solvents: Organic solvents, suitable for oral administration (ethanol, propylene glycol (PG), polyethylene glycol etc. may help to dissolve large amounts of either the hydrophilic surfactant or the drug in the lipid base37 . Example: Co-solvents like diethylene glycol monoethyl ether(transcutol), propylene glycol, polyethylene glycol, polyoxyethylene, propylene carbonate, tetrahydrofurfuryl alcohol polyethylene glycol ether (glycofurol) etc38
4. Consistency builder: Additional material can be added to alter the consistency of the emulsions; such materials include tragacanth, cetyl alcohol, stearic acids and /or beeswax. 5. Polymers: Inert polymer matrix representing from 5 to 40% of composition relative to the weight, which is not ionizable at physiological pH and being capable of forming matrix are used. Examples are hydroxy propyl methyl cellulose, ethyl cellulose, etc39
SOLIDIFICATION TECHNIQUES40, 41
Spray cooling, Spray drying, Adsorption to solid carriers, Melt granulation, Melt extrusion/extrusion spheronization, Supercritical fluid based methods, Solid lipid nanoparticles (SLN) and Nanostructured lipid carriers (NLC)
DOSAGE FORM DEVELOPMENT OF S-SEDDS42
Dry emulsions, Self-emulsifying capsules, Self-emulsifying sustained/controlledrelease pellets Self-emulsifying sustained/controlledrelease tablets, Self-emulsifying solid dispersions Self-emulsifying beads, Self-emulsifying sustained-release microspheres, Selfemulsifying nanoparticles, Self-emulsifying suppositories, Self-emulsifying implants
TERNARY DIAGRAM 43, 44
This technique was mainly used to map the micro emulsion areas (composition ranges). Ternary phase diagram is used to map the optimal composition range for three key excipients according to the resulting droplet size following self emulsification, stability upon dilution and viscosity.
CONSTRUCTION OF PHASE DIAGRAM 43, 44
A Titration method is employed to construct phase diagram. Mixture of oil with surfactant is prepared at different ratios (e.g. 10:0, 9:1, 8:2, 7:3,6:4, 5:5, 4:6, 3:7, 2:8, 1:9, 0:10) into different vials. A small amount of water in 5 % (w /w) increments is added into the vials. Following each water addition the mixture in vials is centrifuged for 2 to 3 minute and is incubated at 25?c for 48 hrs with gentle shaking. The resulting mixture is evaluated by visual and microscopy observation. For phase diagram the micro emulsion is the region of clear and isotropic solution. Coarse emulsion is the region of cloudy dispersion.
EVALUATION PARAMETERS
Turbid metric evaluation:
Nepheloturbidimetric evaluation was done to monitor the growth of emulsification. Self-emulsifying system was added to 0.1N hydrochloric acids under continuous stirring on magnetic plate at ambient temperature, and the increase in turbidity was measured using a turbid meter45, 46 .
Viscosity determination: Viscosities of the systems as such and after dilution with 5% v/v water were determined using Brookfield rheometer at ambient temperature. Under varying shear rate, viscosities were measured and the data obtained were further analyzed by regression treatments47 .
Droplet size analysis or particle size measurements: The droplet size of the emulsions is determined by microscopic techniques or Coulter Nanosizer or photon correlation spectroscopy 48. The nanometric size range of the particle is retained even after 100 times dilution with water which proves the system's compatibility with excess water49 .
Droplet polarity: Polarity of oil droplets is governed by the HLB value of oil, chain length and degree of unsaturation of the fatty acids, the molecular weight of the hydrophilic portion and concentration of the emulsifier. Polarity of the oil droplets is also estimated by the oil/water partition coefficient of the lipophillic drug50 .
Electrical Conductivity Measurement: Electrical conductivity of the samples was measured using a conductivity meter. Electrical conductivity of the formulations was determined to check the stability and assert the nature of the formulation51 .
Refractive index and percent transmission: Refractive index and percent transmittance proves the transparency of formulation. The refractive index of the system is measured by refractometer by placing drop of solution on slide and it is compared with water. If refractive index of system is similar to the refractive index of water and formulation has percent transmittance > 99 percent then formulation has transparent nature 52 .
Centrifugation: Microemulsion systems were subjected to centrifugation at 3000 rpm for 30 minutes and then examined for any phase separation This technique helps to determine behaviour of small particles in gravitational field53 .
Differential scanning calorimetry (DSC): Physical state of the drug in lipid carrier was analyze by DSC studies. Thermal analysis of drug, the physical mixture of drug and Lipid carrier were carried out using differential scanning calorimetry method54 .
X-ray diffraction studies:X-ray diffraction studies analyze the crystalline nature of the drug in the mixture. X-ray diffraction was performed using a diffractometer, with a monochromatics radiation having suitable voltage and current at an angle of 2θ over a range of 5 40. Diffraction patterns of pure drug and Lipid carrier were prepared at the suitable drug-to-lipid ratio for the determination55 .
In vitro diffusion study: In vitro diffusion studies were performed using dialysis technique/Dissolution apparatus56
Drug content: Drug from pre-weighed SEDDS is extracted by dissolving in suitable solvent. Drug content in the solvent extract was analyzed by suitable analytical method against the standard solvent solution of drug.
In vivo Characterization includes Nonclinical Evaluation, Choice of nonhuman Test Species, Lymphatic Transport57 .
CONCLUSION
Approximately 40% of new chemical drug moieties have poor aqueous solubility and it is a major challenge to modern drug delivery system. Self emulsifying drug delivery system are suited for BCS class 2 and class 4 drugs. The proper selection of the oil and surfactants are most important for successful development of SEDDS. Solidification techniques enhances the stability and easy handling. By exploiting studies about human bioavailability and in vitro methods for predicting the dynamic changes involving the drug in the gut in order to monitor the solubilisation state of the drug in vivo, open the gateway for the many drugs to enter market as SEDDS
References:
1. Humberstone AJ, Charman WN. Lipidbased vehicles for the oral delivery of poorly water soluble drugs. Adv Drug Deliv Rev 1997;25(1):103-28.
2. Gursoy RN, Benita S. Self-emulsifying drug delivery systems (SEDDS) for improved oral delivery of lipophilic drugs. Biomed Pharmacother 2004;58(3):173-82.
3. Lipinski C. Poor aqueous solubility-an industry wide problem in drug discovery. Am Pharm Rev 2002;5:82-5.
4. Palmer AM. New horizons in drug metabolism, pharmacokinetics and drug discovery. Drug News Perspect 2003;16:57-62.
5. Amidon GL, Lennernas H, Shah VP, Crison JR. A theoretical basis for a biopharmaceutical drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res 1995;12:413-20.
6. Pinnamaneni S, Das NG, Das SK. Formulation approaches for orally administered poorly soluble drugs. Pharmazie 2002;57:291-300.
7. Kulkarni PK, Dixit M, Kini AG, Johri A. Spherical agglomerates of mefenamic acid by solvent change method. An int j pharma sci 2010;1:388-402,.
8. Wakerly MG, Pouton CW, Meakin BJ, Morton FS. Self-emulsification of vegetable oil-non-ionic surfactant mixtures. ACS Symp Ser 1986;311:242-55.
9. Sachan R, Khatri K, Kasture S. SelfEumlsifying Drug Delivery System: A Novel Approach for enhancement of Bioavalibility. Int J PharmTech Res 2010 July-Sept;2(3):1738-45,.
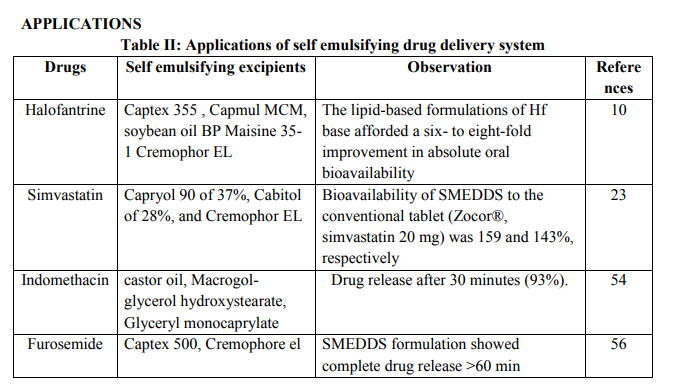
10. Khoo SM, Humberstone AJ, Porter CJH, Edward GA, Charman WN. Formulation Design and bioavailability assessment of lipidic self-emulsifying formulation of halofantrine. Int J Pharm 1998;167:155-64.
11. Strickley RG. Oral Lipid-based Formulations: Enhancing the Bioavailability of Poorly Water-soluble Drugs. New York: Informa Healthcare; 2007, pp.221-238.
12. Strickley RG. Solubilizing excipients in oral and injectable formulations. Pharma Research 2004;2:201-30.
13. Patel MJ, Patel SS, Patel NM, Patel MM. A Self-Microemulsifying Drug Delivery System (Smedds). int J Pharma Sci Rev and Research 2010 October;4(3):29-35.
14. Pouton CW. Lipid formulations for oral administration of drugs: nonemulsifying, self-emulsifying and self microemulsifying drug delivery systems. Eur J Pharm Sci 2000;11: S93- 8.
15. Pouton CW. Self-emulsifying drug delivery systems: assessment of the efficiency of emulsification. Int J Pharm 1985;27:335-48.
16. Corbo DC, Liu JC, Chein YW. Characterization of the barrier properties of mucosal membranes. J Pharm Sci 1990;79:202-6
. 17. Gershanik T, Haltner E, Lehr CM, Benita S. Charge dependent interaction of self emulsifying oil formulation with CaCo-2 cell monolayers; binding effects on barrier function and cytotoxicity. Int J Pharm 2000;211(1- 2),29-36.
18. Gershanik T, Benzeno S, Benita S. Interactions of the SELDDS with mucosa of everted rat intestine as a function charge and particle size. Phar Res 1998;15:863-9.
19. Patil P, Joshi J, paradkar P. Effect of formulation variables on preparation and evaluation of gelled selfemulsifying drug delivery system(SEDDS)of ketoprofen. AAPS Pharm Sci Tech 2004;5(3):34-42 .
20. Pouton CW, Charman WN. The potential of oily formulations for drug delivery to the gastro-intestinal tract. Adv Drug Deliv Rev 1997;25:1-2.
21. Pathak A, Jain V, Nagariya AK, Singh R, Nayak S, Bansal P, Gupta V, Kumar S, Singh H. Recent advances in self emulsifying drug delivery system - A review. Drug Invention Today 2010;2(2):123-9.
22. Tang JL, Sun J, Guihe Z. SelfEmulsifying Drug Delivery Systems: Strategy for Improving Oral Delivery of Poorly Soluble Drug, Current Drug Therapy 2007;2:85-93.
23. Patil P, Patil V, Paradkar A. Formulation of a self-emulsifying system for oral delivery of simvastatin: In vitro and in vivo evaluation: Acta Pharm 2007;57:111-22.
24. Tang B, Cheng G, Chun J. Development of solid self emulsifying drug delivery systems, preparation techniques and dosage forms: Drug Discovery Today 2008;13:606-11.
25. Zhang P, Liu Y, Xu J. Preparation and Evaluation of SEEDS. Int J Pharm 2008;355:269-76.
26. Reiss H. Entropy-induced dispersion of bulk liquid. Journal of colloidal interface Sciences 1975;53:61?70.
27. Groves MJ, Mustafa RMA. Measurement of -spontaneity? of self emulsifiable oils. J Pharm Pharmacol 1974;26:671?88.
28. Groves MJ, Mustafa RMA, Carless JE. Phase studies of mixed surfactants nhexane and water. J Pharm Pharmacol 1974;26:616-23.
29. Pouton CW. Formulation of selfemulsifying drug delivery system. Adv Drug Del Rev 1997;25:47-58.
30. Friedman D. Non-aqueous compositions for oral delivery of insoluble bioactive agents. US Patent 20070190080. 2005 july 21.
31. Charman SA, Charman WN, Rogge MC. Self-emulsifying drug delivery systems: formulation and biopharmaceutic evaluation of an investigational lipophilic compound. Pharmacy Research 1992;9:87-93.
32. Serajuddin ATM. Solid dispersion of poorly water- soluble drug: early promises, subsequent problems, and recent breakthroughs. J Pharma Sci 1999;88:1058-66.
33. Gershanik T, Benita S. Self-dispersing lipid formulations for improving oral absorption of lipophilic drugs: Euro J Pharm Biopharm 2000;50:179-88.
34. Aungst BJ. Novel formulation strategies for improving oral bioavailability of drugs with poor membrane permeation or presystemic metabolism. J Pharm Sci 1993;82:979- 86.
35. Tang JL, Sun J, He ZG. SelfEmulsifying Drug Delivery Systems: Strategy for Improving Oral Delivery of Poorly Soluble Drugs. Curr Drug Theraphy 2007;2:85-93.
36. Aungst BJ. Novel formulation strategies for improving oral bioavailability of drugs with poor membrane permeation or presystemic metabolism: J Pharm Sci 1993;82:979- 86.
37. Wakerly MG, Pouton CW, Meakin BJ, Morton FS. Self emulsification of vegetable oil-nonionic surfactant mixtures: ACS Symp Ser 1986;311:242-55.
38. Dey P, Maiti S, Ray S, Sa B, Sen K. Self-Emulsification of Poorly Soluble and Highly Permeable Drugs: An Overview Int J Pharma Recent Res 2009;1(1):67-72.
39. Roop NG, Rakesh G, Singh RG. Enhancement of oral bioavailability of lipophillic drugs from selfmicroemulsifying drug delivery system (smedds). Int J Drug Dev and Res 2009 sep-dec;1(1):10-18
. 40. Katteboinaa S, Chandrasekhar VSRP, Balaji S. Approaches for the development of solid self-emulsifying drug delivery systems and dosage forms. Asian Journal of Pharmaceutical Sciences 2009;4(4):240-53.
41. Jannin, Musakhanian J, Marchaud D. Approaches for the development of solid and semi-solid lipid-based formulations. V. Advanced Drug Delivery Reviews 2008;60:734-46.
42. Tang B, Cheng G, Gu JC, Xu CH. Development of solid self-emulsifying drug delivery systems: preparation techniques and dosage forms. Drug Discovery Today 2008 July; 13(13/14):606-12.
43. Kamble VA, Jagdale DM, Kadam VJ. Self micro emulsifying drug delivery system. Int J Pharma and Bio Sci 2010;1(2):1-9
44. Abdulkarim MF, Abdullah GZ, Sakeena MHF, Chitneni M, Mun F, Yam et al. Study of Pseudoternary Phase Diagram Behaviour and the Effect of Several Tweens and Spans on Palm Oil Esters Characteristics. Int J Drug Deliv 2010;3:95-100.
45. Paul BK, Moulik SP. Microemulsion: An overview. Disp Sci 1997;18:301- 367
. 46. Maulik SP, Paul BK. Structure dynamics and transport properties of microemulsion. Adv Coll Int Sci 1998;78:99-199.
47. Patel SN, Patel DM, Patel CN, Patel TD, Prajapati PH, Parikh BN. Self emulsifying drug delivery system. Journal of Global Pharma Technology 2010;2(2):29-37
48. Joshi P, Patil P. Effect of Formulation Variables on Preparation and Evaluation of Gelled Self-emulsifying Drug Delivery System (SEEDS) of Ketoprofen. AAPS PharmSciTech 2004;5(3):5-8.
49. Nidhi M, Shikha S. New Strategy for Solubilization of poorly soluble drugSEDDS. Der Pharmacia Lettre 2009;1(2):60-67.
50. Shah NH, Carvajal MT, Patel CI, Infeld NH, Malick AW. Self-emulsifying drug delivery systems (SEDDS) with polyglycolyzed glycerides for improving in vitro dissolution and oral absorption of lipophillic drugs. Int J Pharm 1994;106:15-23.
51. Mustafa G, Khan ZI, Bansal T, Talegaonkar S. Preparation and Characterization of Oil in Water NanoReservoir Systems for Improved Oral Delivery of Atorvastatin. Current Nanoscience 2009;5:428-40.
52. Craig DQM, Barker SA, Banning D, Booth SW. An investigation into the mechanisms of self-emulsification using particle size analysis and low frequency dielectric spectroscopy. Int J Pharm 1995;114:103-10.
53. Jadhav KR, Shetye SL, Kadam VJ. Design and Evaluation of Microemulsion Based Drug Delivery System. Int J Adv Pharma Sci 2010;1:156-6
54. Taha EI. Development and Characterization of New Indomethacin Self-Nanoemulsifying Formulations. Sci Pharm 2009;77:443-51
. 55. Shaji J, Jadhav D. Statistical development and optimization of solid dispersion self emulsifying pellets. Int J Pharma Sci Rev and Res 2010 September - October;4(3):156-167.
56. Deshmukh A, Nakhat P, Yeole P. Formulation and in-vitro evaluation of self microemulsifying drug delivery system (SMEDDS) of Furosemide. Der Pharmacia Lettre, 2010;2(2):94-106.
57. Patro MN, Bankar AS, Rakesh SU, Yadav AV. Oral lipid based formulation: a review. Int J Pharma and Bio Sci 2010;1(2):1-14.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License