IJCRR - 3(7), July, 2011
Pages: 61-69
Print Article
Download XML Download PDF
HEALTH SEEKING BEHAVIOR OF HIV POSITIVE PATIENTS ATTENDING VOLUNTARY COUNSELING AND TESTING CENTER - A GENDER PERSPECTIVE
Author: Shaikh Mohsin, Patil Rajkumar, Pathan Sameer
Category: Healthcare
Abstract:The epidemic of Acquired Immuno Deficiency Syndrome (AIDS) has emerged as a serious public healthproblem in many parts of the world and a gender based difference in the health seeking behavior has significantly precipitated to it. Aims: To study the health seeking behavior of HIV positive cases and impact of gender discrimination over it. Settings and Design: It is a cross sectional study conducted in Voluntary Counseling and Testing Center (VCTC) \? Baroda. Methods: A semi-structured and pretested proforma was used to interview HIV positive patients attending VCTC located at Sayaji Hospital, Vadodara. With the help of VCTC counselors, In-depth interview of all patients were arranged to collect the detailed information on health seeking behavior. Prior verbal and written consent was taken before starting each interview. This study included 100 HIV positive cases (>13years) attending VCTC during April-December 2007. Results: The present study included 100 individuals with equal ratio of male and female, 73 % were in age group 21-40 years, 92% were literate and 60 % were married. 54 % patients consulted private clinic for their health problem while 30 % went to government hospital of which
majority were females (70 %). None of the female patients contacted VCTC initially for counseling purpose, while 13 % patients didn't consult any health care providers before reaching VCTC. 54 % patients consulted private GP initially of which 21 % didn't satisfied and visited Government hospital later. Over all 48 % patients reached SSG hospital and were referred to skin, TB, urology and general medicine before reaching VCTC.
Keywords: Study of gender based health behavior is the vital link to control the spread of HIV. The need of the hour is to strengthen the health services with the focus of gender.
Full Text:
INTRODUCTION
The epidemic of Human Immunodeficiency Virus (HIV) infection that causes Acquired Immuno-Deficiency Syndrome (AIDS) has emerged as a serious public health problem in many parts of the world. Estimates at the end of 2006 suggest that 39.5 million men, women and children are living with HIV/AIDS worldwide and almost 22 million have already lost their lives1 . In sub-Saharan Africa, young women (aged 15-24 years) are infected more frequently than young men. In 2001, the estimated infection rates for young women were 6-11% compared to 3- 6% for young men1 Focus of Gender in HIV/AIDS: Of the 37.2 million adults living with HIV/AIDS at the end of 2006, 17.7 million or nearly 50 percent were women2 . Rather than representing equity between the sexes, the one-to-one ratio of male to female HIV infections demonstrates the way in which gender inequalities affect HIV/AIDS incidence rates. Since the HIV/AIDS pandemic began more than 20 years ago, infection rates among women have accelerated. Traditional gender roles held by many of the world‘s societies definitely affects the health seeking behavior of women, which continued spread of HIV, particularly from men to women. In most societies, women also carry a disproportionate amount of the burden of caring for family members living with HIV/AIDS, and experience the brunt of the stigma associated with HIV infection. Correcting the gender imbalance that contributes to and is exacerbated by the HIV/AIDS pandemic will depend upon improving women‘s social and economic status, and increasing men's responsibility for HIV prevention and care, so as to provide better health care access. Unequal social roles and vulnerability to men‘s demands prevent women to have better health care access. Number of facts associated with HIV transmission like illiteracy, employment, gender discrimination poor health infrastructure etc., stimulates already prevalent stigma related to HIV/AIDS. Finally all these factors such as gender roles, economic, cultural and social factors and stigma related to HIV/AIDS are likely to influence the motivation of HIV infected people to practice safer sex3 . United Nations for HIV/AIDS has reported 5.7 million people in India with HIV/AIDS this year, which is almost 15 % of the global burden of HIV/AIDS, and 37 % of all the infected people in India are women4 . Nash Ojanuga and Gilbert (1992) systematized the obstacles which women face into four categories5 : 1.Institutional barriers: unequal treatment by health providers, 2. Economic barriers: different access to resources, 3.Cultural barriers: social status of women which situates them in socially inferior positions, 4. Education barriers: women having less access to education.
Objective: To study the health seeking behavior of HIV positive cases and impact of gender discrimination over it.
Need of the study
Women are most vulnerable and likely to get discriminated with HIV infection, having so many reasons in the background than men who plays dominant bread earner role in the society, there was a need of gender based research to go through the health seeking behavior of the HIV positive patients to understand the discrimination. It would also help in policy designing for national AIDS control Program.
METHODOLOGY
This is VCTC based cross sectional study consisting of qualitative data collection of HIV positive patients conducted between April ‘07 to December ‘07. Total number of 50 male and 50 female HIV positive patients who visited VCTC, Vadodara during the study period in age group >13 years were purposively selected for this research. The following selected criteria was adopted for inclusion of HIV positive patients attending VCTC in this research, 1) 50 adult male and 50 adult female >13 years of age. 2) HIV positive patients diagnosed minimum 2 months back. 3) Patient who voluntarily took part in the research and visited VCTC – SSGH after HIV infection. 4) Patients with HIV antibody test positive according to NACO guidelines6 . (ELISA and Rapid test). Information on Health seeking behavior and access to health care of HIV positive patient was collected through semi-structured, pre-designed and pre-tested proforma following in-depth. interview technique with the help of health seeking behavior pathway (Annexure). In-depth interview of each and every HIV positive patient was done with the help of expert VCTC counselors, through previously prepared questionnaire at VCTC in a private room with prior informed, written and verbal consent. Proper care has been taken to maintain the confidentiality. Prior permission from the Ethical committee of the university has been taken to carry out whole research. Analysis of the study was done using Epi Info 6.04 d Statistical Package and Chi square test was applied wherever needed. Following steps were involved in documentation and data management after data collection.
Limitations of study:
We could have been covered VCTCs of Gujarat but we didn‘t get the permission to do so and also could have consulted the other high risk groups like male and female sex workers, homosexual group, or truck drivers to understand their health seeking behavior.
RESULTS
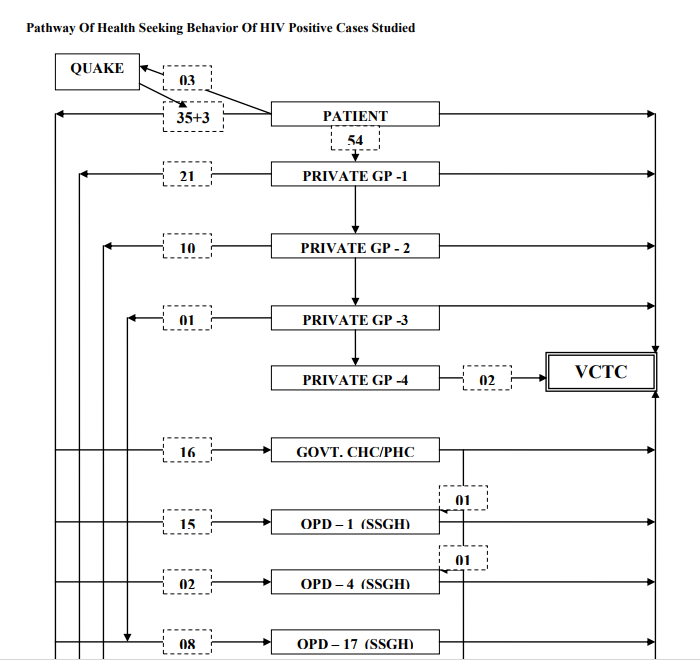
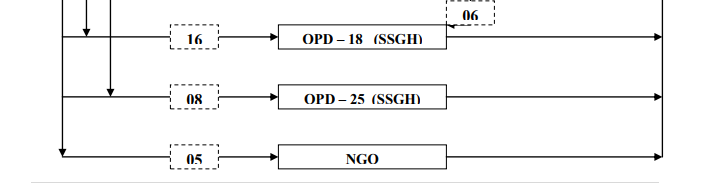
The study included 50 male and 50 female HIV positive (diagnosed minimum 2 months back) cases who visited VCTC. Over two third of the patients (73%) were within 21-40 years of age group among both the genders. Almost 60 % of HIV positive patients were married with significantly higher percentage of males (58 %) as compared to females (42 %). Whereas total number of widow/widower found is 23 % and more than two third of them were females as compared to males. Majority of female patients (80 %) were housewives while majority of males were involved in high risk occupations like truck driving, auto driving, call center job and sales work. Of total patients, 8 % were illiterate, 43 % patients were educated upto 7th standard, 30 % untill 10th standard, 14 % untill 12th standard and only 5 % had studied untill graduation or higher; without much gender difference. Of the total economically self dependant patients (49%), more than two third were males. Out of total 66 % of patients, 42 % had TB infection in the past while 30 % had STD (with equal gender distribution) history. All HIV positive patients had undergone CD4 count testing of whom 49 % were females and 51 % were males (Table – 1). Out of 37 patients on ART, 78 % (n=29) cases experienced at least one ADR related to ART use. 86 % cases had history of ADR in the form of nausea, vomiting and in 31 % cases, in the form of skin reaction with no gender difference. Out of 100 patients, 8 directly went to VCTC without getting referred by anyone and all of them were males, while 62 % patients were referred to VCTC by Doctors ( Private and Government). 7 % patients were referred by the family members, 6 % by their friends, 5 % by NGOs and 9 % of patients by their relatives other than their family members. There was no statistically significant gender difference (Table 2). Table 2, shows the distribution of HIV positive patients by appearance of first sign/symptoms noticed by them when asked. HIV positive patients had history of single or multiple symptoms during initial health problems. Majority of patients observed weight loss (26 %) followed by fever (23 %), cough (22 %), skin problems (17 %), diarrhea (10 %), burning micturition (6 %) and genital ulcer (5 %). There is no statistically significant gender difference seen. 54 % patients initially contacted private clinic/hospital for their symptomatic problems of whom 59 % were males as compared to 41 % females. 30 % patients contacted government hospital initially and 70 % of them were females as compared to 30 % males, which is statistically significant (P3 health care providers before reaching VCTC. Out of 100 patients studied, 8 directly contacted VCTC voluntary bases immediately. 79 % patients had first health care contact within 6 months of observing first sign/symptom by themselves, while 13 % patients took >6 months to contact health care providers. There is no significant gender difference seen (Table-2). 13 % visited VCTC because of Tuberculosis infection, 10 % due to skin problems, 9 % cases visited VCTC because of their high risk behavior, 7 % gave a reason of their spouse being HIV positive, 4 % due to penile ulcer and same percentage of patients visited VCTC as a part of pre operative investigation. 2 % had pneumonia and were consulted VCTC for HIV testing while 2 % were consulted during visa procedure for HIV testing and others during ANC check-ups, for insurance purpose and some MSM behavior. 46 % patients gave a reason that they visited VCTC for other health problems like low grade fever, chronic cough, diarrhea and weight loss. According to health care seeking pathway, Initially 3 patients directly went to Quack with the hope of getting treated – but finally consulted GP/SSGH for their treatment. 8 Patients directly went to VCTC - Baroda for testing and for counseling purpose. 54 Patients directly went to Private General Practitioner out of which 9 patients changed GP for the 3rd time and 2 patients changed GP treatment for the 4th time and finally went to VCTC. 21 Patients who consulted private GP for the first time - were not satisfied and moved to SSG Hospital/Govt. CHC/PHC for further testing and treatment purpose. 38 Patients directly consulted SSGH/Govt. CHC/PHC without going to Private GP. 5 Patients went to NGO directly with their suspicion of having HIV infection and after counseling they were sent to VCTC. 16 patients consulted Govt. CHC/PHC of which 6 patients went to private GP for the first and then to Govt. CHC/PHC. 8 patients out of those 16 went to SSGH because of their unsatisfactory treatment and counseling, finally all were guided to VCTC. Over all 48 patients reached SSGH after consulting one or more GP of whom 15 patients reached OPD-1 (Skin and VD OPD) for skin lesions over body parts and private parts while 16 patients reached OPD-18 (General Medicine OPD) for their generalized health problems and 8 patients reached OPD-17 (TB and Chest diseases OPD) for their suspected koch‘s infection. 8 Patients consulted OPD-25 (Urology OPD) for suspected UTI and 2 patients visited OPD -4 (Orthopedic OPD) for their orthopedic problems.
CONCLUSION
Majority of male patients (59 %) had contacted private clinic/hospital initially for their health problems as compared to 41 % females because of fear of social stigma related to HIV/AIDS and belief of more privacy at private setup. Nearer to two third (70 %) female patients contacted government hospital initially for their problems as compared to 30 % males (P<0.05), as they could not afford to go to private hospital due to their economic dependency on others. 3 females were forced to contact quack for their health problems by their spouse. This was because of the male dominance to their decision where as female has to depend on others physically as well as economically. Almost 15 % cases contacted more than three health care providers as they were not improved and 13 % patients took more than 6 months to have first health care contact. 8 patients contacted VCTC directly and all of them were males, none of them were females.
A Study on Gender impact of HIV/AIDS in India shows that as compared to men, women have poorer access to healthcare. The financial constraint is also a big impediment for getting proper healthcare and it is more so for women7 . Women may be more affected by stigma and discrimination than men because of social norms concerning acceptable sexual behavior in women, and that‘s why women are often more economically vulnerable than men. Our study also reported higher number of economically vulnerable females. Gender differences in decision-making may also affect access to health facilities. For example, a study conducted in developing countries found that while men made independent decisions to seek voluntary counselling and testing services, women felt obliged to discuss testing with their partners before accessing the service5 . Another report by center for disease control and prevention shows that as far as possible, women would try to avoid going to the doctor, in particular, avoid getting hospitalized as the household routine is likely to be disrupted more by the sickness of women of the household. In households where both men and women are sick, more importance is given to get the man who is the breadwinner, the same may be the reason in our study as we found less number of women who accessed treatment.7
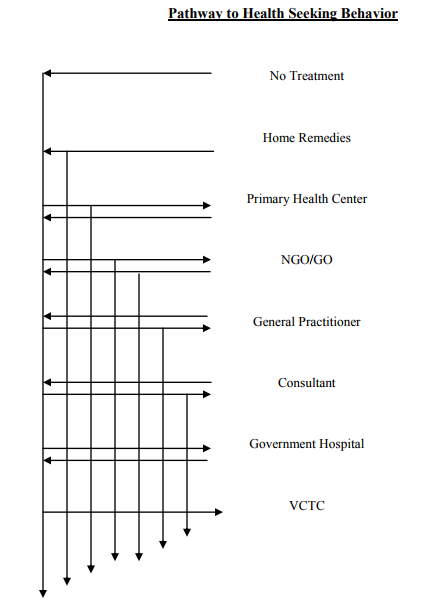
Patients visiting VCTC following different pathways for health care were evaluated through this flowchart. Whether they directly contacted VCTC without starting any treatment or contacted few health care providers before reaching VCTC (PHC MO / NGO / GO / Private Practitioner / Consultant / Government Hospital). The entire interview was focused and in depth.
Abbreviations:
ADR – Adverse Drug Reaction
AIDS – Acquired Immunodeficiency Syndrome
ANC- Ante Natal Care
ARV – Anti Retroviral Drug
ART – Anti Retroviral Therapy
FGD – Focal Group Discussion
GO – Government Organization
GP – General Practitioner
GSACS – Gujarat State AIDS Control Society
HIV – Human Immunodeficiency Virus
IDI – In-depth Interview
MO – Medical Officer
MSM- Men having sex with Men
NGO – Non Government Organization
OPD – Out Patient Department
PHC – Primary Health Centre
PLHIV – People living with HIV
SSGH – Sir Sayajirao General Hospital
STD – Sexually Transmitted Disease
STI – Sexually Transmitted Infection
TB – Tuberculosis UNAIDS – United Nations
UNDP – United Nations Development Program
UTI- Urinary Track Infection
VCTC – Voluntary Counseling and Testing Centre
VDRL – Venereal Disease Research Laboratory
WHO – World Health Organization
References:
1. Joint United Nations Programme on HIV/AIDS (UNAIDS) 2006, AIDS Epidemic Update (English original). Available at :http://www.unaids.org/ globalreport/documents/20101123_GlobalR eport_full_en.pdf. , Accessed on 1st January 2011.
2. Joint Unied Nations Programme on HIV/AIDS (UNAIDS) 2000. Men and AIDS: A Gendered Approach. Geneva: UNAIDS. Available at: www.thebody.com/ unaids/men/contents.html. Accessed on 1st August 2007.
3. Population Council (2007), ?Reducing HIV risk behaviors among key populations by Increasing community involvement and building social capital?. Available at: www.popcouncil.org, Accessed on 1st November 2007.
4. United Nations Program on HIV/AIDS (2007). www.unaids.org.in . Accessed on 10th January 2007
5. Ojanuga, D Nash, Gilbert., (1992). Women‘s access to health care in Developing countries. Social Science and Medicine Vl.35, August 1992:613.
6. National AIDS Control Organization (NACO), (2002), Specialist‘s Training and Reference Module. New Delhi.
7. Matlin, S. and Spence, N. (2001) "The Gender Aspects of the HIV/AIDS Epidemic." Presentation at the Expert Group Meeting on the HIV/AIDS Pandemic and Its Gender Implications, Windhoek, Namibia. Available at:www.un.org/womenwatch/daw/csw/hivai ds/matlinspence.html. Accessed on 10th January 2009.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License