IJCRR - 4(3), February, 2012
Pages: 59-69
Print Article
Download XML Download PDF
TREATMENT SEEKING BEHAVIOR OF MARRIED WOMEN OF REPRODUCTIVE AGE BELONGING TO A
RURAL COMMUNITY OF INDIA
Author: Mohammad Shakil Ahmad, Shaikh Mohsin, Ritu Kumar Ahmad
Category: Healthcare
Abstract:Background: India is a country of villages where 72.2% of the people live in the rural area and women of reproductive age group (15-49 years) constitutes 21% of the total population. Majority of the women suffer from morbidity due to obstetric and gynecological problems. Objectives:To know the health seeking behavior of a married women of reproductive age and to know the types of health services utilized by them. Methodology:It is one year community based cross sectional study. The study was conducted at Handignur PHC area in Belgaum district (India) from January 2007- December 2007, with a sample size of 732 (total number of all women in reproductive age group of selected villages under Handignur PHC area). All married women of reproductive age group were included in the study, and data was collected by administering pre designed and pre tested structured proforma. Data were analyzed using SPSS software. Results:The present study revealed that, 22.03% of the women were in the age group of 35-39 years. The literacy rate of the women was found to be 74.4%. The literacy rate of their husbands was found to be 82.4%. Joint family was the commonest being 81.28%. 71.3% of the women belonged to the category V of modified Prasad's group of socio economic status classification. All married women of reproductive age had the knowledge of the facilities available near their homes. 79.09% of the women preferred to go the PHC/ sub center for general health problems. 99.59% said it was easy accessibility. 92.49% said that they were satisfied by the treatment. In case of 75.18% of the study participants their husband's made decisions for them regarding their general health problems. For obstetrics care all 732 women preferred going to the PHC/ sub center. 39.34% said they made 1-2 visit for their ANC check up's. And to be noted that 21.03% of the women did not make a single visit as there was no PHC's/ sub center during the time of their pregnancy. 78.96% said they received iron and folic acid tablets during the time of their pregnancy. 54.78% women said the doctor provided it to them. 78.96% said they received injection tetanus toxoid injection during the time of their pregnancy. 66.12% said that they preferred the PHC/ sub center for the choice of place for getting delivered. 47.00% preferred the doctors conducting the deliveries. The choice of health facility opted for the gynecological problems; 81.42% said that they preferred the PHC/ sub center. 81.42% women said because it was near to thehouse, all necessary and emergency drugs were available and all facilities were provided. 46.17% of the women said it was their own decision. 91.25% women said they were practicing either temporary or the permanent methods or their husbands were using temporary methods of family planning. 61.07% women were using copper T as the methods of family planning. 61.07% women said the doctors at the PHC/ sub center helped them in providing them the family planning methods. 48.35% women said it was their husband's decisions in case of family planning. Conclusion: The participants had a fair knowledge regarding treatment seeking, the availability of health care services and the types of services offered. TREATMENT SEEKING BEHAVIOR OF MARRIED
WOMEN OF REPRODUCTIVE AGE BELONGING TO A RURAL COMMUNITY OF INDIA
Mohammad Shakil Ahmad1, Shaikh Mohsin1, Ritu Kumar Ahmad2
1College of Applied Medical Sciences, Qassim University, Saudi Arabia
2Chettinad Hospital and Research Institute, Kelambakkam, Chennai
E-mail of Corresponding Author: doc_shakmd@live.com
60 International Journal of Current Research and Review www.ijcrr.com
Vol. 04 issue 03 February 2012
The key decision maker for general health problems, obstetric health problems and for family planning
was the husbands, where as for the gynecological problems the majority of women made her own
decisions.
Keywords: Treatment seeking behavior, married women, reproductive age group, rural community
Full Text:
INTRODUCTION
Health seeking behaviour is a topic which has received considerable attention in recent years. The ?quest for therapy?, all over the world is an important research issue since it reveals essential elements of people‘s social behavior and provides insight into their perceived needs for different kinds of health services. The community diagnosis is the starting point for local health planning - at least in theory- and the study of how people use health care facilities is an important component of it.1 Health care delivery in developing countries have been typically described in terms of insufficient medical and paramedical staff, unequal access to services, emigration of qualified personnel to jobs in other countries, and the concentration of manpower in the cities, leaving the under-served rural areas, has caused more than 80% of the population without access to appropriate medical care.2 The rural areas of developing countries are not ?health care deserts?, but they have their own systems of beliefs and customs and their own kinds of indigenous health practitioners. As their adaptation to the impact of western medicine has become better understood, their potential contribution to the primary health care has been reconsidered.2 Health seeking behavior refers to those activities undertaken by individuals in response to symptoms experienced. It is a dynamic process in the house-hold, which combines knowledge, resources, decision making power and the availability of health facilities. It requires some basic knowledge for seeking treatment such as few repeated episodes of any disease in household or any prior experience which helps in making a decision.3 Situation in India: India is a country of villages where 72.2% of people live in rural areas.4 Because of ignorance, illiteracy, cultural and religious factors, rural people are at higher risk of illness. Many factors play an important role such as socio-economic status, cultural acceptability, decision making power, the availability of health care services, or the treatment seeking behavior of the people. Health seeking behavior is influenced by large number of factors apart from knowledge and awareness like bio-social profile, their past experiences with health services, influences at community level, availability of alternate health care providers and their perceptions regarding efficiency and quality of services.4 In India, women of reproductive age group (15-49 years) constitute 21% of the total population, apart from the morbidity experienced by general population; women of reproductive age group also suffer from morbidity due to obstetric and gynecological problems. 5 Around 70% of the deliveries are conducted by untrained personnel, which will have an impact on maternal and infant mortality as well as morbidity. As women of reproductive age come under vulnerable group, it is important to know their treatment seeking behaviour, their decision making power, and utilization of health care services that are available. This study focuses how efficient is the present woman, in making decisions for availing the health care facilities, while the country is talking of women empowerment. The present study is an attempt in this direction.
Objectives
1. To know the treatment seeking behaviour of married women of reproductive age (15-49 years).
2. To know the types of health services utilized by them
METHODOLOGY
This community based cross sectional study includes all married women (732) of reproductive age (15-49 years) living under the sub center Handignur for a period of one year. Questionnaires was prepared which includes information on socio demographic variables, treatment seeking behavior for general health problems, obstetric care gynecological problems, and family planning the types of health services that are used by them and who actually takes the decision for seeking treatment. Study includes all married women of reproductive age group (15-49 years), residing at their home since one year. Research was conducted during January-2007 to December-2007. Place of study: Handignur village is situated 12 kilometers North East of Belgaum city. Handignur Primary Health Center has four sub-centers; with a total population of 24,160.Out of four one of the sub-centers was randomly selected. All villages under this sub-center were included (total no. of household were 762) and from these villages all married women (732) of reproductive age were included in the study. The required information was collected through door to door personal interview after informed, verbal and written consent. The services utilized for some of the problems like abortion and sexually transmitted diseases were not included in the study. Socio economic status: Per capita income in Rupees per month was classified using the modified BG Prasad classification.6.
Results
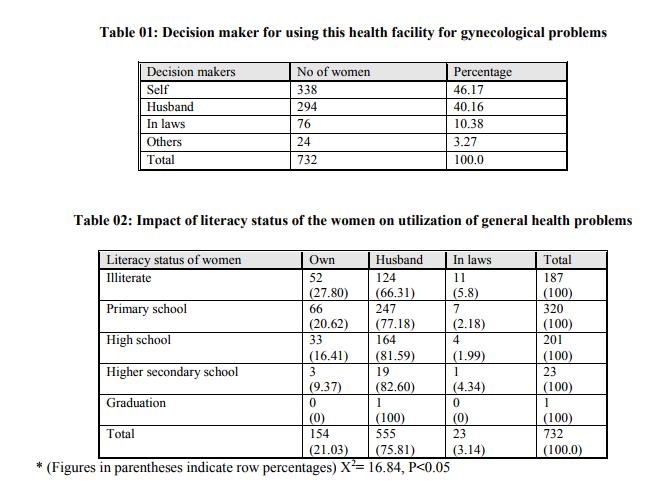
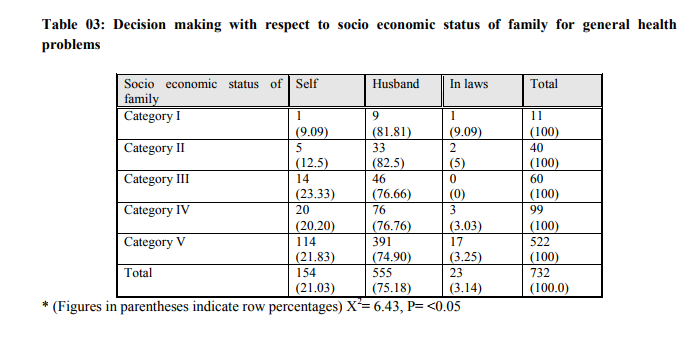
Demographic profile of study participants: The observation stated below are the findings of the present study conducted upon 732 study participants, married women of reproductive age of Handignur sub centre, Belgaum district, Karnataka state. Among the total 732 married women studied majority of them were between the age group of 35-39 years (22.03%). Mean age of patients studied was 35.6 ± 8.87 years. It was observed that out of 732 husbands of study participants, 129 (17.6%) were illiterate and out of 732 study participants (female), 187 (25.5%) were illiterate. While, 135 (18.44%) belonged to nuclear family, 595 (81.28%) study participants were from joint family, and 2 (0.27%) were from broken family. Out of total, 352 (48.08%) were from village Handignur where PHC and sub-center are situated and rest were from other villages under the same PHC. While evaluating modified Prasad‘s classification, out of all study participants, 11 (1.5%) women belonged to category I, 40 (5.5%) women belonged to category II, 60 (8.2%) belonged to category III, 99 (13.5%) belonged to category IV and 522 (71.3%) belonged to category V. When asked about any health facility located near the residence, all of 732 (100%) study participants were aware about PHC/ sub-centre and 352 (48.08%) had knowledge about private clinic. General health problems : This study reveals that, 579 (79.09%) study participants availed the PHC/ Sub centre for general health problems, 29 (3.96%) of the study participants visited a private doctor for general health problems. Out of 732 study participants, 677 (92.48%) women were satisfied with the treatment given at the PHC/sub-centre. 153 (20.90%) women said it would be their own decision for a health facility while 555 (75.18%) women said it would be their husbands decision and rest would depend on others decision to choose a health facility for general health problems. Obstetrics care: In this study out of 732 study participants all women said they were using the PHC/ Sub-centre for their obstetrics. 288 (39.34%) study participants had visited the PHC/sub-centre once during ANC (Antenatal Checkup), 290 (39.01%) women had visited more than once while 154 (21.03%) did not make any visit during ANC as there was no health facility available in and around during their pregnancy. In this study the 578 (78.96%) study participants received iron and folic acid tablets during ANC, and 154 (21.03%) did not receive any iron and folic acid tablets during ANC. 578 (78.96%) participants received injection tetanus toxoid and 154 (21.03%) women did not receive any injection of tetanus toxoid. It was observed that 154 (21.03%) study participants preferred home for conducting delivery as there was no health facility available during pregnancy, 484 (66.12%) preferred PHC / sub-centre for conducting delivery, 24 (3.27%) preferred district hospital, 43 (5.87%) preferred tertiary care center, and 27 (3.68%) women preferred private nursing homes for conducting delivery. The decision makers for using the health facilities for obstetric care were, 153 (20.90%) women made their own decisions, 555 (75.82%) women‘s husbands made the decision, 23 (3.14%) women‘s in laws made the decision, and for one woman (.14%) others who made decision to use the facilities for obstetrics care. Gynecological health problems: Out of 732 study participants who complained of gynecological problems, there were 110 (15.02%) women who complained of menorrhagia, 226 (30.87%) women complained of white discharge, 321 (43.85%) women complained of dysmenorrhoea, and 75 (10.24%) women had other problems. The choice of health facility for gynecological problems given as, 596 (81.42%) women preferred PHC / sub centre, 32 (4.37%) women preferred tertiary care center, 71 (9.69%) preferred the district hospital, 18 (2.45%) women preferred the private hospitals and 15 (2.04%) women preferred other places for gynecological problems. The reasons given for using this health facility for gynecological problems were, 34 (4.64%) women said that it was near to their house, 30 (4.09%) women said it was because all drugs were available, 72 (9.83%) women said because all facilities were provided their, and 596 (81.42%) females said all the reasons were true and that was the reason for using the facility. 338 (46.17%) women made their own decision for using the particular health facility for gynecological problems while others 394 (53.81 %) depended on others decision (Table -1). Family Planning: Out of all participants, 668 (91.25%) women practiced family planning and 64 (8.74%) women did not opt for family planning. In this study out of 732 study participants, 668 women were using any method of family planning, 57 (8.53%) women were using oral contraceptive pills as contraceptive methods, 79 (67.06%) women had got copper T inserted, 31 (23.80%) women had undergone tubectomy, 6 (0.59%) women said their husbands were using condoms. Total 668 couples were using family planning methods. Out of 668 participants, 261 (39.07%) women made their own decision for using for using contraceptive methods and 323 (48.35%) women had taken the advice of their husbands for using contraceptive methods. Impact of literacy status of the women on utilization of general health problems (Table – 2): The decision making with respect to education was as follows, in illiterates 27.80% women made their own decision, 66.31% women consulted their husbands, 5.88% women consulted their in laws, and no women consulted others. In primary school educated group, 20.62% women made their own decision, 77.18% women consulted their husbands, and 2.18% women consulted their in laws, In high school educated group, 16.41% women made their own decision, 81.59% women consulted their husbands, and 1.99% women consulted their in laws, In higher secondary educated group, 9.37% women made their own decision 82.60% women consulted their husbands, 4.34% women consulted their in laws for decision to take treatment for general health problems. Impact of literacy status of the women on utilization of Obstetrics problems: It was observed that decision making with respect to education was as follows, in illiterate group, 91.97% women made their own decision, 1.77% women consulted their husbands, 0.53%women consulted their in laws, and 0.53% women consulted others. In primary school educated group, 39.06% women made their own decision, 50.62% women consulted their husbands, 6.25% women consulted their in laws and 4.06% women consulted others. In high school educated group, 35.32% women made their own decision, 62.18% women consulted their husbands, 0.99% women consulted their in laws and 1.49% women consulted others. In higher secondary educated group, 49.96% women made their own decision, 56.52% women consulted their husbands, and nobody consulted their in laws or others for decision to take treatment for obstetric care. Impact of literacy status of the women on utilization of gynecological problems: It stated that decision making with respect to education was as follows; in illiterate group, 91.97% women made their own decision, 0.53% woman consulted their husbands, 6.95% women consulted their in laws, and 0.53% woman consulted others. In primary school educated group, 30.93% women made their own decision, 16.56% women consulted their husbands, and 45.93% women consulted their in laws, and 6.56% women consulted others. In high school educated group, 29.35% women made their own decision, 9.45% women consulted their husbands, 60.19% women consulted their in laws, and 0.99% women consulted others. In higher secondary educated group, 34.78% women made their own decision, 13.04% women consulted their husbands, and 52.17% women consulted their in laws. In graduate women, all women made their own decision for treatment of gynecological problems.
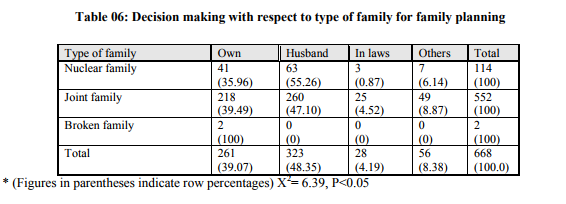
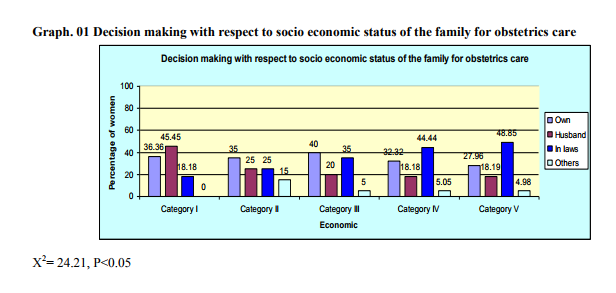
Impact of literacy status of the women on utilization of family planning methods: In this study decision making with respect to education was as follows; in illiterate group, 45.69% women made their own decision, 53.22% woman consulted their husbands, 0.53% women consulted their in laws, and 0.53% woman consulted others. In primary school educated group, 38% women made their own decision, 42.80% women consulted their husbands, 8.11% women consulted their in laws and 11.07% women consulted others. In high school educated group, 34.73% women made their own decisions, 50% women consulted their husbands, 2.63% women consulted their in laws, and 12.63% women consulted others. In higher secondary school educated group, 35% women made their own decision, 60% women consulted their husband, and 5% woman consulted others while all graduate women consulted their husband for family planning methods. Decision making with respect to socio economic status of family for general health problems (Table – 3): It was as follows; in category I, 9.09% woman made their own decision, 81.81% women consulted their husbands, 9.09% woman consulted their in laws. In category II group, 12.5% women made their own decision, 82.5% women consulted their husbands and 5% women consulted their in laws. In Category III group, 23.33% women made their own decision while 76.66% women consulted their husbands. In Category IV group, 20.20% women made their own decision 76.76% women consulted their husbands and 3.03% women consulted their in laws. In Category V group, 21.83% woman made their own decision, 74.90% consulted their husbands, 3.25% women consulted their in laws and none consulted others for treatment of general health problems. Decision making with respect to socio economic status of the family for obstetrics care(Graph-1); in category I, 36.36% women made their own decision, 45.45% women consulted their husbands and18.18% women consulted their in laws. In category II group women 35% women made their own decision, 25% women consulted their husbands, 25% women consulted their in laws, and 15% women consulted others. In Category III group, 40% women made their own decision, 20% women consulted their husbands, 35% women consulted their in laws, and 5% women consulted others. In Category IV group, 32.32% women made their own decision 18.18% women consulted their husbands, 44.44% women consulted their in laws, and 5.05% women consulted others. In Category V group, 27.96% woman made their own decision, 18.19% consulted their husbands, 48.85% women consulted their in laws and 4.98% women consulted others for obstetric care. Decision making with respect to socio economic status of family for gynecological health problems (Table -4); in category I, 9.09% woman made their own decision while rest consulted their husbands. In category II group, 12.55% women made their own decision, 82.5% women consulted their husbands, and 5% women consulted their in laws. In Category III group, 23.33% women made their own decision and 76.66% women consulted their husbands. In Category IV group, 22.22% women made their own decision, 74.74% women consulted their husbands, and 3.03% women consulted their in laws. In Category V group, 21.83% woman made their own decision, 74.90% consulted their husbands, and 3.25% women consulted their in laws for treatment of gynecological health problems. Decision making with respect to socio economic status of family for family planning (Table -5); In category I group, 9.09% woman made their own decision while 90.90% women consulted their husbands. In category II group, 12.5% women made their own decision, 82.5% women consulted their husbands, and 5% women consulted their in laws. In Category III group, 23.33% women made their own decision, 76.66% women consulted their husbands, and no women consulted their in laws. In Category IV group, 22.22% women made their own decision 74.74% women consulted their husbands, and 3.03% women consulted their in laws. In Category V group, 21.83% woman made their own decision, 74.90% consulted their husbands, and 3.25% women consulted their in laws for family planning methods. Decision making with respect to the type of family for general problems; 16.93% women who belonged to the nuclear family made their own decision, 79.83% women consulted their husbands, and 3.22% women consulted their in laws. In women belonging to joint family, 21.94% women made their own decision, 74.91% women consulted their husbands, and 3.13% women consulted their in laws. And in broken family 100% women took their own decision for taking treatment for general health problems. Decision making with respect to the type of family for obstetrics problems; 45.16% women who belonged to the nuclear family made their own decision, 19.35% women consulted their husbands, 33.87% women consulted their in laws and 1.61% women consulted others. In joint family women, 26.73% women made their own decision, 19.14% women consulted their husbands, 47.85% women consulted their in laws and 6.27% women consulted others, while in broken family all women took their own decision for obstetric care. Decision making with respect to the type of family for gynecological problems; 34.67% women who belonged to the nuclear family made their own decision, 12.09% women consulted their husbands and 53.22% women consulted their in laws. In joint family women, 48.67% women made their own decision, 10.06% women consulted their husbands, 37.29% women consulted their in laws and 3.96% women consulted others. Decision making with respect to type of family for family planning (Table -6); 35.96% women who belonged to the nuclear family made their own decision, 55.26% women consulted their husbands, 0.87% women consulted their in laws and 6.14% women consulted others. In joint family women, 39.49% women made their own decision, 47.10% women consulted their husbands, 4.25% women consulted their in laws and 8.87% women consulted others.
DISCUSSION
The present study revealed that, 22.03% of the women were in the age group of 35-39 years. The literacy rate of the women was found to be 74.4%. The literacy rate of their husbands was found to be 82.4%. Joint family was the commonest being 81.28%. According to the census data the literacy of females is 52% so being significant.7 Three-forth of the women belonged to the category V of modified B G Prasad‘s classification of socio-economic status. All married women of reproductive age had the knowledge of the health facilities available near their homes. Door steps services were provided to all married women, 88.93% of the study participants said ANM‘s provided them these services. And all study participants said that services provided were curative, diagnostic, health education, natal services, family planning and immunization. Out of the 732 women for general health problems, 79.09% of the women preferred to go the PHC/ sub-center. The reason that they gave was easy accessibility, as agreed by 99.59%.of women. 92.49% were satisfied by the treatment given. 75.18% of women said their husband‘s were the decision makers for their general health problems. For obstetrics care all 732 women preferred going to the PHC/ sub center. 39.34% said they made 1-2 visits for their ANC checkups, and it was also noticed that 21.03% of the women did not make a single visit during the time of their pregnancy. 78.96% of women had received iron and folic acid tablets during the time of their pregnancy. More than half of study participants told doctor providing it to them. 78.96% had received injection tetanus toxoid during the time of their pregnancy. 66.12% of women preferred the PHC / sub center as a convenient place for getting delivered. 47% preferred the doctors to conduct their deliveries.
Three forth of women said their husbands took the decisions concerned to obstetrics care. The choice of health facility opted by 80% of women for their gynecological problems was either PHC / sub center. 81.42% women went there because it was near to the house and all necessary and emergency drugs were available and also all facilities were provided. More than 90% women said they were practicing either temporary or permanent methods or their husbands were using temporary methods of family planning. 61.07% women were using copper T as the method of family planning. 61.07% women said the doctors at the PHC/ sub center helped them in providing family planning services. Around 50% women said their husband‘s decided about the family planning.
CONCLUSION
In the present study, the women of reproductive age group residing in PHC/sub center Handignur had a fair knowledge regarding treatment seeking, the availability of health care services and the types of services offered by them. Most of the women preferred the PHC/ sub center for mostly obstetric care as the new generation was more aware of the health care system. However it was observed that they utilized much of the services offered by the PHC/ sub center for preventive services as it was adequate and free of cost. For obstetric care they did not hesitate in deciding the choice of place to deliver as Handignur PHC/ sub center is providing all modern facilities, including a baby warmer and a neo natal resuscitation kit. Door steps services were provided by the health workers uniformly at all the three villages that come under the PHC/ sub center. The frequency of the health visitor to the area was also there for health education. Antenatal care was provided by health workers and utilized by the women of the PHC/ sub center. Younger women availed the facility more compared to the older generation, who did not have the privilege women of a health facility near their house at the time of their pregnancy. Women‘s awareness towards treatment seeking for obstetric care was also found, as compared to the older generation. The importance of attending the ANC clinics, intake of iron and folic acid tablets, and the two doses of tetanus toxoid injections was also seen. This was due to the regular health education conducted by the doctor, health visitors, ANM‘s and the anganwadi workers. The decision maker for general health problems, obstetric care and for family planning was still dependent on their husbands where as for the gynecological problems the majority of women made her own decisions.
ACKNOWLEDGEMENT Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Pamela A Hunter and Farhat Sultana, ?Health Seeking Behaviour and the meaning of Medications in Bolochisthan, Pakisthan?; Soc. Sci. Med. Vol. 34, No. 12, pp. 1385 – 1397, 1992.
2. Pierre Claquin ?Private Health Care Providers in Rural Bangladesh?, Soc. Sci. Med. Vol. 15B, pp. 153 – 157, 1981.
3. Alex Kroeger, ?Anthropological and SocioMedical Health Care research in developing countries?, Soc. Sci. Med. Vol. 17, No. 3, pp. 147 – 161, 1983.
4. K Park, Text book of Community Medicine, 18th Edition M/ s Banarasidas Bhanot Publishers; 353- 383, 2005.
5. M Jain, D Nanda, S K Misra, ?Quality assessment of Health Seeking Behaviour and Perception regarding Quality of Health Care Services among rural community of District Agra?, Indian Journal of community medicine Vol. 31, No. 3, July – September, 2006.
6. Kulkarni A P, Barde. J. P. Text book of Community Medicine, Ist edi. Mumbai: Vora Medical Publications: 1998.
7. Governments of India, Ministry of Statistics and Program Implementations, file no. M- 12011/ 2/ 2005- PCL.

|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License