IJCRR - 8(20), October, 2016
Pages: 25-29
Print Article
Download XML Download PDF
A STUDY OF NEONATAL HYPERBILIRUBINEMIA IN A TERTIARY CARE HOSPITAL IN THE NORTH EASTERN REGION OF INDIA
Author: Sungdirenla Jamir, Arunkumar Singh Ngangom, Davina Hijam, Chubalemla Longkumer, Abhishek Dubey, M. Amuba Singh, Kh. Ibochouba Singh
Category: Healthcare
Abstract:Neonatal jaundice is yellow colouration of the skin and the sclera of newborn babies due to accumulation of bilirubin. This is associated with hyperbilirubinaemia, a condition where bilirubin level is raised in the circulation.
Objectives: To assess the etiological factors of neonatal hyperbilirubinemia and therapeutic interventions in a tertiary care hospital in the north eastern region of India.
Methods: A prospective cohort study was carried out in the Department of Biochemistry, Regional Institute of Medical Sciences (RIMS), Imphal, Manipur for a period of two years. One hundred fifty newborns with jaundice aged up to 28 days, both term and preterm were included in this study. Careful clinical assessments were done to assess the possible etiologies. Serum bilirubin was determined by colorimetric method as described by Jendrassik and Grof [12]. Monitoring of serum bilirubin was done by serial measurements once a day in the morning.
Results: Significant hyperbilirubinemia (TSB>15mg %) was seen in 58 (38.7%) neonates while 92 (61.3%) had TSB< 15mg%. There was no significant difference in the mean serum bilirubin values between neonates of different birth weights and maturity. The most common etiological factor for neonatal hyperbilirubinemia was found to be physiological (60.7%) Pathological cause constituted 39% of the neonates. Deficiency of enzyme G6PD (12%) was found to be the commonest cause of pathological neonatal hyperbilirubinemia, followed by prematurity (8.7%) and sepsis (5.3%).
Conclusion: Phototherapy is effective in most cases but exchange transfusion should also be considered it when it failed. Due to high incidence of G6PD deficiency in this, it is recommended to introduce qualitative test of this enzyme as a routine laboratory investigation for all icteric neonates so as to achieve early diagnosis and prevention of adverse consequences of neonatal hyperbilirubinemia.
Keywords: Neonatal hyperbilirubinemia, Phototherapy, Exchange transfusionvvvv
Full Text:
INTRODUCTION:
Hyperbilirubinemia is a common and in most cases, benign problem in neonates. Jaundice is observed during the 1st week of life in approximately 60% of term infants and 80% of preterm infants.[1] The serum bilirubin level varies with birth weight, gestational age, chronological age and internal milieu of the body. When total serum bilirubin (TSB) level exceeds a critical limit, it crosses the blood brain barrier. [2] Neonatal hyperbilirubinemia (NNH), defined as a TSB level above 5 mg per dL (86 μmol per L), is a frequently encountered problem. Chemical hyperbilirubinemia is defined as TSB levels >2mg/dl, is universal in newborns during first week. Although up to 60 percent of term newborns have clinical jaundice in the first week of life, few have significant underlying disease. [3]
Neonatal hyperbilirubinemia is termed as significant when it needs close supervision, further evaluation and sometimes intervention.[4,5] In case of preterm newborn significant hyperbilirubinemia varies according to gestational age and birth weight.[6,7] Neonatal hyperbilirubinemia results from a predisposition to the production of bilirubin in newborn infants and their limited ability to excrete it. The infants, especially preterm infants, have higher rates of bilirubin production than adults, because they have red cells with a higher turnover and a shorter life span. [8] Neonatal jaundice refers to the yellow colouration of the sclera and skin of newborn babies that result from hyperbilirubinemia. It is the most common condition requiring medical attention in newborn babies. It is also a common cause of readmission to hospital after early discharge of the newborn babies. [9]
Some of the most common causes of neonatal jaundice include physiological jaundice, breast feeding or non-feeding jaundice, breast milk jaundice, prematurity leading to jaundice and various pathological causes like hemolytic disease, liver dysfunction, neonatal sepsis, deficiency of glucose-6-phosphatase (G6PD) enzyme, Rh-incompatibility, hypothyroidism and rare conditions such as Gilbert’s syndrome, Crigler-Najjar syndrome etc.[10]
The early diagnosis and treatment of neonatal hyperbilirubinemia is of utmost importance as bilirubin is toxic to CNS and elevated serum bilirubin can cause neurological complication. Further, the incidence, etiological and contributory factors to neonatal jaundice differ in ethnicity and geographical distribution. Thus the present study is undertaken to assess the etiological factors of neonatal hyperbilirubinemia and therapeutic interventions in a tertiary care hospital in the north eastern region of India.
MATERIAL AND METHODS:
A prospective cohort study was carried out in the Department of Biochemistry, Regional Institute of Medical Sciences (RIMS), Imphal in collaboration with the Department of Pediatrics, RIMS, Imphal, Manipur for a period of two years (November 2012 – October 2014). One hundred fifty newborns with Jaundice aged up to 28 days, both term and preterm were included in this study while those with age more than 28 days or with major malformations were excluded from this study.
A detailed history of both mother and baby and meticulous physical examination of the baby were carried out. Gestational age was calculated from the 1st day of the last menstrual period of the mother. Those babies born between 37-41 weeks of gestation were classified as term babies. Those born before 37 weeks were classified as preterm babies. Babies weighing less than 2500g were defined as low birth weight babies and those weighing <1500g as very low birth weight (VLBW).[11]
Careful clinical assessment was done to assess the possible etiologies. Samples were collected at the time of admission, before the start of treatment. Serum bilirubin was determined by colorimetric method as described by Jendrassik and Grof [12] using RX Imola automatic analyser (Randox Laboratories, USA). Monitoring of serum bilirubin was done by serial measurements once a day in the morning.
The management of hyperbilirubinemia in the new born is in accordance to American Academy of Pediatrics Clinical Practice Guieline[13]
Statistical Analysis: The data were analysed using SPSS version 16. All data were expressed in Mean + Standard deviation. c2 test and student t- test were used wherever found suitable and necessary interpretations were made. P value <0.05 was considered significant.
Study was approved by the institutional ethical committee. Informed consent was obtained from all individuals and nature of the study was explained to them.
RESULTS:
DISCUSSION:
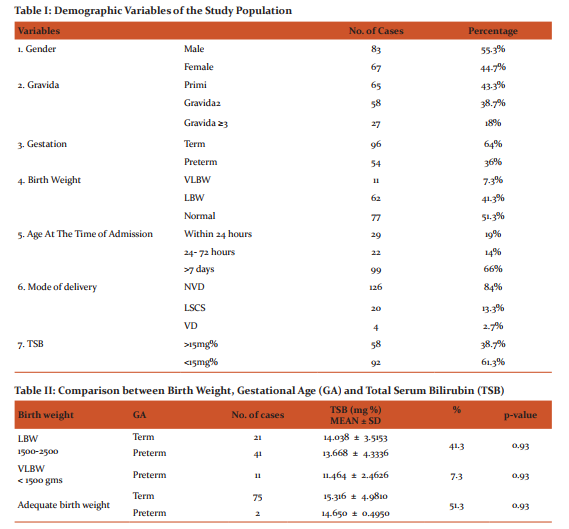
Table I showed that out of 150 neonates in the study, 64% were term, 44.3% were pri mi births and 51.3% had adequate birth weight. 84% neonates were delivered by NVD. These findings are comparable to the findings of D Nepal et al.[14] Significant hyperbilirubinemia (TSB>15mg%) was seen in 58 (38.7%) neonates while 92 (61.3%) had TSB<15mg%. These findings are consistent with the findings of Dhanjal GS et al.[15] Since most of the deliveries were institutional deliveries, this could be the reason for lesser number of neonates having significant hyperbilirubinemia.
From Table II it was observed that there was statistically no much difference in the mean serum bilirubin value between neonates of different birth weights and maturity (p>0.05). This finding is consistent with the findings of Dholakia A et al [16] and Dhanjal GS et al.[17]
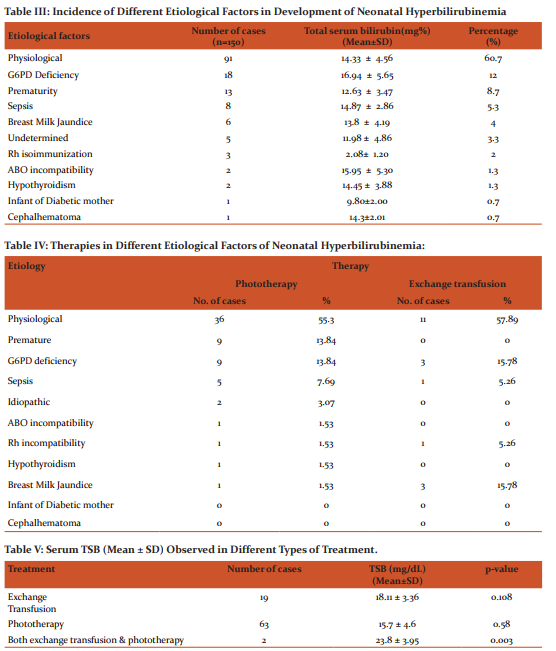
Neonatal hyperbilirubinemia was found to be physiological in 60.7% (91) cases while 39% (59) cases were pathological. This finding was similar with the findings of Bahl L et al [18] who reported 63.8% of cases in his study to be physiological and 36.2% cases to be pathological.
It was observed from Table-III that the most common etiological factor for pathological neonatal hyperbilirubinemia was due to deficiency of enzyme G6PD (12%). This was followed by prematurity (8.7%) and sepsis (5.3%). The other common causes included breast milk jaundice (4%), Rh isoimmunisation (2%), ABO incompatibility (1.3%) and hypothyroidism (1.3%). Lesser common causes were in infant of diabetic mothers (0.7%) and cephalhematoma (0.7%). 5 cases (3.3%) had no obvious cause and maybe considered as idiopathic. This finding was consistent with the findings of Mallick PK et al [19] where 4% of cases were idiopathic. Narang A et al [20] had cited in his study that various reports from our country has revealed that idiopathic hyperbilirubinemia ranges between 8.8 to 57.6%. The present finding is inconsistent with the Indian reports. This may be due to difference in genetic make-up and / or environmental factors. It was also observed that the difference in the total serum bilirubin (Mean±SD) between the various etiological factors is statistically insignificant (p value>0.05).
Table VI shows that among neonates with physiological HB, the mean ± SD total serum bilirubin (TSB) at the time of initial assessment was 12.72 ± 4.10 mg/dL. The mean ± SD peak level (TSB peak) was 14.28 ± 2.54 mg/dL while mean ± SD at the time of discharge (TSB last) was 10.35 ± 2.27 mg/dL. In this study, peak level of serum bilirubin was reached by the mean age of 5 days falling rapidly thereafter over the next few days. These findings were consistent with the findings of Shartsho JT. [21]
In this study, the incidence of hyperbilirubinemic neonates receiving either PT or ET or both was found to be 54.7% (Table IV). 65(43.3%) were given phototherapy and 19(12%) received blood exchange transfusion. Out of these, 2 neonates received both PT and ET. So 45.3% were not treated by either PT or ET or both. These findings are similar with the findings of Rasul CH et al[22] who reported that the most common treatment in their study was phototherapy(62.6%) while ET was used only in 5.2% cases. 61% patients required only phototherapy in a study by Khaton S et al[23]. It is evident from Table V that Neonates with higher mean serum bilirubin (23.8 ± 3.95mg/dL) received both phototherapy and exchange transfusion (p<0.01).
CONCLUSION:
It can be concluded from this study that the most common etiological factor for neonatal hyperbilirubinemia is physiological constituting 60.7% of all cases while pathological cause constituted 39% cases. Deficiency of enzyme G6PD (12%) was found to be the commonest cause of pathological neonatal hyperbilirubinemia, followed by prematurity (8.7%) and sepsis (5.3%). The other common causes included breast milk jaundice (4%), Rh isoimmunisation (2%), ABO incompatibility (1.3%) and hypothyroidism (1.3%). Lesser common causes were in infant of diabetic mothers (0.7%) and cephalhematoma (0.7%). In 5 cases (3.3%), the cause of pathological hyperbilirubinemia remained undetermined.
The incidence of hyperbilirubinemic neonates receiving either PT or ET or both was found to be 54.7%. Most common treatment given was phototherapy 65(43.3%). 19(12%) received blood exchange transfusion. Out of these, 2 neonates received both PT and ET and they were found to be G6PD deficient. Rate of exchange transfusion is much higher in G6PD deficient neonates (50%) compared to G6PD normal neonates (7.57%).
It can also be concluded from the present study that phototherapy is effective in most cases but exchange transfusion should also be carried out when it failed. Due to considerable incidence of G6PD deficiency found in this study (12%), it is recommended to introduce qualitative test of this enzyme deficiency as a routine laboratory investigation for all icteric neonates for early diagnosis and prevention of adverse consequences of neonatal hyperbilirubinemia.
References:
- Kliegman RM, Behrman RE, Jensen HB, Stranton B: Nelson Textbook of Pediatrics. Jaundice and hyperbilirbinemia in the newborn. 19th ed. Philadelphia: Saunders; 2012.p. 603-12.
- Brown AK, Damus K, Kim MH et al. Factors relating to readmission of term and near-term neonates in the first-two weeks of life. Early discharge survey group of the Health Professional advisory board of the Greater NY Chapter of the March of Dimes. J Perinat. Med 1999; 27(4): 263-75.
- IAP- NNF National Task Force 2006 on guidelines for level II neonatal care. IAP-NNF guidelines 2006 on level II neonatal care. Jaundice in newborn; 2006.p. 187-210.
- Bhutani VK, Johnson L,Sivieri EM. Predictive ability of a predischarge hour serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and nearterm newborns. Pediatrics 1999; 103:6-14.
- Newman TB, Maisels MJ. Evaluation and treatment of jaundice in the term newborn. A kinder, gentle approach. Pediatrics1992; 89:809-18.
- Bhat YR, Rao A. Transcutaneous bilirubin in predicting hyperbilirubinemia in term neonates. Indian J Pediatr 2008; 75:119-23.
- Linn S, Schoenbaum SC, Monson RR Rosner B, Stubblefield PG, Ryan KJ. Epidemiology of neonatal hyperbilirubinemia. Pediatrics1988; 75:770-74.
- Brouillard R. Measurement of red blood cell life-span. JAMA 1974; 230:1304-5.
- Akobeng AK: Neonatal jaundice, Clinical evidence. Am Fam Physician 2005; 71(5):947-48.
- Madan A, James RM, Stevenson DK. Neonatal Hyperbilirubinemia. In: Taeusch HW, Ballard RA, Gleason CA. Avery’s diseases of the new born. 8th ed. Philadelphia: Elsevier Saunders; 2004.p. 1226-56.
- Tooley WH. Intensive care nursery house staff manual. Very low and extremely low birth weight Infants. UCSF hospital. University of California. 8th ed. 2003; 65-8.
- Jendrassik L. and Grof P; Biochem. Z. 1938; 81:297.
- Paediatrics Vol. 114 (1) July 2014
- Nepal D, Banstola D, Dhakal AK, Mishra U and Mahaseth C. Neonatal hyperbilirubinemia and its early outcome. JIOM 2009; 31(3): 17-20.
- Dhanjal GS, Jain G and Singh M. Clinico-etiological study of neonatal jaundice in a tertiary carecentre in Ambala (Haryana) India. JBPR 2014; 3(1): 64-67.
- Dholakia A, Darad D and Chauhan C. Neonatal hyperbilirubinemia and its correlation with G6PD enzyme deficiency in a tertiary care hospital in Gujarat. National J of Medical Research 2012; 2(1): 59-62.
- Dhanjal GS, Jain G and Singh M. Clinico-etiological study of neonatal jaundice in a tertiary carecentre in Ambala (Haryana) India. JBPR 2014; 3(1): 64-67.
- Bahl L, Sharma R, Sharma J. Etiology of neonatal jaundice at Shimla. Indian J Pediatr 1994; 31: 1275-8.
- Mallick PK, Alam B. Aetiological study of neonatal hyperbilirubinaemia-A hospital based prospective study. Medicine Today 2012; 24(2): 73-4.
- Kuruvilla KA. Atanu ST, Jana K. Glucose-6-Phosphate dehydrogenase deficiency in neonatal hyperbilirubinemia in a South Indian Referral Hospital. Indian J Pediatr 1998; 35: 52-4.
- Shartsho JT (2007). A study on neonatal jaundice (0-14). Unpublished doctoral dissertation, Manipur University, Canchipur, Manipur.
- Rasul CH, Hasan MA, Yasmin F. Outcome of neonatal hyperbilirubinemia in a tertiary care hospital in Bangladesh. Malaysian J Med Sci. 2010; 17 (2):40-4.
- Khaton S, Islam MN. Neonatal jaundice-clinical profile of 140 cases. Bang J Child Health. 1993; 17:158-63.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License