IJCRR - 4(12), June, 2012
Pages: 198-207
Date of Publication: 22-Jun-2012
Print Article
Download XML Download PDF
CORRELATION OF PERIODONTAL DISEASE SEVERITY WITH RHEUMATOID DISEASE ACTIVITY AMONG RHEUMATOID ARTHRITIS PATIENTS IN CHENNAI: A CROSS SECTIONAL STUDY
Author: A.M.Deva Priya, P.K.Saraswathi, K.H.Pani Shankar, M.G.Krishna Baba
Category: Healthcare
Abstract:Aim: The current study aims to determine whether there is a relationship between Rheumatoid arthritis
disease activity and severity of chronic periodontitis in the study population. Methods: 100 patients aged
20-70 years, diagnosed with Rheumatoid arthritis and Chronic periodontitis were selected for the study.
The rheumatoid disease activity was assessed using DAS 28 and severity of periodontitis was classified
based on clinical attachment loss. Physical disability was elicited using Indian Health Assessment Questionnaire and Oral hygiene status was measured using Oral Hygiene Index. Results: Among the 100 Rheumatoid Arthritis patients with periodontitis, 11 were males (11%) and 89 were females (89%). Rheumatoid disease activity showed no correlation with periodontal disease severity (r value 0.01,p value>0.05) . Functional disability of the patients showed a significant correlation with their oral hygiene
status (r value 0.232,p value< 0.05). The number of missing teeth showed significant correlation with
clinical attachment loss (r value 0.511,p value< 0.001) and functional disability(r value 0.259,p value< 0.001). Conclusion: It can be concluded from the results of our study that severe rheumatoid
disease activity impairs the functional ability of the patients in maintaining good oral hygiene which in
turn leads to periodontitis
Keywords: Functional disability, Oral hygiene status, Periodontitis, Rheumatoid arthritis
Full Text:
INTRODUCTION
Periodontal medicine is an emerging branch of Periodontology that has been establishing a strong relationship between periodontal and systemic health or disease1 . Studies have shown significant association between Periodontal Disease (PD) and coronary heart disease2 , diabetes3 , stroke4 , respiratory disease5 , preterm low birth weight delivery6 .Rheumatoid Arthritis (RA) has been included in the group of systemic diseases known to influence the periodontium. Periodontitis is a chronic destructive inflammatory disease of the supporting structures of the teeth. RA is a progressive inflammatory disorder characterised by proliferation of the synovial membrane and persistent uncontrolled inflammation resulting in chronic destructive polyarthritis7 . Both the diseases are chronic inflammatory diseases with excessive level of proinflammatory cytokines, Matrix MetalloProteinase (MMP) and prostaglandins and decreased level of Tissue Inhibitors of MMPs, eventually leading to destruction of hard and soft tissues. They are of different etiology but share similar pathologic, immunologic, environmental and genetic factors. Smoking and HLA-DRB1 shared epitope alleles are common risk factor for both the diseases 8, 9 . Porphyromonas gingivalis, an important periodontal pathogen possesses a unique enzyme Peptidyl Arginine Deiminases (PAD) that causes citrullination of proteins, generating citrullinated peptides leading to generation of autoantigens that could possibly initiate autoimmunity in RA10 and link both the diseases. Periodontopathic bacteria like Porphyromonas gingivalis, Tannerella forsythensis, and Prevotella intermedia have been identified in Rheumatoid Arthritis synovial fluid11. While causal relationship is unlikely there is a possibility of common dysregulation of host inflammatory response in both the diseases which needs to be established. The relationship between Rheumatoid Arthritis and Periodontitis is hypothesised to be bidirectional with RA affecting the progression of periodontal disease and vice versa but results are not confirmatory. Self reported epidemiological studies12,13, cross sectional and case control studies14,15,16 have shown that RA patients have a higher prevalence of periodontitis , more number of missing teeth and severe periodontal destruction with deeper pockets and attachment loss. Ribeiro et al17 , Havemose-Poulsen et al18, Al Katma et al19 , Ortiz20 et al have reported that Periodontitis exacerbates the severity of rheumatoid arthritis and could be a possible risk factor for development of RA .Clinical trials19,20 have provided evidence that non surgical treatment of periodontal disease can reduce the severity of rheumatoid disease severity . Data from First National Health and Nutrition Examination Survey21 and ARIC22 study suggests that periodontitis patients have an increased risk of incident or prevalent RA but findings from the Nurses Health Study23 study found no such association. As limited studies are available and conflicting results have been published, this study was undertaken, to determine whether there is a relationship between the severity of rheumatoid arthritis and severity of periodontitis. Aims of the study were 1. To assess the severity of RDA and to correlate it with the severity of periodontitis, oral hygiene status, and functional disability among the RA patients with periodontitis. 2. To correlate the oral hygiene status with the functional disability of the RA patients 3. To correlate the number of missing teeth with clinical rheumatologic variables.
MATERIALS AND METHODS
This observational study was conducted in the outpatient clinic of Rheumatology department, Government General Hospital, Chennai. Ethical clearance was received from the Ethical committee of Madras Medical College, Chennai. 100 patients presenting for the first time to the outpatient clinic and diagnosed with RA were selected for the study. The patients were diagnosed with Rheumatoid Arthritis based on the 1987 Revised American Rheumatism Association Criteria for the classification of Rheumatoid Arthritis24 . Patients aged between 20 – 70 years were selected for the study. RA patients with Clinical Attachment Loss (CAL) associated with periodontal inflammation were selected and periodontal disease was defined as ≥ 2 sites with interproximal CAL ≥ 4mm, not on the same tooth or ≥ 2 sites with interproximal Probing Pocket Depth (PPD) ≥ 4mm, not on the same tooth25. Patients were included in the study if they had at least 8 teeth in the oral cavity, not taken antibiotics within the past 6 months and had no oral prophylaxis or periodontal therapy before. Patients who had CAL associated with malpositioned tooth, improper restorations or crowns, aggressive tooth brushing were not included. Patients were excluded from the study if they were under medication with drugs like anticonvulsant, calcium channel blockers, immunosuppressant that can influence the periodontium, gave a history of hypertension, diabetes mellitus and xerostomia, had medical conditions requiring antibiotic prophylaxis before periodontal examination, smokers, pregnant, lactating women and refused to give informed consent. Written informed consent was obtained from all the patients. Rheumatoid Disease Activity (RDA) was measured using Disease Activity Score28 (DAS 28). DAS is a clinical index developed, to evaluate the status and course of RA disease activity; it combines information from swollen joints, tender joints, acute phase response and general health into one continuous measure of rheumatoid inflammation. DAS 28(4) consists of 28 Tender joint count (TJC), 28 swollen joint count (SJC), Erythrocyte sedimentation Rate (ESR) and General health on visual analogue Scale (VAS).The rheumatologic examinations were performed by specialist rheumatologist and the periodontal examination was performed by a single Periodontist. The swollen joint count reflects the amount of inflamed synovial tissue and it influences the range of joint motion. Tender joint count is associated more with the level of pain. VAS is a measurement instrument that tries to measure a characteristic or attitude that is believed to range across a continuum of values and cannot easily be directly measured. It is usually a horizontal line, 100 mm in length, marked 0 at left extreme to 100 on the right extreme. The patient marks on the line the point that they feel represents their perception of their current state of health. The VAS score is determined by measuring in mm from the left hand end of the line to the point that the patient marks. All the RA patients were referred for routine haematological lab investigations in the same hospital.ESR and Rheumatoid Factor (RF) titre was recorded from the lab for the study patients. ESR was measured using Westergren Method and the results are given in millimetre value. RF was measured using latex agglutination method. Functional Disability was elicited Using Indian Health Assessment Questionnaire (HAQ)26. RA patients develop difficulty in doing their daily activities and measurement of this disability is routinely done in all outcome studies. Majority of the patients were not educated and also in view of their physical disability, the questionnaire was explained to the patients by the Periodontist and the response was recorded and scoring was given. Clinical oral examination consisted of recording the number of teeth present, number of missing teeth, Oral Hygiene Index (OHI), PPD and CAL .The cumulative end point of periodontal disease is CAL .It is the distance between the base of the pocket and fixed point on the crown, such as cementoenamel junction and is a valid method for assessment of loss of attachment of junctional epithelium from the cementoenamel junction.CAL was measured manually using Williams periodontal probe. Attachment loss was recorded at 6 sites around all teeth. Mean CAL was calculated and based on 1999, American Academy Of Periodontology criteria for chronic periodontitis27, the patients were classified as mild, moderate and severe periodontitis. OHI given by Greene and Vermillion, Waggener28 was used to measure existing debris and calculus as an indicator of oral cleanliness. Data collected was analysed statistically using Microsoft SPSS 15 package. Association between the variables was studied using Pearson chi square test and correlation was done using Pearson correlation coefficient.
RESULTS
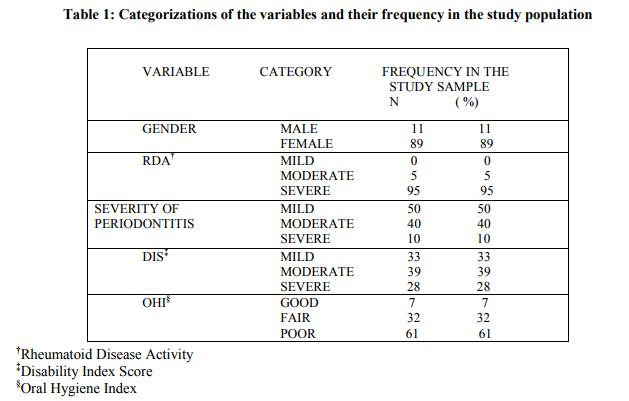
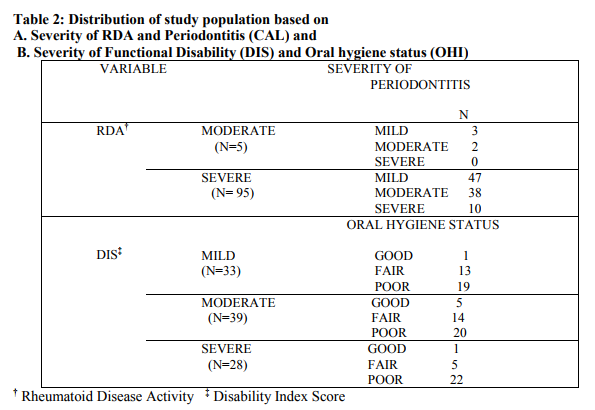
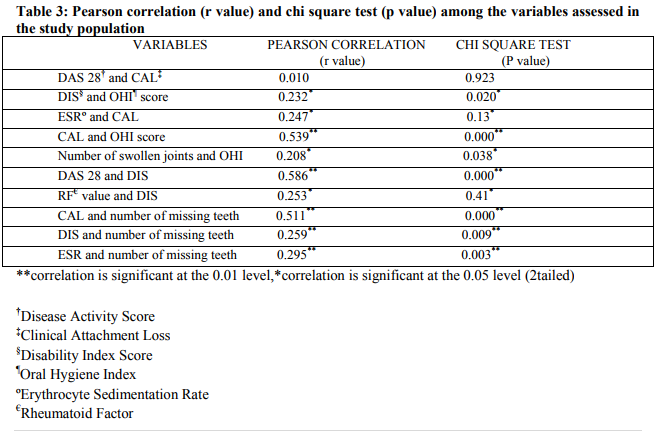
Among the 100 Rheumatoid Arthritis patients with periodontitis, 11 were males (11%) and 89 were females (89%). Mean age of the study population was 41.94 years (SD±11.85).Mean and standard deviation of the variables assessed in the study were number of tender joints 20.89(SD±6.86), swollen joints 12.45(SD±8.28), DAS 28(4) 6.87(SD±0.98), RF 208.1(SD±105.2), PPD 2.49(SD±0.70), CAL 2.99 (SD±1.61), DIS 1.49 (SD±0.79) and OHI score 6.97(SD±2.66). Based on DAS 28(4), the patients were classified as having mild, moderate or severe RDA (Table1).Majority of patients had severe RDA. Based on CAL, patients were categorised as having mild, moderate or severe periodontitis.50% of the patients had mild periodontitis (Table1). Frequency distribution of study population based on severity of periodontitis and RDA is shown in Table 2 .Five patients had moderate RDA of which 3 had mild periodontitis and 2 had moderate periodontitis. Among patients with severe RDA, 47 patients had mild periodontitis, 38 had moderate and 10 had severe periodontitis. Distribution of study population based on severity of Functional disability and oral hygiene status is also shown in Table 2. Among the patients with different degree of functional disability majority of the patients had poor oral hygiene. RDA showed no correlation with CAL (Table 3). Functional Disability and the number of swollen joints showed a significant correlation with oral hygiene status (Table 3).Mean number of missing teeth among RA patients was 5.22 (SD±5.38). DIS and ESR showed a significant correlation with the number of missing teeth (Table 3). Non parametric test was also done to test the association between variables as they were ranked based on severity. Patients with severe rheumatoid arthritis showed a significant association with periodontal disease (chi square 23.5, df 2,p value<0.001).Functional disability of the RA patients showed a highly significant association with oral hygiene status p value <0.01(statistics not shown).
DISCUSSION
In the past few years association between Rheumatoid Arthritis and Periodontal Disease has gained greater attention and numerous studies have been done, to establish this relationship, but results have been contradictory. Studies have put forth a significant association between RA and PD and that patients with moderate to severe periodontitis are at higher risk of suffering from Rheumatoid Arthritis and vice versa. In accordance with the previous studies9,12,1,15,16, the present study was done to determine the severity of periodontitis in patients with RA and to check whether there is a correlation between severity of periodontitis and Rheumatoid Disease Activity. The functional disability of the RA patient was also measured and correlated with their oral hygiene status. RA has a peak incidence in fourth and fifth decade of life7 , but can occur at any age, so patients aged 20-70 were selected for the current study. In this study, the number of female patients were more than males, this is as expected because RA has a higher prevalence among females7 , and our findings are in agreement with the previous studies. Secondary sjogrens syndrome more commonly develops in RA patients, it is characterised by dry eyes and xerostomia .The effect of xerostomia on the periodontium is controversial29, 30 hence patients giving a history of xerostomia were not included for the study. Only newly diagnosed RA patients not under treatment were included to eliminate the confounding effect of drugs like NSAIDS, DMARDS and steroid on the periodontium. Some patients were taking analgesics occasionally. NSAIDs have analgesic and anti inflammatory properties and have been shown to limit periodontal destruction31 similarly DMARDs are also anti inflammatory but their effect on the periodontium is uncertain. Glucocorticoids have been shown to induce secondary osteoporosis32, and osteoporosis has been shown to be a risk factor for periodontal disease. As the present study was carried out among the Indian population, Indian HAQ was utilised to measure physical disability, it was obtained by modification of the Multi Dimensional Health Assessment Questionnaire by Pincus et al. In the present study, there was no correlation between rheumatoid disease activity and clinical attachment loss, a probable indication that both the disease processes do not influence the progression of each other directly. Similarly, Addie et al16, Helminen et al33, Rosamma et al34 found no association between periodontitis status and measures of RA disease activity. It has been observed in the current study that majority of the patients had severe RDA and mild periodontitis .The results are in contrast to the findings by Mercado et al9 , Ishi et al17 , Pischon et al35 and similar to the findings by Sjostrom et al36, Basak et al37, Bozkurt et al38 , Yavuyilmaz et al39 that lesser periodontal destruction is seen among RA patients. Non parametric analysis showed that patients with severe Rheumatoid disease activity had a significant association with periodontal disease than moderate RDA patients, this is similar to the observation by Mercado et al9 . In our study, Indian HAQ was used to assess physical disability and it was significantly correlated with OHI indicating that, with increasing physical disability, the oral hygiene status of the patients deteriorated with more accumulation of plaque and calculus. This finding is unique for our study and could be crucial for establishing the relationship between functional disability, oral hygiene status and periodontal disease in patients with rheumatoid arthritis. Our analysis also showed that functional disability was not correlated with the severity of periodontal disease in agreement to the findings by Pischon et al35 but contradicting the findings of Mercado et al9 . Rheumatoid Factor contributes to tissue injury and tends to correlate with disease activity and severity in RA. Rheumatoid Factor titres and severity of RDA significantly correlated with the functional disability of the RA patients in this study suggesting that the functional disability of these patients were affected by the severity of RDA. Oral hygiene status of these patients showed a strong positive correlation with the clinical attachment loss. This implies that the poor oral hygiene status of these patients could be responsible for the periodontal destruction. Pischon et al35 in his study evidenced similar finding wherein plaque and gingival index markedly associated with CAL and accounted for 13.4% of association between RA and periodontal disease. Studies by Pischon et al35 , Ishi et al17, De Pablo et al40 have shown that RA patients have poor oral hygiene contrary to findings by Mercado et al9 , Abdelsalam et al41 . Our analysis showed that the number of missing teeth in these RA patients positively correlated with the clinical attachment loss. Those patients who had severe attachment loss had more number of missing teeth (mean 11.5) than those with lesser attachment loss (mean 4.3). Studies42,43 have reported that periodontitis and tooth mortality are closely associated and that tooth mortality on a lesser extent could be a predictor for attachment loss. Based on our findings we can suggest that severe periodontal destruction could have been a significant contributing factor for tooth loss in this sample but cannot be conclusive because patients could not clearly state the reason for tooth loss and there are multiple reasons for missing teeth like tooth decay, trauma, extraction for orthodontic treatment ,congenitally absent . The results from this study also indicated that patients with severe periodontitis had more number of missing teeth and elevated ESR. Ali Saad Thafeed Al Ghamdi44 in his study among chronic periodontitis patients showed that elevated level of ESR was seen in severe periodontitis patients and it positively correlated with the number of missing teeth. Currently the effect of such an association between ESR, tooth loss and periodontal destruction is uncertain. The strength of our study is that we used a composite index for RA disease activity(DAS 28), original OHI was used for oral hygiene status assessment hence all the teeth were assessed for debri and calculus rather than index teeth , and Indian HAQ was used for assessment of physical disability, which is more relevant for Indian population and shown to have high reliability and validity. Limitations of the study were cross sectional design, small sample size, osteoporosis a possible risk factor for periodontal disease was not excluded.
CONCLUSION
From the results of our study, it can be concluded that severe rheumatoid disease activity impairs the functional ability of the patients leading to difficulty in brushing their teeth and maintaining good oral hygiene which in turn leads to possible destruction of the periodontium and attachment loss. The periodontal destruction seen in these patients could be attributed to the poor oral hygiene due to limited dexterity rather than the RA disease process itself therefore RA patients should be educated on oral health and motivated to maintain good oral hygiene. Powered tooth brushes can be advised along with the use of chemical plaque control agent like mouthwash and consultation with a dentist or a Periodontist should be encouraged at frequent intervals. More number of longitudinal prospective cohort studies with larger sample size is needed, to further establish the relationship between both the disease activity and severity of rheumatoid arthritis and periodontal disease.
ACKNOWLEDGEMENT
Authors would like to acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to the authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Offenbacher S. Periodontal Diseases: Pathogenesis. Ann Periodontol 1996; 1: 821 – 878
2. Mattila,K.J.,Valtonen,V.V.,Nieminen,M.S. andAsikainen,S. Role of infection as a risk factor for atherosclerosis,myocardial infarction,and stroke. Clinical Infectious Diseases 1998; 26:719 -734
3. Grossi S.G,Genco R.J. Periodontal disease and diabetes mellitus: a two way relationship. Ann Periodontol 1998; 3:51-61
4. Scannapieco FA, Bush RB, Paju S. Associations between periodontal disease and risk for atherosclerosis, cardiovascular disease, and stroke: a systematic review Ann Periodontol 2003;8:38-53
5. Scannapieco FA, Bush RB, Paju S . Associations between periodontal disease and risk for nosocomial bacterial pneumonia and chronic obstructive pulmonary disease: A systematic review. Ann Periodontol 2003;8:54-69
6. Jeffcoat MK, Hauth JC, Geurs NC, Reddy MS, Cliver SP, Hodgkins PM, Goldenberg RL. Periodontal disease and preterm birth: results of a pilot intervention study.J Periodontol 2003; 74:1214-8
7. Harris,E.D.,Jr.Clinical features of Rheumatoid Arthritis.In:Textbook of Rheumatology,eds.Kelly,W.N.,Harris,E.D.and Sledge,C.B.,5thedition,1997.p898.Philadelph ia:WB Saunders
8. P.M.Bartold,R.I.Marshall,and D.R.Haynes.Periodontitis and Rheumatoid Arthritis: A Review.J Periodontol 2005;76:2066-2074
9. Mercado FB,Marshall RI,Bartold PM:Interrelationships between rheumatoid arthritis and periodontal disease.J Clin Periodontol 2003;30:761-772
10. Wegner,N.Wait R,Aroka A,Eick S,Nguyen K.A,Lundberg K,Kinloch A,Culshaw S,Potempa J andVenables P.J.Peptidylarginine deiminase from Porphyromonas gingivalis citrullinates human fibrinogen and alpha enolase implications for autoimmunity in rheumatoid arthritis.Arthritis Rheum 2010;62,2662 -2672
11. Moen K,Brun JG,Valen M,Skartveit L,Ribs Eribe EK,Olsen I,Jonsson R.Synovial inflammation in active rheumatoid arthritis facilitates trapping of a variety of oral bacterial DNAs.J Dent Res 2006;85:1074- 1078
12. Mercado FB,Marshall RI,Klestov AC, and Bartold PM.Is there a relationship between rheumatoid arthritis and periodontal disease.J Clin Periodontol 2000;27:267-272
13. Dumitrescu AL.Ocurrence of self reported systemic medical conditions in patients with periodontal disease.Rom J Intern Med 2006;44:35-48
14. Mercado FB,Marshall RI,Klestov AC, and Bartold PM.Relationship between rheumatoid arthritis and periodontitis.J Periodontol 2001;72:779-787
15. Eduardo de Paula Ishi,Manoel Barros Bertolo,Carlos Rossa Jr,Keith Lough Kirkwood,Mirian Aparecida Onofre.Periodontal condition in patients with rheumatoid arthritis. Braz Oral Res 2008;22:72-77
16. Addie Dissick, Robert S. Redman,Miata Jones, Bavana V. Rangan, Andreas Reimold, Garth R. Griffiths,Ted R. Mikuls, Richard L. Amdur, John S. Richards, and Gail S. Kerr..Association of Periodontitis With Rheumatoid Arthritis: A Pilot Study.J Periodontol 2010;81:223-230
17. Ribeiro J,Leao A,Novaes AB.Periodontal infection as a possible severity factor for rheumatoid arthritis.J Clin Periodontol 2005;32:412-416
18. Anne Havemose-Poulsen, Jytte Westergaard, Kaj Stoltze, Henrik Skjødt, - Bente Danneskiold-Samsøe, Henning Locht, Klaus Bendtzen, and Palle Holmstrup.Periodontal and hematological characteristics associated with aggressive periodontitis, Juvenile idiopathic arthritis, and rheumatoid arthritis J Periodontol 2006; 77:280-288
19. Al Katma MK,Bissada NF,Bordeaux JM:Control of periodontal infection reduces the severity of active rheumatoid arthritis J Clin Rheumatol 2007;13:134-137
20. Ortiz P,Bissada N.F,Palomo L,Han Y.W,AlZahrani M.S,Paneerselvam A and Askari A.Periodontal therapy reduces the severity of active rheumatoid arthritis in patients treated with or without tumor necrosis factor inhibitors J Periodontol 2009; 80:535-540
21. Demmer RT,Molitor JA,Jacobs DR Jr,Michalowicz BS.Periodontal disease ,tooth loss and incident rheumatoid arthritis :results from the first National Health and Nutrition Examination Survey and its epidemiological follow – up study. J Clin Periodontol 2011;38:998-1006
22. Molitor J.A,Alonso A,Wener M.H,Michalowicz B.S,Beck J.D,Gersuk V.H,Buckner J.H and Folsom A.R.Moderate to severe adult periodontitis increases risk of rheumatoid arthritis in non smokers and is associated with elevated ACPA titres. The ARIC study. Arthritis Rheum 60.S433
23. Arkema EV,Karlson E.W and Costenbader KH.A prospective study of periodontal disease and risk of rheumatoid arthritis.J Rheum 2010;37:1800-1804
24. Arnett FC,Edworthy SM,Bloch DA et al.The American Rheumatism Association1987 revised criteria for the classification of rheumatoid arthritis.Arthritis Rheum 1988;31:315-324
25. Page RC,Eke PI.Case definitions for use in population based surveillance for Periodontitis.J Periodontol 2007;78:1387- 1399.
26. Kumar A, Malaviya AN, Pandhi A. Validation of an Indian version of the Health Assessment Questionnaire in patients with rheumatoid arthritis. Rheumatology 2002;42:1457-9
27. Gary C Armitage.Development of a classification system for periodontal diseases and conditions.Ann Periodontol 1999;4:1-6
28. Greene JC, Vermillion JR. The oral hygiene index: a method for classifying oral hygiene status. J Amer Dent Ass 1960; 61: 29-35
29. Najera MP,Al-Hashimi I,Plemons JM,Rivera-Hidalgo F,Rees TD,Haghighat N et al.Prevalence of periodontal disease in patients with Sjogren‘s syndrome.Oral Surg Oral Med Oral Pathol Oral Rasdiol Endod 1997;83:453-457
30. Raquel Pippi Antoniazzi, Letícia Algarves Miranda, Fabricio Batistin Zanatta, Alexandre Garcia Islabao, Anders Gustafsson, Geraldo Augusto Chiapinotto, and Rui Vicente Oppermann. Periodontal Conditions of Individuals With Sjögren's Syndrome J Periodontol 2009;80:429-435
31. Williams RC.Non steroidal anti inflammatory drugs for altering periodontal bone loss.J Dent Res 1999;78:638-641.
32. McIlwain HH. Glucocorticoid-induced osteoporosis: pathogenesis, diagnosis, and management. Prev Med. 2003 Feb;36:243-9.
33. Helminen-Pakkala E.Periodontal conditions in rheumatoid arthritis.A clinical and roentenological investigation.Part two.The study in rheumatoids.Proc Finnish Dental Soc 1971;Suppl IV :1-108
34. Rosamma Joseph, Sreeraj Rajappan, Sameera G. Nath and Binoy J. Paul.Association between chronic periodontitis and rheumatoid arthritis: a hospital-based case–control study. Rheumatology International, Online First™, 6 January 2012
35. Pischon N,Pischon T,Kroger E,Glumez BM,KleberJP,Bernimoulin H,Landau PG,Prinkman P,Schlattman J,Zernicke F,Detert J.Association among RA,oral hygiene and Periodontitis J Periodontol 2008 ;79:979-986
36. Sjostrom L, Laurell L, Hugoson A and Hakansson JP.Periodontal Conditions in adults with rheumatoid arthritis.Community Dent Oral Epidemiol 1989 : 17 : 234 – 236
37. Biyikoglu B, Buduneli N, Karde?ler L, Aksu K, Pitkala M, Sorsa T.Gingival crevicular fluid MMP-8 and -13 and TIMP-1 levels in patients with rheumatoid arthritis and inflammatory periodontal disease.J Periodontol. 2009 ;80:1307-14
38. Bozkurt FY, Berker E, Akku S, Bulut S. Relationship between IL-6 Levels in gingival crevicular fluid and periodontal status in patients with Rheumatoid Arthritiis and Adult Periodontitis.J Periodontol 2000:71:1756-1760
39. Yavuzyilmaz E, Yamalik N, Calguner M, Ersoy F, Baykara M, Yeniay I.Clinical and Immunological Characteristics of patients with RA and Periodontal disease .J Nihon Univ Sch Dent : 1992 : Jun : 34 (2) : 89-95
40. Paola De Pablo, Thomas Dietrich, Timothy E McAlindon. Association of periodontal disease and tooth loss with rheumatoid arthritis in the US population. J Rheumatol 2008; 35: 70-76
41. Safa K Abdel salam,Nada T Hashim,Emitithal M Elsalamabi and Bakri G Gismalla.Periodontal status of rheumatoid arthritis patients in Khartoum state.BMC Research Notes 2011;4:460
42. Hujoel PP , Löe H, Anerud A, Boysen H , Leroux BG. The Informativeness of Attachment Loss on Tooth Mortality.J Periodontol 1999; 70: 44-48
43. Philippe Bouchard, Pierre Boutouyrie, Catherine Mattout, Denis Bourgeois Risk Assessment for Severe Clinical Attachment Loss in an Adult Population.J Periodontol 2006; 77: 479-489
44. Ali Saad Thafeed Al Ghamdi. Effect of chronic periodontal diseases on Erythrocyte Sedimentation Rate. Egypt Dent J 2009;55 :2641
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License