IJCRR - 4(12), June, 2012
Pages: 48-54
Date of Publication: 22-Jun-2012
Print Article
Download XML Download PDF
BLOOD AND COMPONENTS USAGE IN A TERTIARY CARE HOSPITAL
Author: Mallikarjuna Swamy C M, Shashikala P, Kavita G U
Category: Healthcare
Abstract:Background: Availability of blood for transfusion, its need, quality and safety of blood transfusion depends on the geographical location as well as state of medical care in that area. Misuse or overuse of this naturally available resource has to be avoided. Aim: To review blood component usage and to assess the pattern of blood usage in a tertiary care hospital. Materials and methods: This study was conducted at a blood bank of a tertiary health care hospital. Details of the blood and component recipients in one representative month were recorded. Results: Supply of blood was found to be more in the surgical wards forming 57.36% (n=343/598) of total supply. The most common diagnosis for patients requiring blood transfusion was anemia (n=157, 26.25%). Anemia (353/620, 56.93 %) was also the most common indication for packed red blood cells (PRBCs) transfusion followed by surgery (194/620, 12.24%). Thrombocytopenia was the commonest indication for platelet transfusion (378/514, 23.85%). Highest number of fresh frozen plasma (FFP) units was utilized for patients with hypoproteinemia (79/166, 45.78%). Our audit shows that the use of PRBCs has largely replaced that of whole blood. Conclusion: Appropriate guidelines need to be set to reduce the inappropriate transfusions of blood components like PRBCs, platelets, and FFP. The clinician should always bear in mind that transfusion can lead to serious complications and benefit/risk assessment must be taken into account before each transfusion.
Keywords: Blood utilization audit, transfusion appropriateness, transfusion practices.
Full Text:
INTRODUCTION
Transfusion medicine has become one of the sophisticated medical technical discipline, that has eased modern medical therapy. Blood transfusion is done in all parts of the world. Availability of blood for transfusion, its need, quality, safety of blood transfusion depends on the geographical location as well as state of medical care in that area. As the supply of red blood cells continues there is an increasing demand for platelets. Since blood is considered as a drug, it is regulated by Food and Drug Administration. As any other drug, blood transfusion may cause side effects like transfusion reactions, transmit infections etc., everyone must be aware of the potential risks of blood transfusion. Blood transfusion is considered as similar to tissue transplantation. Keeping in mind the graft versus host reaction, blood must be ordered and transfused only when it is absolutely necessary. Misuse or overuse of this naturally available resource has to be avoided. Review of blood component usage has to be undertaken to assess the pattern of blood usage in any hospital. Hence the present was study was undertaken.
MATERIALS AND METHODS
This study was conducted at a blood bank of a tertiary health care hospital. The number of all whole blood units and blood components supplied over a period of one year was recorded and their average was calculated. Data of one month, which was closest to the average blood supply in one year, was chosen as a representative month. All the details of the blood and component recipients in this representative month were recorded, including age, gender, ABO and Rhesus blood groups, address, consultant in-charge, ward/unit where patients were admitted, diagnosis along with indications for blood transfusion. History of previous and present illness, including any previous transfusions and transfusion reactions if any were noted. Reports of salient investigations like hemoglobin, platelet count and coagulation profile were recorded. Details of usage of blood including the number and type of components transfused were noted and correlated with the clinical diagnosis and indications for transfusion.
RESULTS
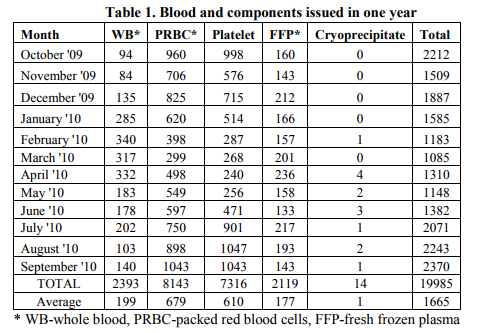
The total number of whole blood and components issued from our blood bank in one year (1st October 2009 to 30th September 2010) was 19,985 units, with a monthly average of 1665 units. The supply showed some seasonal variation, with lesser unit supplied around midyear and peak during year ends (Table 1). For this study data was collected for a month (January 2010) the blood supply of which (n=1585 units) was closest to the calculated monthly average (n=1665 units), to account for seasonal variation in blood demand. In that representative one month the number of requests for blood products was from 598 patients, with many of these requests being more than one unit. The break-up supply for whole blood and various components showed that PRBC was the maximum utilized product followed by platelets, whole blood and FFP (Table 1).
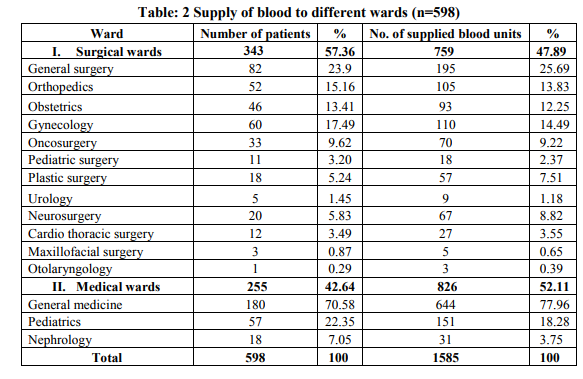
Supply of blood was found to be more in the surgical wards forming 57.36% (n=343/598) of total supply; maximum blood required for general surgery (n=82/343, 23.9%). Request for medical wards constituted 42.64% (n=255/598) of all demands, with highest requirement in general medicine wards (n=180/255, 70.58%) (Table: 2).
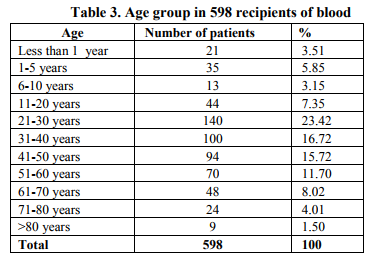
Youngest recipient of blood unit was one day (two males and one female neonate) and the oldest was 95 year old male. Largest number of patients were in the age group 21-60 years (n=404/598, 67.55%) (Table 3). Male to female ratio was 0.89:1(Table 4).

The most common diagnosis for patients requiring blood components was anemia (n=157, 26.25%); followed by elective surgery (n=86, 14.38%) and dengue-like illness/viral fever (n=70, 11.7%) (Table 6).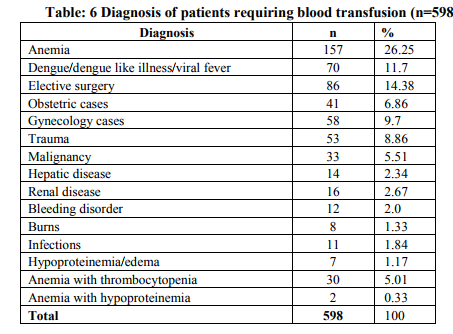
Among the indications for all blood components taken together, anemia was the common indication (n=491, 30.98%) followed by thrombocytopenia (405, 25.56%) and elective surgery (353, 22.27%) (Table 7)

Among the 1585 units supplied to 598 patients, PRBCS was the maximum issued component (620/1585, 39.11%), followed by platelets (514/1585, 32.42%), whole blood (285/1585, 17.98%) and FFP (166/1585, 10.47%). Anemia (353/620, 56.93 %) was most common indication for PRBCs transfusion followed by surgery (194/620, 12.24%). Thrombocytopenia was the commonest indication for platelet transfusion (378/514, 23.85%) followed by anemia with thrombocytopenia and surgical procedures. Surgical procedures (126/285, 44.21%) were the commonest indication for whole blood transfusions followed by anemia (123/285, 43.15%). Highest number of FFP units was used for patients with hypoproteinemia (79/166, 45.78%).
DISCUSSION
Blood and blood components are no longer considered to be a low or no risk procedure, and consequently an increasing need for stricter guidelines for transfusing blood products has been recognized, not just to check infections, but also to minimize other side effects of transfusion.1 Whole blood and blood components are considered as drugs by the Food and Drug Administration (FDA) and the main aim of any blood bank is to provide safe and effective blood and blood components to the patients.2 To fulfill the demands of the blood, we need to know about the trends of blood usage and the ordering pattern in the hospital. Also it helps us to set policies in place to improvise the transfusion services. In our audit we found that blood components utilized in the hospital showed a ratio of PRBC: platelet: whole blood: fresh frozen plasma as 3.1:2.57:1.425:0.83 and whole blood: PRBCs was 3.77:1.11 which is different from most of the other studies that show whole blood to PRBC ratio as 1:3 or less.2 The utility or demand of blood and blood components was higher in patients admitted to surgical wards (57.36%) compared to medical wards (42.64%). Similar observation is reported from many other studies.2 Higher utility in surgical wards was probably because, blood and blood components are often ordered due to anticipated blood loss rather than actual blood loss, thereby leading to overuse of blood and unnecessary exposure of patients to antigens and infections. Another reason for increased usage of blood in surgical wards could be for the correction of anemia detected prior to surgery in patients requiring surgeries. According to studies, there is mounting evidence that some of the blood that is transfused is not always clinically indicated.3 Among all 598 patients who required transfusion, anemia was found to be the commonest indication (26.25%) similar to other studies.2 Of the 1585 units issued to 598 patients, PRBC was the maximum utilized component (39.11%) in our audit which is dissimilar to other studies that indicate more utilization of whole blood.2,4 Unnecessary transfusion of PRBCs could be avoided by alternative means like appropriate diet and hematinic therapy wherever possible. In both Medical and Surgical wards, it is necessary to correlate the clinical condition of the patient and the trigger values of hemoglobin and hematocrit in blood transfusion in anemic patients. Platelets were the second most commonly used blood component for transfusion 32.42% (514/585). The most common indication for platelet transfusion in our audit was thrombocytopenia (25.56%) possibly because Davangere happens to be an endemic area for dengue and dengue like illness. Indications for platelet transfusion are a count of < 20,000 /mm3 or among patients requiring surgery in less than 12 hours, a platelet count of < 50,000 /mm 3 could be the trigger level. Some studies indicate that platelet count of up to 10,000/cu.mm could be safe and platelet transfusion could be avoided.5 Indication for whole blood transfusion are patients with acute bleeding, trauma (large volume blood loss > 25%) and surgical patients, cardiac surgery and exchange transfusion in infants.4 In our audit, use of whole blood was 17.98%, maximum use was in patients undergoing surgery ( 126/285, 44.21%) followed by patients with anemia (123/285, 43.16%). The utilization of whole blood in the latter case could be replaced by PRBC wherever possible. FFP was the least used component (10.47%) in our audit, commonest indication for its transfusion being hypoproteinemia (45.78% 79 out of 166). Though least used, some of the transfusions of FFP were also found to be inappropriate. It is often used as a volume expander and a source of albumin.6 FFP should not be used for intravascular volume expansion, correction/ prevention of protein malnutrition, and when specific factor concentrates are available; alternative products that have undergone viral inactivation through complex manufacturing processes are preferable.7 In case of FFP, it is recommended to transfuse 5-6 units to correct the haemostatic defect due to clotting factor deficiency. Many times only one or two units are transfused. Many reports show inappropriate use of FFP at various centres. 8,9,10,11,12 CONCLUSION With the availability of blood component treatment, the clinicians are posed with a wide variety of choices. Inadequate and variable level of knowledge about transfusion practices among doctors increases the potential for misuse of blood.
Though the transfusion trends in our audit may not be representative of other hospitals, assessment of local transfusion practice is essential. Our audit shows that the use of PRBCs has largely replaced that of whole blood. More attempts must be made through frequent seminars and clinical meets to educate clinicians to limit the use of whole blood to only cardiac patients and acute trauma patients. Appropriate guidelines also need to be set to reduce the inappropriate transfusions of blood components like platelets, and FFP. The clinician should always bear in mind that transfusion can lead to serious complications and benefit/risk assessment must be taken into account before each transfusion.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Jain R, Jose B, Cashic P, Agarwal R, Deorari AK. Blood and blood component therapy in neonates. Indian J Pediatr 2008;75(5):489-95.
2. Gaur DS, Negi G, Chauhan N, Kusum A, Khan S, Pathak VP. Utilization of blood and blood components in a tertiary care hospital. Indian J Hematol Blood Transfus 2009;25(3):91-5.
3. Audet A, Goodnough LT, Parvin CA. Evaluating the appropriateness of red blood cell transfusions: the limitations of retrospective medical record reviews. International Journal for Quality in Health care 1996;8(1):41-9.
4. EFE S, Demir C, Dilek I. Distribution of blood and blood components, indications and early complications of transfusion. Eur J Gen Med 2010;7(2):143-9.
5. Greeno E, McCullough J, Weisdorf D. Platelet utilization and transfusion trigger: a prospective analysis. Transfusion 2007;47:201-5.
6. Wade M, Sharma R, Manglani M. Rationale use of blood components- an audit. Indian J Hematol Blood Transfus 2009;25(2):66-9.
7. Uppal P, Lodha R, Kabra SK. Transfusion of blood and components in critically ill children. Indian J Pediatr 2010;77:1424-8.
8. Thomson A, Contras M, Knowles S. Blood component treatment: A retrospective audit in five major London hospitals. J Clin Pathol 1991; 44:734-7.
9. Chang WJ, Tan MK, Kuperan P. An audit of fresh frozen plasma usage in an acute general hospital in Singapore. Singapore Med Jv2003; 44(11):574-8.
10. Schofield WN, Rubin GL, Dean MG. Appropriateness of platelet, fresh frozen plasma and cryoprecipitate transfusion in New South Wales public hospitals. MJA 2003;178:117-21.
11. Shinagare SA, Angarkar NN, Desai SR, Naniwadekar MR. An audit of fresh frozen plasma usage and effect of fresh frozen plasma on the pre-transfusion international normalized ratio. Asian J Transf Sci 2010; l4(2):128-32.
12. Makroo RN, Raina V, Kumar P, Thakur UK. A prospective audit of transfusion requests in a tertiary care hospital for the use of fresh frozen plasma. Asian J Transfus Sci 2007; 1:59-61.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License