IJCRR - 4(12), June, 2012
Pages: 27-35
Date of Publication: 22-Jun-2012
Print Article
Download XML Download PDF
MYOEPITHELIOMA OF THE PAROTID GLAND: A CASE REPORT
Author: Atul Jain, Pragnesh Parmar
Category: Healthcare
Abstract:The present paper describe the clinical and pathologic feature of a benign myoepithelioma of parotid glad. Through 1985, only 42 other cases have been reported in the literature, 3 malignant and 39 benign. Fewer than 100 cases had been reported through 1993. The number of case report of myoepitheliomas is increasing as pathologist have become more aware of their existence. This uncommon tumor is most
commonly diagnosed in parotid gland and in the minor salivary glands of palate. The complex and varied
morphologic expression of neoplastic myoepithelium have attracted numerous investigators who have presented valuable but often contradictory data. In our opinion these tumors are still a rare variety because they are simply not well recognized. Together with the review of literature, consideration are presented on the clinical evaluation, differential diagnosis and treatment of this lesions.
Keywords: Parotid gland, Salivary gland, Neoplasm, Myoepithelioma
Full Text:
INTRODUCTION
Salivary gland neoplasms composed exclusively of myoepithelial cells (myoepitheliomas) are unusual and intriguing. Salivary Gland tumors are quite uncommon and comprise less than 3% of all neoplasm of head and neck region. [1] Among the salivary gland tumors, myoepithelioma comprise only 1 – 1.5%. [1, 2, 4] It commonly occurred in the parotid gland and few are located in oral cavity. [3, 4] Majority of Myoepitheliomas, described in literature are benign. [5] Peak age of occurrence is between 3rd – 4 th decade of life and both sexes are equally affected. [6, 7] In 1943, Sheldon was the first to classify tumors as myoepitheliomas when he categorized three such tumors in a review of 57 mixed tumors of the salivary glands. [7] Initial diagnostic criteria for benign myoepithelioma were based on the review of Barnes et al. [2] and Sciubba and Brannon. [3] The traditional definition included only solid (without myxochondroid elements) tumors containing either spindle or plasmacytoid cells. However, with the recent appreciation of the diverse phenotypic and ultra structural modifications exhibited by the neoplastic myoepithelial cells of different salivary gland tumors, the morphologic spectrum of myoepithelioma has expanded. Usually in such cases patient underwent partial parotidectomy and specimen sent for Histopathological examination which was diagnosed as Myoepithelioma of parotid gland.
CASE REPORT
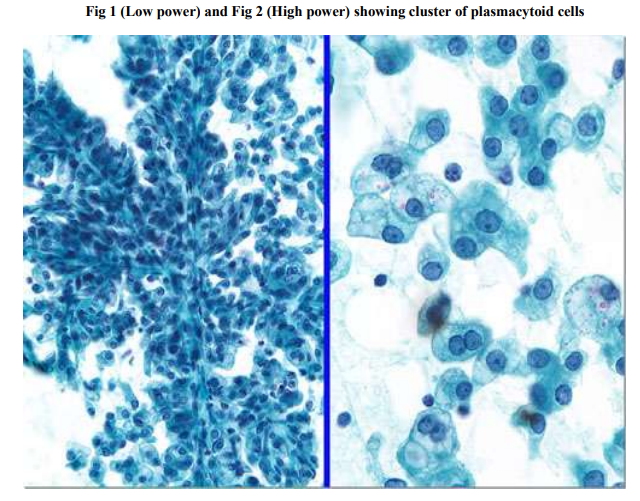
We are presenting here a case of 40 years old woman presented in our hospital with painless swelling in the right side of her face for past 6 months. On examination, a well demarcated, firm mass of 4 X 2 cm in the right parotid region was palpated. The mass was well demarcated, and it had a smooth external appearance. It had a moderately firm consistency, fixed to neighbouring tissues and no pain on palpation. The oral cavity was normal on inspection. There was no associated facial weakness or cervical lymphadenopathy. Clinical diagnosis made as plemorphic adenoma and sent for Fine needle aspiration cytology. Fine needle aspiration cytology Showed sheets of plasmacytoid cells and spindle shaped cells arranged in clusters and nuclei were small and oval with homogenous chromatin. (fig.1, fig.2) Under general anaesthesia, a nodular wellcircumscribed mass was surgically excised with a surrounding supra facial portion of normal parotid gland. Right partial parotidectomy was done and specimen sent for Histopathological Examination.
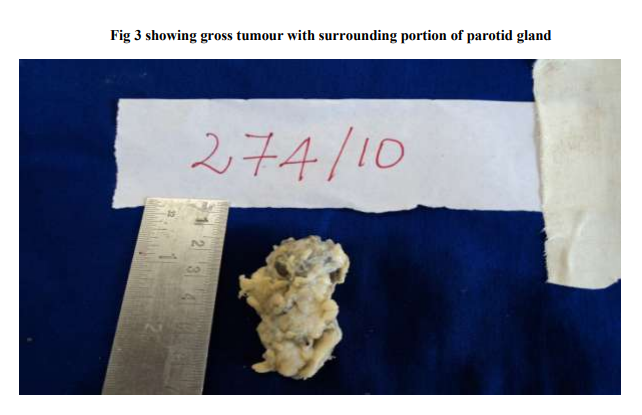
Gross Examination
• Tumor with surrounding normal portion of parotid gland was measured about 4.5 X 3.5 X 1.5 cm (fig.3)
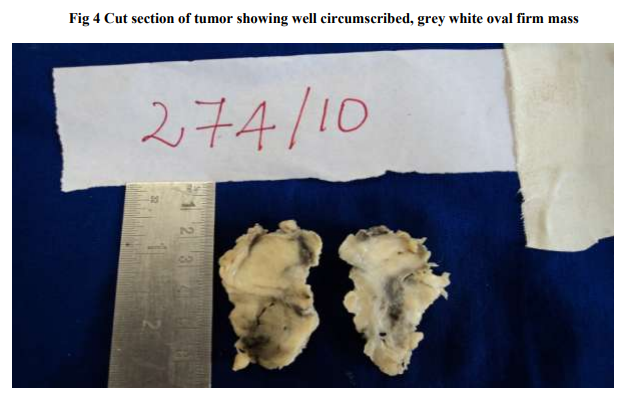
• Cut section showed well circumscribed, gray white, oval firm mass measuring 3.5 X 1.5 cm (fig.4)
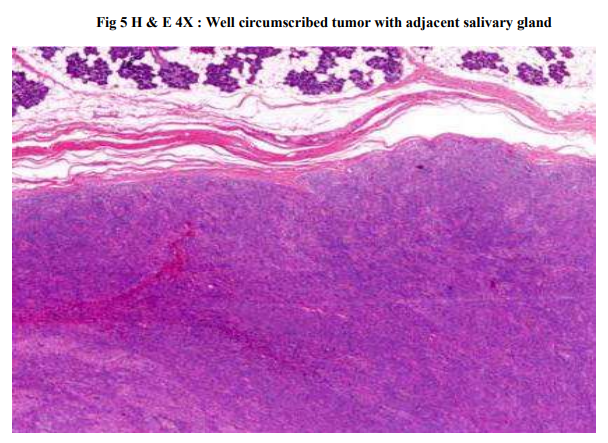
Histopathological Examination
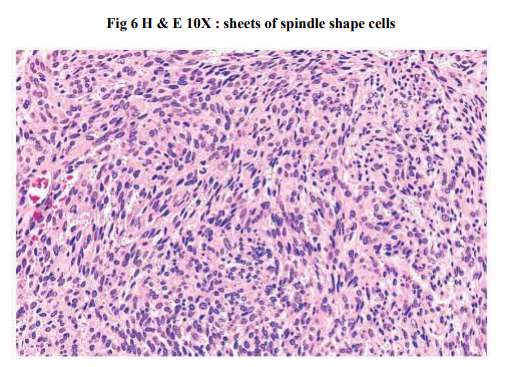
• Showed the encapsulated tumor was hypercellular & composed of sheets of round to oval cells and spindle shaped cells.(fig.5, fig.6)
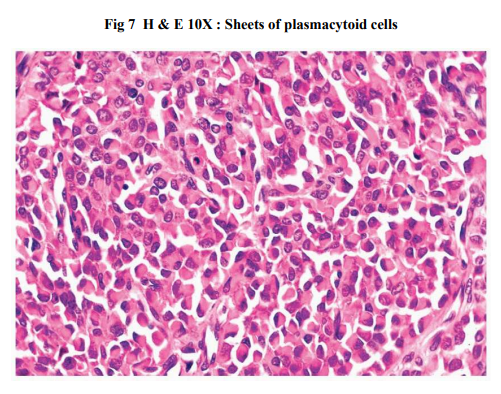
• Few plasmacytoid cells with oval nuclei and eosinophilic cytoplasm were seen.(fig.7, fig.8)
The tumor had a fascicular cellular arrangement with poor intercellular stroma. There was no necrosis, cellular atypia, or mitosis. Stroma was hyalinized at places. Postoperatively, there was no facial paralysis. There was no evidence of disease at one year follow-up.
DISCUSSION
Myoepitheliomas account for less than 1.5% of all salivary gland tumors. A review of the literature through 1993 yielded approximately 100 cases. [8] The tumor appears to be rare, and this contrast with the active role of myoepithelial cells in the histogenesis of several type of salivary gland tumors. The number of case reports is increasing as pathologists have become more aware of its existence. The most common location of myoepithelioma of the head and neck are the parotid gland (40%) and the palate (21%). [2, 9] The age and sex distribution of myoepitheliomas is similar to that of mixed tumors. There are no distinctive clinical features and similar to most other salivary gland tumors, myoepitheliomas present as asymptomatic, slowly growing masses. Parotid lesions never cause facial nerve dysfunction or cervical lymphadenopathy and those of the palate rarely ulcerate. Fine needle aspiration cytology is a baseline investigative tool in the assessment of patients with salivary gland swellings. It is an accurate method of distinguishing neoplastic from non neoplastic lesions. It may not be possible to always accurately predict a specific tumor type due to the overlapping spectrum of cytological appearances found in a wide variety of salivary gland neoplasms. [6, 8] Usually peak age of occurrence is between 3rd and 4th decade of life. In this case 40 year old woman, presented with tumor.
Macroscopically, myoepitheliomas appear as well circumscribed, frequently encapsulated tumors that show no features distinct from mixed tumors except for the absence of grossly myxoid or chondroid areas. Myoepithelioma usually ranges from 1 to 5 cm in diameter. In our case tumor measures 3.5 X 1.5cm which is well demarcated with smooth external appearance. [6, 8] Grossly, myoepitheliomas have solid, tan or yellow–tan glistening cut surface. In our case gray white, oval firm mass is present. Parotid myoepitheliomas are usually encapsulated, whereas those arising in the minor salivary glands may not demonstrate a capsule. Microscopically, they show three morphologic patterns. Spindle cell pattern is most common and consist of a proliferation of spindle shaped cells with eosinophilic cytoplasm. These may be arranged in diffuse sheets or interlacing fascicles. Tumors are hypercellular and have limited myxoid or mucoid stroma. The plasmacytoid pattern shows groups of round cells with eccentric nuclei and eosinophilic often hyaline appearing cytoplasm. These may be present in sheets of closely packed cells or in groups of cells separated by a loose myxoid stroma. The third pattern shows a combination of plasmacytoid and spindle-shaped cells. The spindle cell pattern is most common in parotid tumors. In our case combination of plasmacytoid and spindle cell pattern was present. [9, 10] Myoepithelioma distinguished from pleomorphic adenoma as relative lack of ducts and absence of myxochondroid areas. The rarity of myoepithelioma and the varied phenotypic expression of myoepithelial cells may cause problems in diagnosis. Tumors consisting predominantly of spindle shaped myoepithelial cells may be difficult to differentiate from mesenchymal lesions such as fibrous histiocytoma, schwannoma or leiomyoma. Ultrastructurally, they were composed of a single cell population characterized by numerous cytoplasmic filaments, duplicity of the basement membrane material and the characteristic cytoplasmic appearance of myoepithelial cells. [10] Immunohistochemistry is usually done to differentiate between clear cell variant of myoepithelioma from other clear cell tumors of salivary gland. Muscle specific actin marker is strongly positive in other clear cell tumors whereas negative in clear cell variant of myoepithelioma. In our case there were no clear cells. With immunocytochemical techniques, myoepithelial cells stain positive for cytokeratin, muscle specific actin, occasionally express S100 protein and glial fibrillary acidic protein (GFAP). Desmin has not been demonstrated. The neoplastic myoepithelial cells consistently demonstrate cytokeratin, S100 and muscle specific actin, whereas the immunoreactivity for vimentin and GFAP is more variable. [11] Identification of myoepithelial tumors as either benign or malignant on histological ground is difficult. The criteria for a diagnosis of malignancy are the presence of cytologic abnormalities, an increased mitotic rate, and particularly an invasive growth pattern. [12] These criteria were not met in our case. According to the World Health Organization‘s classification of salivary gland tumors, ??Myoepitheliomas are characterized by a more aggressive growth pattern than pleomorphic adenomas. [12, 13] But some authors have found that the biological behaviour of myoepitheliomas appears to parallel that of the pleomorphic adenoma. [2, 8] Others believe that myoepitheliomas are monomorphic variants of mixed tumors. [3, 14]
It is our opinion, as well as that of Barnes et al [2] and Dardick et al [15] that salivary adenomas are a part of a spectrum, with monomorphic adenoma and myoepithelioma at the extremes and a wide range of pleomorphic adenomas in between, depending on the type and degree of gene expression that is coupled with neoplastic transformation. While distinguishing benign myopithelioma from benign pleomorphic adenoma may primarily be of academic interest. Benign myoepitheliomas should be carefully differentiated from malignant tumors, such as malignant myoepithelioma, mucoepidermoid carcinoma, and spindle cell squamous carcinoma. [3, 16] Surgery is the first choice of treatment for myoepithelial carcinomas. The high recurrence rate suggests that initial surgery should be radical with sufficient normal tissue margins. Adjuvant chemotherapy and radiotherapy have not been found helpful for treating these carcinomas. Treatment of benign myoepitheliomas are similar to that of mixed tumors and consist of complete surgical removal. Most myoepitheliomas have a benign course with minimal tendency of recurrence. Treatment for a benign salivary gland tumor is surgical excision with a margin of normal uninvolved tissue being included. The recurrence rate is similar to that of the pleomorphic adenoma. [3, 17] The prognosis of benign myoepitheliomas is quite favourable, but patients should undergo regular follow-up examinations to rule out local recurrence.
CONCLUSION
Myoepithelioma occurs in most major and minor salivary gland tissues, and it is generally a biologically benign lesion. By means of this case report, we have attempted to scrutinize this entity. The variability of the histopathologic structure of mixed tumors and the alteration of the histochemical characteristics of myoepithelial cells in tumors from those of normal glands made identification of tumor myoepithelial cells difficult and uncertain. However, ultrastructural study of myoepithelial cells established fine structural criteria on which positive identification could be made. While myoepithelioma has no specific clinical features, it is accepted pathologically as a distinct entity. Treatment for a benign salivary gland tumor is surgical excision with a margin of normal uninvolved tissue being included. The recurrence rate is similar to that of the pleomorphic adenoma (15–18%).
References:
1. Kawashima Y, Kobayashi D, Ishikawa N, Kishimoto S, A case of myoepithelioma arising in an accessory parotid gland, The Journal of Laryngology and Otology, 2002; 116:474–6.
2. Barnes L, Appel BN, Perez H, El-Attar AM, Myoepithelioma of the head and neck: Case report and review, European Journal of Surgical Oncology, 1985; 28:21–8.
3. Sciubba JJ, Brannon RB, Myoepithelioma of salivary glands: Report of 23 cases. Cancer 1982; 49:562–72.
4. Morinie`re S, Robier A, Machet MC, Beutter P, Lescanne E, Massive infra clinic invasion of the facial nerve by a myoepithelial carcinoma of the parotid, International Journal of Pediatric Otorhinolaryngology, 2003; 67:663–7.
5. Savera AT, Sloman A, Huvos AG, Klimstra DS, Myoepithelial carcinoma of salivary glands: A clinicopathologic study of 25 patients, The American Journal of Surgical Pathology, 2000; 24(6):761–74.
6. Dean A, Sierra R, Alamillos FJ, LopezBeltran A, Morillo A, Are´valo R et al. Malignant myoepithelioma of the salivary glands: Clinicopathological and immunohistochemical features, British Journal of Oral and Maxillofacial Surgery, 1999; 37:64–6.
7. Sheldon WH, So called mixed tumors of the salivary glands, Archives of Pathology and Laboratory Medicine, 1943; 35:1–20.
8. Turgut S, Cekic A, Ergu¨l G, Aksoy F, Seckin S, O¨zdem C, Myoepithelioma of the parotid gland: A report of two cases, Ear Nose and Throat Journal, 2001; 80(3):155–8.
9. Waldron CA, Mixed tumor (pleomorphic adenoma) and myoepithelioma. In: Ellis GL, Auclair PL, Gnepp DR, editors. Surgical pathology of the salivary glands. Philadelphia: WB Saunders; 1991. Page 165–86.
10. Leifer C, Miller AS, Putong PB, Harwick RD, Myoepithelioma of the parotid gland. Archives of Pathology and Laboratory Medicine, 1974; 98:312–9.
11. Franke WW, Schid E, Freudenstein C, et al. Intermediatesized filaments of the prekeratin type in myoepithelial cells, The Journal of Cell Biology, 1980; 84:633–54.
12. Di Palma S, Guzzo M, Malignant myoepithelioma of salivary glands: Clinicopathological features of ten cases. Virchows Archiv. A, Pathological anatomy and Histopathology, 1993; 432:389–96.
13. Dardick I, Thomas MJ, Van Nostrand AW, Myoepithelioma — new concepts of histology and classification: A light and electron microscopic study, Ultrastructural Pathology, 1989; 13:187–224.
14. Batsakis JG, Myoepithelioma. Annals of Otology, Rhinology and Laryngology, 1985; 94:523–4.
15. Dardick I, Van Nostrand AW, Phillips MJ, Histogenesis of salivary gland pleomorphic adenoma (mixed tumor) with an evaluation of the role of myoepithelial cell, Human Pathology, 1982; 13:62–75.
16. Nayak JV, Molina T, Smith JC, Branstetter BF, Hunt JL, Snyderman CH, Myoepithelial neoplasia of the submandibular gland: Case report and therapeutic considerations, Archives of Otolaryngology, Head and Neck Surgery, 2003; 129:359–62.
17. De Stefani A, Lerda W, Bussi M, Valente G, Cortesina G, Tumors of the parapharyngeal space: Case report of clear cell myoepithelioma of the parotid gland, Acta Otorhinolatyngol Ital, 1999; 19:276– 82.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License