IJCRR - 4(13), July, 2012
Pages: 16-24
Date of Publication: 18-Jul-2012
Print Article
Download XML Download PDF
COMPREHENSIVE ORAL REHABILITATION OF CLEFT LIP AND PALATE PATIENTS
Author: Savitha Sathyaprasad
Category: Healthcare
Abstract:Cleft lip and palate is one of the most common birth defect with incidence of 1 in 600 births and causes severe facial deformity adversely affecting the self esteem of the child if treatment is not initiated in appropriate time. There has been a robust growth in the treatment of Cleft lip and palate with intricate interconnections of different multi specialities who deliver the treatment in the most seamless way. The purpose of this review article is to illustrate the various dental treatment modalities that can be delivered on a cleft child from birth to adolescence in the overall rehabilitation.
Full Text:
INTRODUCTION
Cleft of lip and palate are immediately recognizable disruption of normal facial structure accounting approximately one in 600 new born babies1 and over 300 syndromes are known to have clefting of the lip or palate as an associated feature.2 It causes considerable morbidity, impose a substantial financial risk for family with a concomitant societal burden. These patients may experience problem with feeding, speaking, hearing, and social integration which can be corrected to various degree by surgery, dental treatment, speech therapy and psychologic intervention. The treatment protocol of a cleft lip cleft palate patient is unique and needs a smooth delivery of optimum expertise of various specialties in an intricate seamless way, because treatment delivered by one specialty may hamper or interfere in the treatment of other specialty. Team approach to patients with craniofacial anomalies which includes coordination with oral and maxillofacial surgeons, ENT specialists, obstetricians, speech pathologist, paediatricians, psychologist, ophthalmologist and the nursing staff. Pedodontist role in the multidisciplinary team approach is very important as a specialist being trained in every aspect of child from physiology to psychology their active role in early intervention in overall management is highly recommended. The purpose of this paper is to provide a review of all the different treatment procedures to be delivered to the cleft lip and palate patient from birth to adolescence.
Diagnosis and maternal counselling
Intrauterine diagnosis of orofacial clefts is possible by ultrasonography. Clefts are seen easily at 16 weeks of gestation, MRI is used increasingly for evaluation of fetal abnormalities that are difficult to identify on sonography alone.3, 4 Parental counselling may be required as the family will be under stress. Genetic counselling is also necessary5 .
Clinical findings:
These cases show absent or short columella, shallow gingivolabialsulcus, hypoplastic maxilla, dental problems like congenitally absent primary or permanent lateral incisors or missing premolars adjacent to alveolar cleft ,supernumerary teeth, enamel hypoplasia, microdontia/macrodontia, fused teeth aberrations in crown shape and Posterior cross bite with medial collapse of posterior segments.
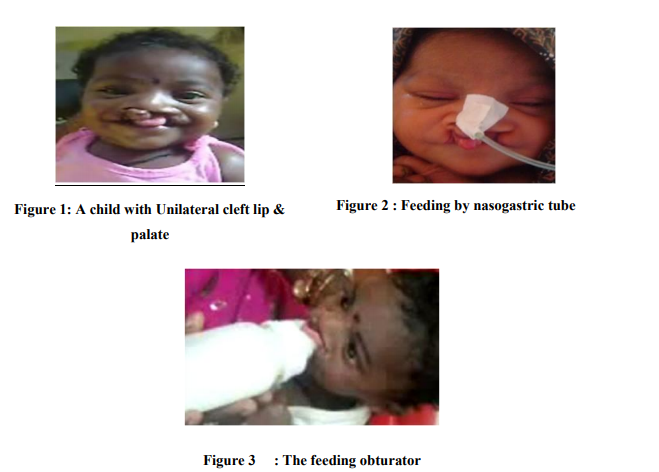
FIGURE 1 Management:
Mainly by multidisciplinary approach with timely and intricate coordination of various specialties Feeding Advice: Cleft children face a lot of problems in feeding like insufficiency in sucking milk from the nipple due to inability to create negative pressure, excessive air intake during feeding, choking, nasal discharge, regurgitation and excessive time required for nourishment make it difficult for the infant to maintain adequate nutrition .6, 7 Specialized feeding bottles such as the Hagerman feeder and Mead Johnson bottle helps in overcoming some of the feeding problems. The Mead-Johnson cleft palate feeder is a compressible bottle with an elongated cross-cut nipple. With this flow is increased by gently squeezing the bottle in rhythm with the infant‘s suckling action.. The mothers of cleft child are highly anxious during the feeding process, so counseling the right feeding skills is advisable, cleft babies kept upright at 450 while feeding make gravity aid in the feeding process.6 The feeding obturater is a prosthetic aid FIGURE 2,3 that is designed to obdurate the cleft and ensures the separation between the oral and nasal cavities, thereby reducing nasal regurgitation and helps in the development of the jaws and speech. It also prevents the tongue from entering the defect and interfering with spontaneous growth of the palatal shelves hence providing maxillary orthopaedic molding of the cleft segments into approximation before any surgical intervention is done.7, 8
Technique of fabrication of Obturators;
Impression technique: .is very challenging and There are variety of methods followed for it.
METHOD I
Some plastic surgeons prefer light-polymerizing acrylic resin sheets which are moldable to adapt to the oral anatomy after which it is taken out and cured with light to from the primary impression tray for preliminary impression. The impression is poured in Type III dental stone and a custom made tray is fabricated.. Final impression can be recorded with Vinyl polysiloxane materials; the baby is held face toward the floor, in order to prevent aspiration in the event of vomiting and asphyxia.
Method II
Primary impression can be made by softened green stick compound and For Wash impression putty consistency addition silicone impression material is used.6,3,5Most often used in patients with microstomia and palatal fistula where the patient is unable to open the mouth
Method III
A wax sheet of approximate size and shape can be adapted intraorally using the thumb and Index finger. A stone model of the negative wax reproduction is then obtained and a custom acrylic tray with a handle is prepared to be used for final impression.7
The Pre Maxillary Orthopaedics:
Orthopaedics start within the first week of life and aim at normalizing function and arch form by the most gentle means as possible during the first 18 months, a period of most intensive growth8 .
Naso Alveolar Molding [NAM] NAM
is a non surgical method of reshaping alveolus, lip and nostrils before cleft lip and palate surgery, lessening the severity of cleft.. The modern school of pre surgical orthopaedic treatment in cleft lip and palate was started by McNeil in 1950. Burston, an orthodontist, further developed McNeil's technique and made it.
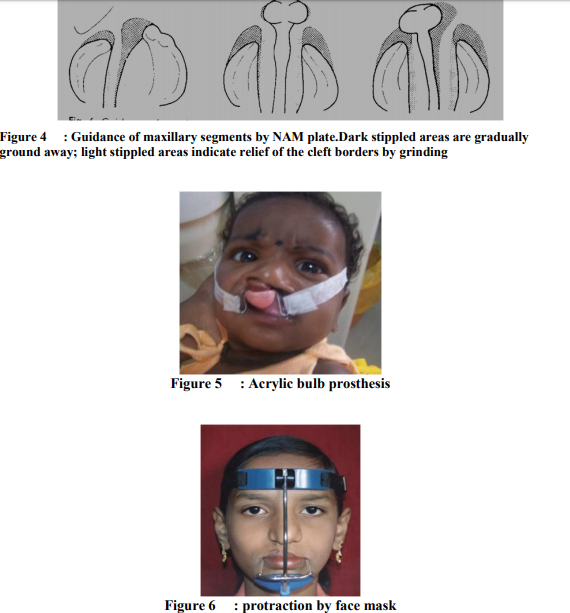
popular. It takes advantage of malleability of immature cartilage which is high in maternal estrogen and hyaluronic acid in the first few weeks of birth and its ability to maintain permanent correction of its form.NAM improves alignment of the alveolar segments and the cleft gap is significantly reduced in size before surgery, making primary repair of the lip, alveolus and the nose an effortless procedure. Narrowing of cleft region reduces tension of the tissues after surgery which would otherwise lead to lip dehiscence in large cleft lip surgery (McNeil 1956). it also improves aesthetic outcome (Gnoinski1990). It also forces the tongue out of cleft and aids in the development of normal tongue tip behaviour and enhances production of alveolar sounds at 1 yr of age (Dutchcleft trial; Konst et al 1999). Less scar tissue and better lip and nasal form can be achieved so reduces the number of surgical revisions for excessive scar tissue, oronasal fistulas, and nasal and labial deformities. With the alveolar segments in a better position and increased bony bridges across the cleft, the permanent teeth have a better chance of eruption in a good position with adequate periodontal support.8, 9, 10 It facilitates feeding, parental support and improved speech the aim of this procedure is Molding the nasal and alveolar segments before surgery to achieve optimum functional and esthetic results.(Oliver1973, Lubit1976, Huddart1990)8, 9, 11
Fabrication
The molding plate is fabricated on the dental stone model with clear self cure acrylic after blocking undercuts and the cleft space with wax. A small opening measuring 6-8 mm in diameter is made on the palatal surface to provide an airway in the event that the palate drops down posteriorly, especially in cases of Pierre Robin syndrome. A retention button is fabricated and positioned anteriorly at an angle of 400 to the plate. In the unilateral cleft only one retention arm is advised.9, 11
Appliance insertion and taping
The appliance is secured extra orally to the cheeks and bilaterally by surgical tapes that have orthodontic elastic bands at one end.. The tapes are a quarter inch in width and about 3-4 inches in length. The elastic on the surgical tape is looped on the retention arm of the molding plate and the tape is secured to the cheeks. The elastics (inner diameter 0.25 inch) are stretched approximately two times their resting diameter for proper activation force of about 100 grams. Parents are instructed to keep the plate in the child‘s mouth full time and to remove only for cleaning daily the use of skin barrier tapes on the cheeks like DuoDerm or Tegaderm is advocated to reduce irritation on the cheeks. The infant may require time to adjust to feeding with the appliance in the first few days. 11, 12, 13
Appliance Adjustments
The baby is seen weekly to make adjustments of the molding plate to bring the alveolar segments together by selectively removing the hard acrylic and adding the soft denture base relining material to the molding plate. No more than 1 mm of modification of the molding plate should be made at one visit9 .Guidance of maxillary segments moulding plate is adjusted by removing about 1mm soft acrylic along the medial surface of distorted major segment. FIGURE 4` After the cleft of the alveolus is reduced to about 5-6 mm the nasal stent is added to improve the alignment of base of the nose and the lip segment. Stent is made up of 0.36 inch, round stainless steel wire in the shape of a 'Swan Neck'. The stent is attached to the labial flange of the molding plate, near the base of the retention arm extends 3-4 mm past the nostril aperture.. The hard acrylic component is shaped into a bi-lobed form that resembles a kidney. 9, 11
Pre maxillary Retraction
In cases of cleft lip and palate, premaxillary segment may be positioned severely anterior to the maxillary arch or deviated laterally to one side of the cleft defect, a straight extra oral force would not place the pre maxilla in the facial midline In this case, an impression is made of the infant's premaxilla for construction of external acrylic "bulb" prosthesis. This appliance is fitted over the protruding and laterally displaced premaxilla and anchored to the infant's head with a bonnet appliance. After the premaxilla is in the midline, the bulb appliance is replaced by a single elastic strap. In many cases the use of soft, elastic tape (Microfoam Tape) can be used to retract the premaxillary segment in a simpler manner than with the bonnet retraction system.12, 17.It is worn 24 hours a day and is removed only for feeding. The desired movement can usually be accomplished within 6 to 8 weeks. FIGURE 5 Latham Appliance (described by Georgiade in 1970).It is an intra oral appliance anchored on the non-cleft maxillary segment that would exert forward force on the cleft maxilla and provide some control over the non-cleft segment. The appliance is designed so that it could be secured to the palatal segments with stainless steel pins. Clockwise turns of the screw move the cleft side of the appliance towards the screw head.18
Controversies of Infant Orthopaedics
Controversies exist against infant orthopedics. Some authors believe that this treatment is expensive and may inhibit maxillary growth (Pruzansky 1964). Bokhout et al (1996) showed that infant orthopedics increases the incidence of dental caries and cause irritation to the oral mucosa, gingival tissue or nasal mucosa.
Complications of NAM
Complications include intraoral tissue ulceration from excessive pressure applied by the appliance, commonly found in the oral vestibule and on the labial side of the premaxilla. The intranasal lining of the nasal tip can become inflamed if too much force is applied by the upper lobe of the nasal stent. Extreme care should be taken while removing the cheek tape to avoid any irritation to the skin.9, 13, 15
GINGIVOPERIOSTEOPLASTY:
This creates a mucoperiosteal bridge across the alveolar cleft associated with cleft lip and palate. The subperiosteal tunnel allows for bone generation in the absence of bone grafting in young patients. . Multiple studies reveal superior facial growth parameters, particularly vertical maxillary growth, when compared with primary bone grafting typically performed within the first year of life and a reduced need for later secondary bone grafting21 .
CHEILOPLASTY:
The appearance of an unrepaired wide cleft lip can be distressing lip surgery will significantly improve the infants appearance and thereby relieve parental apprehensions. Surgical closure of the cleft lip may be shortly accomplished after birth. i.e. at 10 weeks of age
PALATOPLASTY:
The repair of palate between 1- 1 1/2 years of age gives the best balanced result. Early repair leads to better speech development but severe midfacial growth retardation and dental malocclusion. If palatal repair is done after full growth of the maxilla, midfacial growth retardation and dental malocclusion problems will be less, but speech problem will be very severe. The soft palate is repaired early to facilitatespeech; surgical correction of hard palatal repair is deferred for a later repair at 4 to 5 years.
Hearing problems and Speech disorders
Paediatric dentist should also be aware of common speech and hearing problem for proper referral and timings of treatment. Speech disorders commonly found in cleft lip and palate patients are hypo nasality, ENT problems, nasal deviation, oronasal fistula and, abnormal growth of oronasal structures. Hyper nasal speech is corrected by pharyngoplasty and speech therapy.22Middle ear disease are commonly seen in cleft lip and palate patients mainly due to short Eustachian tube leading to failure of ventilatory function and abnormal insertion of Tensor veli palatine muscle into tube. These dysfunctions cause otitis media with effusion commonly known as glue ear. Early palatine surgery improves eustachian tube functions and any hearing problem should be repaired before the child learns to speak. A rehabilitative procedure employing palatal lift prosthesis (PLP) is given to recover diminished speech function22 .
Oral hygiene and Preventive therapy
Oral hygiene is of crucial importance after surgery, the patient is anxious about the bleeding caused due to surgery and is nervous to brush.20 Lip is lifted with the aid of index finger along the labial gingiva without damaging the scar and a baby brush with a small sized head is advised for brushing as there is a lack of sulcus depth and awkward tooth positions in the cleft region. 0.12% chlorhexidine gluconate mouthwash is useful for short periods following surgery to stabilize gingival health in severe cases of gingival inflammation; use of pit and fissure sealants is advisable.20 Patient-applied topical fluoride in the form of a mouthrinse is worthwhile especially during orthodontic treatment.
Orthodontic problems in mixed dentition
The midfacial deformities due to primary cleft surgeries include transverse maxillary deficiency with crossbite, midfacial retrusion, reduced anteroposterior development, mandibular prognathism and concave soft tissue profile. A current treatment protocol involves the combined use of Orthodontic treatment, alveolar bone grafting and Implant rehabilitation.17
Palatal expansion
The constricted maxilla as result of the scar tissue following surgery and restricted growth of mandible leads to cross bite. Various expansion appliances that are used are fan shaped maxillary expander, butter fly expander, rapid maxillary expander, quad helix expansion appliance, the banded hyrax appliance, and bonded rapid palatal expander.16, 18, 23 They are inefficient because of intermittent nature of force application. Also, they are often soldered to maxillary first molars with pre- existing mesiolingual rotations that the devices are unable to correct. These rotations can distort the appliances and until the rotations are corrected, much of potential expansion time is wasted25,27. To overcome disadvantages of rapid maxillary expansion,Nickel Titanium Expander were put forward by Micheal O. Abdoney in 1995. It is temperature activated expander which creates transverse expansion, uprights and rotates the maxillary molars and allows a smooth transition to fixed retention with not much dependence on patient compliance.27, 30 Bonded rapid palatal expander,an acrylic splint (0.2mm/day) for one month has shown approximately 4.2mm expansion. Protraction of mid face Protraction is achieved by using a face mask orthopedically. A force of 450 grams per side is initiated and is continued for 1.2 years for a minimum of 12-14 hrs/day. Though the skeletal changes are limited, they produce marked improvements in the soft tissue profile.33 Figure 6 Alveolar bone grafting Alveolar bone grafting is typically done between 9 and 11 years of age, when the permanent lateral incisor or the canine tooth roots are approximately one-third developed. It provides bony support to adjacent teeth and provide bony matrix for eruption of teeth in the cleft site. It also eliminates oronasal fistulae, elevate the alar base and provide adequate bone for future dental implant.26
Endosseous implant placement
It is done in case of congenitally missing lateral incisor. Factors influencing implant success are, type of bone used for the graft, developmental stage of the dentition and healing time of the graft. Implant is placed 4-6 months after the grafting procedure. It is not usually placed in young patients for the risk of it becoming ankylosed.31
Distraction Osteogenesis
Distraction of maxilla was first proposed by Molina & Oritz-Monasterio(1998). It is a procedure wherein two segments of bone are slowly moved apart in such a way that new bone fills the gap. A device known as distractor is attached to both sides of osteotomed bone, which is gradually adjusted over a period of days or week to stretch the bones so new tissue fills within it which enhances soft tissue adaptation..28, 29, 30
Alveolar distraction process using dental implants
An intraosseous, prosthetic device can be used to correct vertical bony defects and serve as the anchor for prosthesis after completion of distraction It is a two-stage procedure in which the implant is placed and permitted to heal for some month .After a latency period of 5 to 12 days, active distraction is started. After completion of distraction process the implant is used to support a dental prosthesis.31, 32
Complications
Mechanical problems, such as pin loosening, device failure, Local infections, Ankylosis of zygoma and coronoid process, Damage to teeth and Tooth mobility.
Orthognathic surgeries for secondary cleft and craniofacial deformities
Timing of surgery depends on functional problems, psychological factors and facial growth pattern.35 generally it is done after completion of growth or when skeleton is mature to achieve predictable results. Lefort I maxillary osteotomy is the basic procedure for the corrections of maxillary deficiency in patients who have cleft .Mid face osteotomies at Lefort II and Lefort III level also have been used depending on the esthetic needs of patients.34,37
PSYCHOLOGICAL FACTORS:
Patients with cleft palate have lowered self esteem and difficulties in social interaction. Parents of children with clefts are more likely to spoil their child by being over protective. Communication disorders are more the result of psychological problems than phonological which influences the entire development of an affected child. Strong parent support networks may help to prevent the development of negative self concept in children with cleft lip and palate.
SUMMARY
There has been a robust growth in the treatment of cleft lip and palate and has come a long way before the total rehabilitation by multi disciplinary approach has helped the cleft patient lead a normal life with almost a face as normal as any other individual and is been possible with excellent surgical results and intricate and seamless multidisciplinary approach by various specialists. The paediatric dentist has a pivotal role restoring esthetics and function and providing continuing high quality, preventive- based dental care through thorough treatment planning and skilful behaviour management.
References:
1. Batra P,Duggal R Prakash H. Genetics of cleft lip and palate revisited. J Clin Pediatr Dent: 27(40): 311-320; 2003
2. Cobourne M T. The Complex genetics of Cleft lip and palate. European Journal of Orthodontics 26:7-16; 2004
3. Jianyan L et al. Analysis of interactions between genetic variants of BMP4 and environmental factors with nonsyndromic cleft lip with or without cleft. Int J Oral Maxillofac Surg:39: 50-56: 2010 4. Bender PL. Genetics of cleft lip and palate. J Pediat Nurs:15; 242-49 2000
5. Jones MC, Prenatal diagnosis of cleft lip and palate: Detection rates, accuracy of ultrasonography and strategies for councelling .Cleft Palate Craniofac J; 39; 169-73,2002
6. Bhatia R,Trivedi BD. Role of Pediatric Dentist in Cleft Lip and Cleft palate patients. Scientific Journal: 3:2009
7. Pani S C, Hegde A M .Impressions in cleft lip and palate -A novel two stage technique. J Clin Pediatr Dent: 33(2):7-10, 2008 8. Ijaz A, Nasoalveolar moulding of the unilateral cleft of the lip and palate infants with modified stent plate; Pakistan Oral and Dental Journal: 28: 1, 2010
9. Grayson B H, Cutting CB. Presurgical Nasoalveolar Orthopedic Molding in Primary Correction of the Nose, Lip and Alveolus of Infants born with Unilateral and Bilateral clefts. Cleft palate Craniofac. J; 37:528-532, 2000
10. Pfeifer T M, et al Nasoalveolar moulding and gingivoperiosteoplasty versus alveolar bone graft: An outcome analysis of costs in the treatment of unilateral cleft alveolus: Cleft Palate craniofacial journal :39:1,2002
11. Mitsuyoshi L et al Simple modified preoperative nasoalveolar moulding in infants with unilateral cleft lip and palate: British journal of Oral and maxillofacial surgery: 42; 578-580,2004
12. Yang S, Stelnicki EJ, Lee MN. Use of Nasoalveolar molding appliance to direct growth in new born patient with complete unilateral cleft and palate. Pediatr Dent :25; 253-256 , 200
13. Aminpour S, Tollefson TT.Recent advances in Presurgical molding in cleft lip and palate.Plast reconstr surg ;122(4):1131-7 , 2008
14. King NM et al. The management of children born with cleft lip and palate. HKMJ; 2; 153- 159, 1996
15. Grayson BH, Shetye PR. Presurgical Nasoalveolar moulding treatment in cleft lip and palate patients.; Review; Indian J Plast Surg; 42(S); 56-61,2009
16. Jaeger, M Braga-Silva. Correction of the Alveolar Gap and Nostril Deformity by Presurgical Passive Orthodontia in the Unilateral Cleft Lip; J Ann Plast Surg; 59: 489–494, 2007
17. Vargervik K. Growth characteristics of the premaxilla and orthodontic treatment principles in bilateral cleft lip and palate. Cleft palate journal:20(4):289-301,1983
18. Spira M, Findlay S, Hardy S, Gerow F ; Early maxillary orthopedics in cleft palate patients: A Clinical Report, Journal of CranioMaxillofacial Surgery:24, 45–48, 1992
19. Yukihiro F et al Journal of maxillofacial prosthestics:22(2):86-94,1999
20. Rivkin CJ. Dental care for the patients with a cleft lip and palate. BDJ: 188:2, 2000
21. Losquadro WD, Tatum SA .Direct gingivoperiosteoplasty with palatoplasty.Facial plast surg 2007 may;23(2): 140-5
22. Witzel MA. Speech evaluation and treatment. Oral Maxillofac Surg Clin North Am 3: 501- 16, 1991
23. Vasant MR.Menon S, Kannan S.Maxillary Expansion in Cleft lip and Palate using Quad Helix and Rapid Palatal Expansion Screw. MJAFI: 65 :150-153:2009
24. Klempner S Early orthopaedic class III treatment with a modified tandem appliance: JCO:37(4):218-223,2003
25. Isaacson R J .Some effects of Rapid maxillary expansion in cleft lip and palate patients: AJOD: 34;3,1964
26. Kawakami et al .Maxillary Expansion and protraction in cleft lip/palate. Angle orthodontist 2002:72(4):356-361
27. Rygh P .Orthopedic Expansion and Protraction of maxilla in cleft palate patients – A New Treatment rationale Cleft palate journal:19; 2, 1982
28. Watzinger F et al. Computer-aided surgery in distraction osteogenesis of maxilla and mandible .Int J Oral Maxillofac Surg; 28; 171- 175, 1999
29. Swennen G et al .Craniofacial distraction osteogenesis:review of literature.Part –I clinical studies.Int J Oral Maxillofac surgery:30:89-103,2001
30. Arndt.WV .Nickel Titanium Palatal Expander .JCO; Mar129-137, 1993
31. Salyer KE, Xu H et al .Skeletal facial balance and hormony in the cleft patient :principles and techniques in orthgnathic surgery.Indian journal of plastic surgery;42;149-167,2009
32. Pena WA et al. The Role of Endosseous Implants in the Management of Alveolar Clefts Pediatr Dent; 31; 329-333; 2009
33. Sakamoto T et al. Orthodontic treatment for jaw deformities in cleft lip and palate patients with the combined use of external expansion arch and a facial mask.Bull.Tokyodent coll: 43(4):223-229,2002
34. Oral and maxillofacial Surg Clin N Am:17: 503-517,2005
35. Smith AS et al :Prenatal Diagnosis of Cleft Lip and Cleft Palate Using MRI .American journal of roentgenology:183: 229-235,2004
36. Ravichandra et al: A new technique of impression making for an obturator in cleft lip and palate cases.J Indian Soc Pedod Prev Dent: 4( 28); 311-314,2010
37. Chigurupathi R : Orthognathic surgeries done for secondary cleft and craniofacial deformities. Oral Maxillofacial Surg Clin N Am: 17;503-517 ,2005
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License