IJCRR - 8(21), November, 2016
Pages: 19-24
Print Article
Download XML Download PDF
CLINICAL STUDY OF CONTEMPORARY PATTERN AND OUTCOME OF HYPERTENSION IN PREGNANCY AMONG PRIMIPAROUS AND MULTIPAROUS WOMEN IN A TERTIARY CARE CENTRE
Author: Renukadevi B., Kavitha G., Rathna Ramamurthy, Raja rajeshwari
Category: Healthcare
Abstract:Introduction: Hypertension complicates 10% of all pregnancies. Various adverse outcomes of hypertension in pregnancy include antepartum hemorrhage, postpartum hemorrhage, acute renal and hepatic failure, maternal death, preterm birth, intrauterine growth retardation, and neonatal death. Despite various screening tools, there is high prevalence of hypertension in pregnancy and its related complications. Periodical analysis such cases are of utmost importance as it may help in early identification of the problem and measures to prevent its complications.
Objectives: The objectives of this study is to identify the difference in pattern of hypertension in primiparous and multiparous women and its maternal and fetal outcomes and differences in lab parametersin both groups.
Methodology: This was a retrospective study conducted among 88 women with hypertension and /or proteinuria complicating pregnancy who were admitted for delivery in the department of obstetrics and gynaecology, Velammal Medical College over a period of 1 year (Aug 2015 \? July 2016). The data were collected from the patients' records. The patients were divided into two groups, primiparous and multiparous. The data were collected in terms of age, parity, gestational age, mode of delivery, birth weight of baby and complications. The results were statistically analysed with IBM SPSS statistics software 23.0 version.
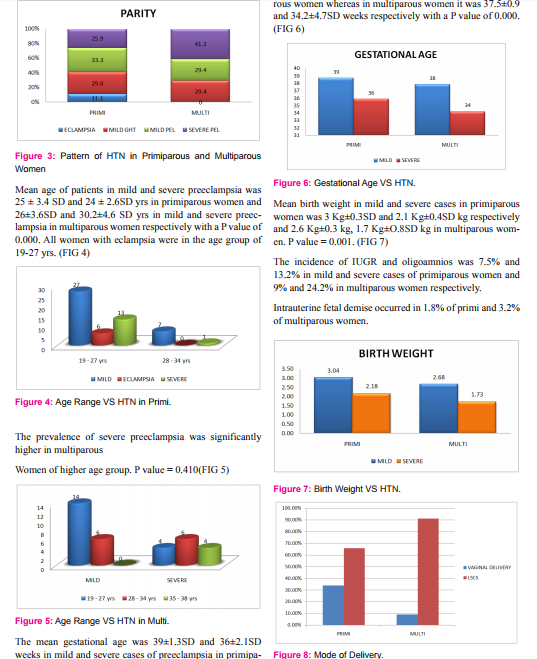
Results: The frequency of hypertensive disorders of pregnancy was 11.6 % in our study. The prevalance of eclampsia was 0.7%. The mean gestational age of babies was 39 weeks and 36 weeks in mild and severe preeclampsia in primiparous women and 37.5 and 34.2 weeks in multiparous women. The mean platelet count in mild and severe cases were 2.5 and 1.8 lakhs/cu mm in primiparous and 2.4 and 1.9 lakhs/cu mm in multiparous women.
Conclusion: Though the prevalence of hypertension in primiparous women is more, the prevalence of severe preeclampsia in more common in multiparous women. Almost all cases of eclampsia occurred in primiparous women. A different pathophysiology could be a cause of hypertension in pregnancy in primiparous and multiparous women, as implied by significant differences in both groups.
Keywords: Eclampsia, Gestational hypertension, Hypertension, IUGR, Preeclampsia
Full Text:
INTRODUCTION
Hypertensive disorders in pregnancy is one of the most commonly encountered medical problem which causes significant maternal and fetal morbidity and mortality. The classification of hypertension disorders in pregnancy as recommended by the National high blood pressure education program working group includes 1) Gestational hypertension 2) Preeclampsia –Eclampsia 3) chronic hypertension 4) preeclampsia superimposed on chronic hypertension.Gestational hypertension is defined as blood pressure of >140/90 on two separate occasions atleast 6 hrs apart without proteinuria after 20 weeks of gestation. Mild Preeclampsia is defined as BP of 140/90 mmHg or more on two separate occasions atleast 4 hours apart with urinary protein excretion of > 300mg/ 24 hrs . Because of its wide spectrum of prevalence, edema is no longer included in the diagnostic criteria. Severe preeclampsia is defined as BP ≥ 160/110 mmHg and significant proteinuria of ≥3 + or > 5gm/day with evidence of other organ dysfunction.
MATERIALS AND METHODS
This was a retrospective study done among 88 women with hypertension and /or proteinuria admitted for delivery in the department of obstetrics and gynaecology in velammal medical college. This study was conducted over a period of 12 months from august 2015 – July 2016.
METHODS OF COLLECTION OF DATA
The data of the patients were obtained from patients’case records.Demographic details of the patient ,obstetric history, gestational age, blood pressure recordings, mode of delivery, fetal weight, lab investigations were collected and entered in excel sheet.They were divided into groups of primiparous and multiparous women and data analysed.
INCLUSION CRITERIA
All pregnant women admitted for delivery with hypertension with or without proteinuria in pregnancy were included in the study.
EXCLUSION CRITERIA
All pregnant women with secondary hypertension were excluded from the study.
DATA ANALYSIS
The collected data were analysed with IBM.SPSS statistics software 23.0 Version.To describe about the data descriptive statistics frequency analysis, percentage analysis were used for categorical variables and the mean and S.D were used for continuous variables. To find the significant difference between the bivariate samples in Independent groups the Unpaired sample t-test was used. For the multivariate analysis the one way ANOVA with Tukey's Post-Hoc test was used.To find the significance in categorical data Chi-Square test was used. In all the above statistical tools the probability value .05 is considered as significant level.
RESULTS
The frequency of hypertensive disorders of pregnancy was 11.6 % in our study .There was a total of 757 deliveries during the study period. Eighty eight (88) women were diagnosed as hypertensives during pregnancy and thus the prevlance of hypertension in pregnancy was 11.6%. The prevalace of eclampsia was 0.7%(n=6) .Among 88 patients, mild GHT was 29%, mild Preeclampsia was 32%, severe preeclampsia was 32% and eclampsia was7%.(FIG 1)
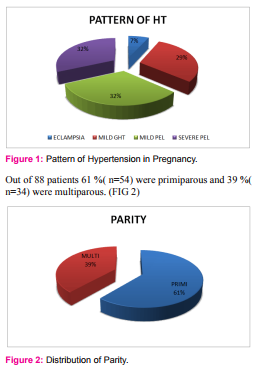
The prevalence of mild preeclampsia was 27.6% in primiparous and 29.4% in multiparous women whereas the prevalence of severe preeclampsia was 25.9% and 41.2% in both groups with significant increase in multiparous women. P value (0.410). In our study eclampsia was present in 11.1% of primiparous women whereas none of multiparous women had eclampsia. (FIG 3)
Mean uric acid level in mild and severe preeclampsia in primiparous women was 4.74 mg% and 6.23 mg% respectively and 4.6 mg% and 5.2 mg% in mild and severe preeclampsia in multiparous (p value 0.001) (FIG 9).
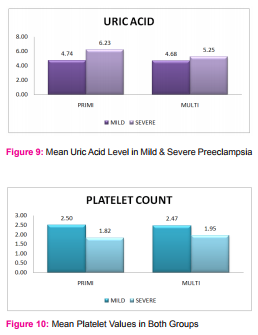
The mean platelet count in mild and severe cases were 2.5 and 1.8 lakhs/cu mm in primiparous and 2.4 and 1.9 lakhs/cu mm in multiparous women. P value 0.001. (FIG 10) Among 88 patients, 2 (2.2%) had abruption, 2(2.2%) developed HELLP, 1 (1.1%) pt had PPH and 1(1.1%) patient had massive ascites. The prevalence of eclampsia was 0.7% in our study. Mean age of patients was 24.1±2.5SD yrs. Mean gestational age was 38±1.7SD weeks and Mean birth weight 2.6 ±0.8kg.
DISCUSSION
The frequency of hypertensive disorders of pregnancy was 11.6 % in our study.It is a leading cause of maternal and fetal morbidity and mortality in both developed and developing countries and contributes significantly to economy of health care.3,4The incidence of preeclampsia in India is reported to be 7-10% of the pregnancies.2We also observed preeclampsia in 6.7% of our study population.It is the second largest cause of maternal mortality in India and is responsible for 14% of maternal deaths.Racial differences, socioeconomic status and other parameters like parity and age attribute to the variations in incidence .1 The prevalence of Eclampsia in our study was found to be 0.7 % of pregnancies. The reported incidence of eclampsia from India is 0.71 % which is comparable with our study.
Age and Parity has an important influence on the incidence of hypertensive disorders of pregnancy. A study done in Saudi Arabia showed that women at extremes of maternal age, the nulliparous women, and high-parity women are at an increased risk of developing pre-eclampsia. Young primigravidae under 20 years and all patients over 30 years have an increased chance of hypertension.5 In our study highest incidence of the hypertensive disorders occurred among those aged 19 to 27 years. This could be because the majority of conceptions take place in this age group in our country. The age distribution of eclampsia patients in our study is similar to other reports and suggests that eclampsia is, probably, a disease of young women6.Eclampsia exclusively occurred in primigravida in our study.
The incidence of PIH increases with advancing gestation and early-onset PIH is often associated with severe preeclampsia.7This correlates with our study in which the mean gestational age was 34 weeks in cases of severe preeclampsia and 38 weeks in mild cases.
In our study the incidence of caesarean section was 77.5%. (FIG 7) According to Miguil M et al 8 and Dissanayake VH et al9, caesarean section rates hypertension complicating pregnancy was 71% and 78% respectively.
Complications of fetus parallels the severity of disease in preeclampsia .With increasing severity of hypertension and proteinuria, there is an increased incidence of IUGR and preterm labour.According to Eskenazi et al, increased incidence of SGA fetus occurred in multiparous women with severe preeclampsia.10This correlates with our study which shows that incidence of IUGR in multiparous women was 24.2 % compared to13.2 % in primiparous with severe preeclampsia.Another study by Gleicher et al showed that with different parity in hypertension there was no difference in fetal birth weight.11
According to Al-Mulhim A.A et al, placental abruption was the leading maternal complication (12.6%) in women with preeclampsia, followed by oliguria (7.9%), coagulopathy (6.0%), and renal failure (4.1%).7 In our study, abruption occurred in 3.4%, 2.2% had HELLP syndrome and 1.1% had severe ascites complicating preeclampsia.
Thrombocytopenia is the most common hematological abnormality seen to occur in 11% to 29% of patients with preeclampsia.12,13.They are also associated with qualitative changes suggesting increased platelet production and destruction.
S. Joshi et al (2004) reported platelet count of 2.2 lakh/cumm in control group, 2.0 lakh/cumm in mild preeclampsia, 1.40 lakh/cumm in severe preeclampsia and 1.30 lakh/cumm in eclampsia. In our study the values correlate well with 2.48lakhs/cu mm in mild cases and 1.88lakhs/cu mm in severe cases.
Increase in uric acid is associated with 8–9 fold risk for preeclampsia and a 1.6–1.7-fold risk for SGA infants. An ROC analysis suggests that a uric acid of 5.2 mg/dl provides excellent sensitivity, specificity and likelihood ratios for diagnosis and prognosis. Hence measurement of serum uric acid is clinically useful and should be a part of evaluation of the pregnant patient with preeclampsia. An elevated serum uric acid in pregnancy may is a valuable biomarker for preeclampsia and also has a contributory role in the pathogenesis of the maternal and fetal manifestations as suggested by evidence.14,15It is a potent inhibitor of endothelial function, induces systemic and glomerular hypertension in animals, and passes freely into the fetal circulation and has a direct role in blocking fetal angiogenesis resulting in SGA infants.16This correlates with our study in which patients with severe preeclampsia had a mean uric acid level of 6.2 and 5.2 mg/dl in primiparous and multiparous women.
Currently there are no well established measures for prevention of preeclampsiaand there is no single reliable test for screening.17Moderate reduction in blood pressure has been observed with calcium supplementation in women at high risk for hypertension in pregnancy. In women with abnormal uterine artery doppler in second trimester ultrasound, low dose aspirin has been shown to reduce the incidence of preeclampsia.
Patients with risk factors and rapid increase in weight gain and facial edema are closely monitored for onset of hypertension and proteinuria.For patients with established diagnosis of preeclampsia a series of lab tests should be conducted and repeated frequently if required.Fetal growth is tested with a baseline sonogram at 25-28 weeks.Biweekly non stress test and biophysical profile is indicated in the presence of IUGR and oligoamnios and delivery is contemplated in the presence of fetal compromise. Regional anaesthesia with minimal risks is preferred during caesarean delivery and contraindicated in the presence of coagulopathy.
The management goals during labour includes control of hypertension and prevention of seizures. Antihypertensive agents that are used in severe preeclampsia includes labetalol and hydralazine. Magnesium sulphate is the drug of choice to prevent seizures though it does not prevent the progression of disorder.19
CONCLUSION
According to our study though preeclampsia is more in primiparous women , severity was increased in multiparous women which could be attributed to varying pathophysiology in both groups.In our study eclampsia solely occured in primiparous women.Though preeclampsia is not preventable, maternal deaths due to this condition can be avoided. Quality antenatal care, early detection of the condition ,close monitoring with maternal and fetal surveillance and effective management will be crucial in reducing morbidity and mortality associated with this condition.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Ethics committee approval: Obtained
Source of funding: None
Conflicts of interest: None
References:
1. Al-Ghamdi Saeed MG, Al-Harbi AS, Khalil A, El-yahya AR. Hypertensive disorders of pregnancy: prevalence, classification and adverse outcomes in northwestern Saudi Arabia. Annals of Saudi Medicine Journal 1999; 19:557-560.
2. MoodleyJ.South Africa Med.j.CME-1991;9:72.
3. World Health Organization. Global Program to Conquer Preeclampsia/Eclampsia.2002.
4. Dolcea C. AbouZahr C. Global burden of hypertensive disorders of pregnancy in year 2002. In: Global Burden of Diseases;2000; World Health Organisation..
5. Zibaeenazhad MJ, M Ghodsi P Arab, Gholzom N. the prevalence of hypertensive disorders of pregnancy in Shiraz, Southern Iran; Iranian Cardiovascular Research Journal 2010; 4:169-172
6. J.Nadkarni, J. Bahl, P. Parekh. Perinatal outcome in pregnancy associated hypertension, Indian pediatrics 2001,38:174-178
7. Al-Mulhim AA, Abu-Heija A, AlJamma F, El-Harith el-HA. Preeclampsia: maternal risk factors and perinatal outcome. Fetal Diagn Ther. 2003; 18 (4): 275-80.
8. Miguil M, Chekairi A. Eclampsia, Study of 342 cases. Hypertension in Pregnancy. 2008; 27 (2): 103-11.
9. Dissanayake VH, Samarasinghe HD, Morgan L, Jayasekara RW, Seneviratne HR, Pipkin FB. Morbidity and mortality associated with preeclampsia at two tertiary care hospitals in Sri Lanka. J Obstet Gynaecol Res. 2007; 33 (1): 56-62.
10. Eskenazi B, Fenster L, Sidney S, Elkin EP. Fetal growth retardation in infants of multiparous and nulliparous women with preeclampsia. Am J Obstet Gynecol 1993; 169: II 12-8.
11. Gleicher N, Boler LR, Norusis M, Del Granado A Hypertensive diseases of pregnancy and parity. Am J Obstet Gynecol 1986; 154: I 044-9.
12. Gibson G, Hunter D, Neame PB, Kelton JG. Thrombocytopenia in pre-eclampsia and eclampsia. Semin Thromb Hemost. 1982;8:234-247.
13. Pritchard JA, Cunningham FG, Mason RA. Coagulation changes in eclampsia: their frequency and pathogenesis. Am J Obstet Gynecol. 1976;8:855-864.
14. Kang DH, Finch J, Nakagawa T, Karumanchi SA, Kanellsi J, Granger J, Johnson RJ. Uric acid, endothelial dysfunction and pre-eclampsia: searching for a pathogenetic link. Journal of hypertension. 2004; 22:229–235. [PubMed: 15076175]
15. Bainbridge SA, Roberts JM. Uric Acid as a Pathogenic Factor in Preeclampsia. Placenta. 2008 29S: 67–72.
16. Feig DI, Nakagawa T, Karumanchi SA, Oliver WJ, Kang DH, Finch J, Johnson RJ. Hypothesis: Uric acid, nephron number, and the pathogenesis of essential hypertension. Kidney international. 2004; 66:281–287. [PubMed: 15200435]
17. ACOG Committee on Obstetric Practice. ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. No. 33, January 2002.
18.American College of Obstetricians and Gynecologists. Obstet Gynecol 2002;99:159-67Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol 2000;183:S1-22.
19. Livingston JC, Livingston LW, Ramsey R, Mabie BC, Sibai BM. Magnesium sulfate in women with mild preeclampsia: a randomized controlled trial. Obstet Gynecol 2003;101:217-20.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License