IJCRR - 4(20), October, 2012
Pages: 85-88
Date of Publication: 20-Oct-2012
Print Article
Download XML Download PDF
ACTINOMYCOSIS OF BREAST-A CASE REPORT
Author: B. Arora, Sumit Giri , D.R. Arora
Category: Healthcare
Abstract:Primary actinomycosis of the breast is a very rare disease and most commonly caused by Actinomyces israelii which normally inhabits mouth, colon, and vagina. Primary forms directly affect the breast but the etiology is unknown. Possible causes include infection of the lactiferous ducts due to trauma during breast feeding or kissing. In secondary actinomycosis, the infection at the primary sight ultimately reaches the breast. The purpose of the study is to present, in detail, a case of a 50 year old woman, with the complaint of swelling in the right breast of 6 months duration which was variable in size and associated with discharging sinuses.
Keywords: Actinomycosis, breast, Actinomyces israelii.
Full Text:
INTRODUCTION
Actinomycosis is a chronic granulomatous or suppurative disease, usually caused by an anaerobic bacterium called Actinomyces israelii, which is a common organism found in the nose and throat, flora of oral cavity, particularly in the periphery of decayed teeth, and in the grooves of tonsils, as well as female genital tract [1, 2]. It is a Gram-positive, non-motile, non-sporing, nonacid- fast organism[3]. Disease is characterized by development of abscesses, draining by multiple sinus tracts containing bloody suppurative discharges and “sulphur granules” which are composed of branched filaments. The disease is classified clinically to the varieties of cervicofacial, thoracic, abdominal and pelvic. Clinical signs of disease are different, depending on the site of infection. The infection is not contagious. Actinomycosis is seen in all age groups and regions globally, but occurs frequently between 15 to 35 years, and its reported frequency in men is two times that in women [4]. Primary actinomycosis of the breast was first described by Ammentrop in 1893. Breast actinomycosis is primary when inoculation occurs through the nipple. Secondary actinomycosis of the breast refers to the extension of a pulmonary infection through the thoracic cage in a process that can affect the ribs, muscles and finally the breast [5]. Breast actinomycosis may present as sinus tract or with mass-like features mimicking malignancy. The clinical presentation makes it difficult to distinguish primary actinomycosis from mastitis and inflammatory carcinoma [6]. We report a case of primary actinomycosis of the breast caused by Actinomyces israelii that was diagnosed by fine needle aspiration cytology (FNAC) and was further confirmed on histopathologic study of a specimen obtained by excisional biopsy, Gram stain and culture.
CASE REPORT
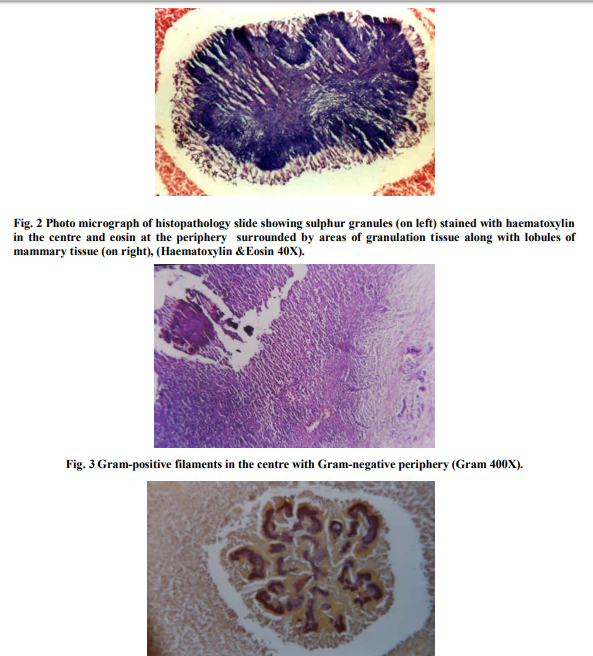
A 50-year-old woman, otherwise healthy, presented in surgery outpatient department of our hospital with the complaint of swelling in the right breast of 6 months duration which often increased and decreased in size and was associated with episodes of on and off burst to discharge pus. No history of lung disease, breast trauma, gingivitis, or tooth problems was found and it was diagnosed as chronic breast abscess and she was referred to pathology department for FNAC. Physical examination revealed a firm fluctuating swelling in upper outer quadrant of right breast measuring 6x4 cm in size, with marked induration in the surrounding area. The overlying skin was adherent to the swelling but the underlying structures were free. On pressing the swelling, pus-like discharge came out. No palpable adenopathy was found. Examination of oral cavity, face and neck for detecting any skin lesion or mass was unremarkable. All other test results including blood biochemistry, hemoglobin electrophoresis, urine analysis and stool examination were within normal limits except for mild leukocytosis in the blood count. FNAC smears were prepared from pus-like discharge which oozed out on pressing the swelling and stained with May Grunwald Giemsa stain. Microscopy revelaed grains which comprised of hyphal fragments surrounded by a peripheral zone of swollen radiating club-shaped structures presenting as sun-ray appearance in a background dense inflammatory infiltrate (Fig.1). Histopathology confirmed the diagnosis. Gross examination revealed multiple grey white to grey yellow tissue pieces. The largest piece was skin covered measuring 6x3x3cms. Cut surface was grey brown in some areas and dark tan in others. A grain of dark colour was also seen in the dark tan area. Haematoxylin & eosin stained sections revealed lobules of breast tissue along with “sulphur granules” which were deeply stained with haematoxylin except in the periphery which was stained by eosin, which showed short, radiate, club-like structures. It was surrounded by areas of granulation tissue comprising of predominantly polymorphonuclear leukocytes, lymphocytes, plasma cells and fibroblasts (Fig.2). Pus was shaken with sterile water in a tube and “sulphur granules” were allowed to settle at the bottom. Half of these were removed with a Pasteur pipette and were crushed between two slides and stained with Gram stain. Microscopy revealed Gram-positive filaments with Gram-negative periphery (Fig.3). Remaining were crushed in a drop of saline with a glass rod and inoculated on brain heart infusion agar, blood agar and thioglycollate broth and incubated both anaerobically and aerobically with 5−10% carbon dioxide at 350 −370 C for upto 14 days. The colonies of Actinomyces israelii were 0.5−2 mm in diameter, white to grey-white, smooth, lobulated resembling molar teeth.
DISCUSSION
Breast actinomycosis is rare throughout the world and only a few cases have been published so far [5,7−11]. It has been called „the most misdiagnosed disease?, and it has been stated that „no disease is so often missed by experienced clinicians? [12]. Primary actinomycosis of the breast is an unusual condition where the most commonly isolated pathogen has been A. israelii [13]. Possible causes of this condition include trauma, lactation and kissing [14]. Most of the reported cases of primary actinomycosis of the breast were caused by A. israelii. In recent years, other strains have been found as well. For instance Brunner et al. [11] reported a catalase-negative strain of Actinomyces neuii as the possible causative agent of an infected mammary prosthesis. Mohammed in 1993 described a case of actinomycosis of the accessory breast [9].
CONCLUSION
The physician should keep actinomycosis in mind as a possible diagnosis and perform the appropriate investigation, if the pathogenic findings of a mass are in favour of granulomatous inflammatory process or microabscess formation, and if work up for tuberculosis, and or fungal infections are negative. Actinomycosis should be vigorously sought and promptly treated in patients with chronic granulomatous disease presenting with uncommon and prolonged clinical signs of infection.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Baron EJ, Finegold SM. 80'ed. Mosby, St. Louis, Baltimore 1990; P: 521-23.
2. Brook I. Actinomycosis. In: Goldman L, Ausiello D, eds.Cecil Medicine. 24th ed. Philadelphia, Pa: Saunders Elsevier; 2011:P 337.
3. Arora DR, Arora B. Actinomycetes in Textbook of Microbiology, CBS Publishers and Distributors, New Delhi. Bangalore 3rd edition 2008, pp 481-86.
4. Zaini F, Mchbod ASA, Emami M. Comprehensive medical mycology. Tehran University Publication. Tehran Iran 1999; P: 39-40.
5. de Barros N, Issa FK, Barros AC, D?Avila MS, Nisida AC, Chammas MC, Pinoti JA, Cerri GG: Imaging of primary actinomycosis of the breast. AJR Am J Roentgenol 2000; 174:1784–86.
6. Capobianco G, Dessole S, Becchere MP, Profili S, Cosmi E, Cherchi PL, Meloni GB: A rare case of primary actinomycosis of the breast caused by Actinomyces viscosus: Diagnosis by fine-needle aspiration cytology under ultrasound guidance. Breast J 2005; 11:57–59.
7. Gogas J, Sechas M, Diamantis S, Sbokos C. Actinomycosis of the breast. Int Surg 1972; 57 (8):664-65.
8. Schouten A. A case of primary actinomycosis of the breast. Arch Chir Neerl 1973; 25(3): 319-23.
9. Mohammed KN. Actinomycosis of the accessory breast treated with cotrimoxazole. Med J Malaysia 1993; 48(2): 229-31.
10. Jain BK, Sehgal VN, Jagdish S, Ratnakar C, Smile SR. Primary actinomycosis of the breast: a clinical review and a case report. Dermatol 1994; 21(7): 497-500.
11. Brunner S, GrafS Riegel P, Altwegg M. Catalase negative Actinomyces neuii subsp. Neuii isolated from an infected mammary prosthesis. Int J Med Microbiol 2000; 290(3): 285-87.
12. Mandell GL, Bennett JE, Dolin R: Principles and Practice of Infectious Diseases, ed 6. Saunders, 2005, pp 2924–31.
13. Attar KH, Waghorn D, Lyons M, Cunnick G: Rare species of actinomyces as causative pathogen in breast abscess. Breast J 2007;13:501–05.
14. Lloyd-Davies JA: Primary actinomycosis of the breast. Br J Surg 1951;38:378–81.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License