IJCRR - 4(23), December, 2012
Pages: 124-130
Date of Publication: 15-Dec-2012
Print Article
Download XML Download PDF
RANDOMIZED CLINICAL TRIAL OF SINGLE VERSUS THREE DOSES OF CEFAZOLIN AS PROPHYLAXIS FOR NONPERFORATED ACUTE APPENDICITIS
Author: Sheik Abdullah, Rajan Vaithianathan, Kannan Rajendiran, Ramachandran Santhanam
Category: Healthcare
Abstract:Background: The most common and significant cause for morbidity following emergency appendicectomy is surgical wound infection. There are conflicting reports regarding the optimal duration of antibiotic prophylaxis in nonperforated appendicitis. The efficacy of prolonged prophylactic antibiotic treatment in preventing wound infection for nonperforated appendicitis is poorly defined. Objective: A prospective randomized study was carried out to compare the efficacy of single dose cefazolin with three doses of cefazolin in reducing the incidence of postoperative wound infection for patients with nonperforated acute appendicitis. Methods: One hundred patients with a clinical diagnosis of appendicitis were randomized into two groups. Group 1 received single intravenous dose of 1gm cefazolin at induction of anaesthesia and group 2 received two further doses of cefazolin following surgery. Postoperative wound infection was the primary endpoint. Results: The two groups were similar with regard to demographic data, pathologic condition of the appendix and duration of hospital stay. The postoperative wound infection rate was not significantly different among the two groups, 11% in group 1 and 9% group 2 (p =0.986). Conclusions: Single-dose cefazolin is equally effective to multiple-dose cefazolin in preventing postoperative wound infection in patients undergoing open appendicectomy for nonperforated acute appendicitis. However, because of the greater convenience and economic implications, single pre-operative dose of cefazolin is the choice of prophylaxis for nonperforated appendicitis.
Keywords: acute appendicitis, antibiotic, single dose, nonperforated
Full Text:
INTRODUCTION
Appendicectomy is one of the most common emergency surgical procedures with a postoperative wound infection rate of 1-10%1-4 . Wound infection following open appendicectomy is a major cause for post-operative morbidity, prolonged hospitalization and increased costs. The pathologic state of the appendix is the most important determinant of postoperative wound infection following appendicectomy5, 6. The incidence of wound infection in patients with complicated appendicitis (perforated or gangrenous appendix) is nearly four to five times greater than that of nonperforated cases. The efficacy of antibiotic prophylaxis in reducing wound infection in patients undergoing open appendicectomy is well established. Many randomized and observational studies have shown that appropriate use of antibiotics reduces the risk of infection by 40–60%4, 7-10 . Based on prospective clinical studies, guidelines have been established regarding the choice of prophylactic antibiotics, it’s timing and route of administration for emergency appendicetomy11. However, the duration of antibiotic usage remains a contentious issue and there is no definite consensus among the surgical community12, 13 . Single dose antibiotic prophylaxis has been recommended for majority of elective general surgical procedures14. In reality, this practice is not universally accepted and multiple dose regimens are still in use at many centres. In the emergency setting, though postoperative antibiotics are universally used for perforated appendicitis, no consensus exists regarding the efficacy of postoperative antibiotics in preventing surgical site infections in nonperforated cases. The main purpose of our study was to compare the efficacy of single dose of cefazolin with multiple doses of cefazolin in reducing the rate of wound infection in nonperforated appendicitis.
RESEARCH METHODOLOGY
A randomized prospective study of 100 patients with a clinical diagnosis of acute appendicitis presenting to the Emergency Department of Mahatma Gandhi Medical College was carried out over a period of two years. Before performing an emergency open appendicectomy, the patients were randomized into two groups by opening a sealed envelope containing details of the prophylactic antibiotic regimen to be used. Group 1 received single dose of cefazolin 1gm i.v. at time of induction of anaesthesia. In group 2, two further doses of cefazolin were given intravenously at 8 hours and 16 hours from the time of index surgery. Appendicectomy was carried out in all the patients by the standard protocol of open surgical technique. The surgical wound was closed in layers.
Exclusion criteria:
1.Gangrenous or perforated appendix
2. Abscess found at time of surgery
3. Allergic to cephalosporins
4. Prior antibiotic treatment
During the post-operative period, the progress of the surgical wound was monitored on a daily basis for all the patients included in the study. Wound infection was graded using the Southampton scoring system15.
Wound healing was taken as normal for grades 0, 1 and 2. Infection of the wound was categorised as minimal for grade 3 and as major for grades 4 and 5. Patients who developed major infection were treated appropriately with daily wound irrigation and antibiotics based on culture reports. Informed consent was obtained from all the patients and the study was carried out with prior clearance from the ethical committee.
Study parameters:
- Demographic data –age and sex
- Final histopathological report of the appendix
- Grade of wound infection
- Length of hospital stay
Statistical Method - Comparison of proportions by ‘CHI Square’ test.
RESULTS
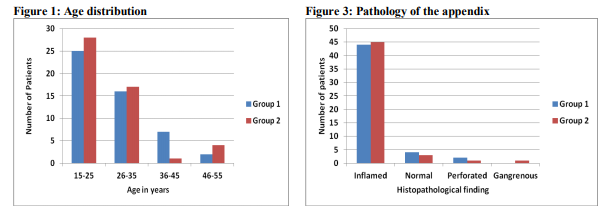
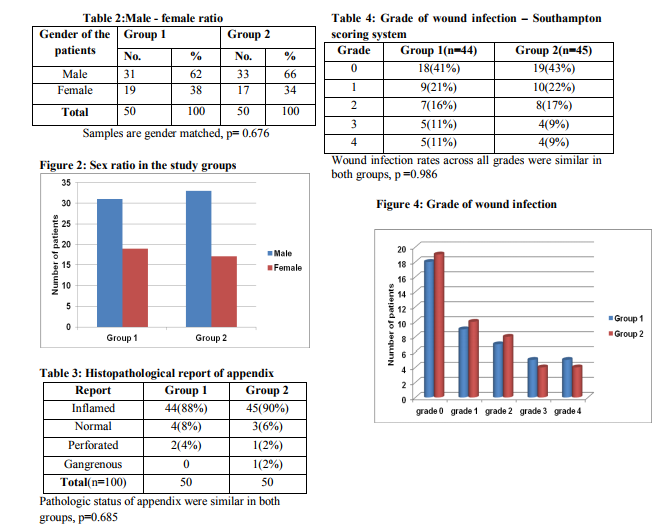
In our study, 100 patients were included with a diagnosis of acute appendicitis and randomized to two groups, with fifty patients in each group. The age group varied from 15 to 55 years in both groups, with a mean age of 28.2 years in group 1 and 29.1 years in group 2 (p=0.147) , as shown in table 1 and fig 1. The male to female ratio was 1.63 and 1.94 in group 1 and group 2 respectively (p=0.676) as shown in table 2 and fig 2. The histopathological examination of the removed appendix revealed features of acute inflammation in 44(88%) patients in group 1 and 45(90%) in group 2. Six patients in group 1 and 5 from group 2 were excluded from the study in view of the presence of perforation, gangrenous or normal appendix (table 3 and fig 3). In the postoperative period, the surgical wounds were examined and graded using the Southampton scoring system. Normal wound healing was observed in 34(77%) patients in group 1 and 37(82%) in the other group. Minimal wound infection which resolved spontaneously was present in 5 out of 44 patients (11%) in group 1 and 4 of 45 (9%) patients belonging to group 2. Discharge of pus (grade 4) was observed in 5(11%) patients in group 1 and 4(9%) in group 2. No patients in either group developed grade 5 wound infection. Using Chi square test for analysis, the incidence pattern and the grade of wound infections in both the study groups were found statistically not significant(p=0.986), table 4 and fig 4. The mean hospital stays of the single-dose and three-dose groups were 4.6 days and 5.2 days. The median duration of stay was 5 days in both groups. There was no significant difference in length of hospital stay between the two groups.
DISCUSSION
Usage of appropriate antibiotics is well known to control wound infection rates following open appendicectomy for uncomplicated acute appendicitis. While antibiotic prophylaxis is common in surgical procedures16, inappropriate use of antibiotics occurs in 25–50% of general elective surgeries17-21. A Cochrane systematic review found that antibiotic use in patients having uncomplicated appendicitis was superior to placebo in reducing the rates of postoperative complications but concluded that no recommendations can be made regarding the duration of antibiotic use. At the same time, in patients with severe form of appendicitis, it has advised to continue a comprehensive antibiotic regime, as the risk of infective complications is quite high in this group1 . The choice of antibiotic for prophylaxis varies widely in different centres and even among the different surgical units attached to the same Institute. The American Society of Health System Pharmacists (ASHP) recommends cephalosporins as drug of choice for prophylaxis for nonperforated appendicitis and gentamicin with metronidazole only in cases of penicillin allergy22, 23. The major controversy lies in the optimum duration of prophylaxis in cases of acute nonperforated appendicitis. Many studies have shown that single preoperative dose of antibiotic is as effective as multiple postoperative doses in preventing wound complications following appendicectomy24-26 . A randomized control study by Mui et al have shown that single dose of preoperative antibiotic is adequate for prevention of infective complications of the wound in patients undergoing surgery for uncomplicated appendicitis. Their conclusion was that the prolonged antibiotic administration was cost-ineffective and led to unnecessary complications27 . In our study, we have used a more objective method to assess the progress of the surgical wounds by correlating with the Southampton scoring system. There was no significant difference (p=0.986) between wound infection rates of the single-dose group (11%) and the threedose group (9%). These findings are in full agreement to the similar studies in the literature24- 27 . Moreover, comparing the incidence of wound infection across all the grades in both the groups by using the Chi-square test has shown no significant difference between the two groups(p=0.986). Cefazolin was chosen in our study as it was readily available, cheaper and has very good antibacterial spectrum for pathogens causing post appendicectomy sepsis. This choice of antibiotic is in line with the recommendations given by the ASHP22. We also found from our study that there was no significant difference in the length of the hospital stay between the two groups. The median duration of stay in both groups was 5 days. Many studies have highlighted and repeatedly emphasised the effects of improper choice and inappropriately prolonged duration of prophylactic antibiotics on the rising emergence of antimicrobial resistance among the common pathogens28-33. Coakley et al, in a recent study, have consistently proven that postoperative antibiotic treatment for nonperforated appendicitis did not reduce infectious complications. In fact, their study showed significantly increased rate of adverse effects like Clostridium difficile infection, diarrhea, longer length of hospital stay and higher treatment cost. Patients receiving postoperative antibiotics were also more frequently readmitted and reoperated34 . A possible benefit that can be derived from our study is that by using a single preoperative dose, the surgeon can be certain of having given an effective prophylaxis at induction of anaesthesia without the need to monitor further postoperative doses. Moreover, avoiding further intravenous doses of antibiotics may lead to savings in terms of nursing effort, time and the cost of treatment.
CONCLUSION
It is evident that prophylactic postoperative doses of cefazolin confer no additional benefit over a single preoperative dose of cefazolin. With additional benefits of the greater ease of administration and decreased cost, single-dose cefazolin is the prophylaxis of choice for appendicectomy in patients with nonperforated appendicitis. It is essential for surgeons and surgical departments to update their routine practice of antibiotic prophylaxis to comply with updated guidelines and evidence base.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are citied and included in references of this manuscript. The authors are also grateful to authors/ editors/publishers of all those articles, journals and books from where the literature for this article has been review and discussed. The authors also thank all the residents and staff in the Department of Surgery, Dean and Vice Chancellor of Mahatma Gandhi Medical College and Research Institute for their support throughout the study period, without which this study would not have been possible.
References:
1. Andersen BR, Kallehave FL, Andersen HK. Antibiotics versus placebo for prevention of postoperative infection after appendicectomy. Cochrane Database Syst Rev 2005; 3:CD001439.
2. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control 2004; 32:470-85.
3. Hale DA, Molloy M, Pearl RH, Schutt DC, Jaques DP. Appendectomy: a contemporary appraisal. Ann Surg 1997; 225:252-61.
4. Koch A, Zippel R, Marusch F, Schmidt U, Gastinger I, Lippert H: Prospective multicenter study of antibiotic prophylaxis in operative treatment of appendicitis. Dig Surg 2000; 17:370-78.
5. Bennion RS, Thompson JE, Baron EJ et al. Gangrenous and perforated appendicitis with peritonitis: treatment and bacteriology. Clin Ther 1990; 12 Suppl C:31-44.
6. Browder W, Smith JW et al. Nonperforative appendicitis: a continuing surgical dilemma. J Infect Dis 1989; 159:1088-94.
7. Lau WY, Fan ST, Chu KW, Suen HC, Yiu TF, Wong KK. Randomized, prospective, and double-blind trial of new betalactams in the treatment of appendicitis. Antimicrob Agents Chemother 1985; 28:639-42.
8. Nguyen BL, Raynor S, Thompson JS. Selective versus routine antibiotic use in acute appendicitis. Am Surg 1992; 58:280-83.
9. Tonz M, Schmid P, Kaiser G. Antibiotic prophylaxis for appendectomy in children: critical appraisal. World J Surg 2000; 24:995- 98.
10. al Dhohayan A, al Sebayl M, Shibl A, al Eshalwy S, Kattan K, al Saleh M. Comparative study of augmentin versus metronidazole/gentamicin in the prevention of infections after appendicectomy. Eur Surg Res 1993; 25:60-64.
11. Antimicrobial prophylaxis in surgery. Med Lett Drugs Ther 1999; 41:75-80.
12. Danziger L, Hassan E. Antimicrobial prophylaxis of gastrointestinal surgical procedures and treatment of intra-abdominal infections. Drug Iniell Clin Pharm 1987; 21:406-16.
13. Fry DE. Antibiotics in surgery. An overview. Amj Surg 1988; 155(5A):11-5.
14. Malcolm Mcdonald, Elizabeth Grabsch, Caroline Marshall, Andrew Forbes. SingleVersus Multiple–Dose Antimicrobial Prophylaxis For Major Surgery. A Systematic Review. ANZ J Surg 1998; 68:388–95. 15.
15.Bailey SI, Karran SE, Toyn K et al. Community surveillance of complications after hernia surgery. Brit Med J 1992; 304:469-71.
16. Dellinger EP, Gross PA, Barrett TL, Krause PJ, Martone WJ,McGowan JE Jr, Sweet RL, Wenzel RP. Quality standard for antimicrobial prophylaxis in surgical procedures. Infectious Diseases Society of America. Clin Infect Dis 1994; 18:422-27.
17. Gyssens IC, Geerligs IE, Nannini-Bergman MG, Knape JT, Hekster YA,van der Meer JW. Optimizing the timing of antimicrobial prophylaxis in surgery: an intervention study. J Antimicrob Chemother 1996; 38:301-8.
18. Silver A, Eichorn A, Kral J, Pickett G, Barie P, Pryor V, Dearie MB. Timeliness and use of antibiotic prophylaxis in selected inpatient surgical procedures. The Antibiotic Prophylaxis Study Group. Am J Surg 1996; 171:548-52.
19. Bedouch P, Labarere J, Chirpaz E, Allenet B, Lepape A, Fourny M, Pavese P, Girardet P, Merloz P, Saragaglia D, Calop J, Francois P. Compliance with guidelines on antibiotic prophylaxis in total hip replacement surgery: results of a retrospective study of 416 patients in a teaching hospital. Infect Control Hosp Epidemiol 2004; 25:302-7.
20. Pons-Busom M, Aguas-Compaired M, Delas J, Eguileor-Partearroyo B. Compliance with local guidelines for antibiotic prophylaxis in surgery. Infect Control Hosp Epidemiol 2004; 25:308-12.
21. Dahms RA, Johnson EM, Statz CL, Lee JT, Dunn DL, Beilman GJ. Third-generation cephalosporins and vancomycin as risk factors for postoperative vancomycinresistant enterococcus infection. Arch Surg 1998; 133:1343-46.
22. ASHP Therapeutic Guidelines on Antimicrobial Prophylaxis in Surgery. American Society of Health-System Pharmacists. Am J Health Syst Pharm 1999; 56:1839-88.
23. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 1999; 27:97- 132.
24. Liberman MA, Greason KL, Frame S, Ragland JJ. Single dose cefotetan or cefoxitin versus multiple dose cefoxitin as prophylaxis in patients undergoing appendectomy for acute nonperforated appendicitis. J Am Coll Surg 1995;180:77-80
25. Le D, Rusin W, Hill B, Langell J. Postoperative antibiotic use in nonperforated appendicitis. Am J Surg 2009; 198:748-52.
26. Tsang TM, Tam PK, Saing H.Antibiotic prophylaxis in acute nonperforated appendicitis in children: single dose of metronidazole and gentamicin. J R Coll Surg Edinb 1992; 37:110-2.
27. L.M. Mui, E.K.W. Ng,D.W.H. Lee, Y.H. Lam et al. A Prospective Randomized Trial To Compare One Dose Preoperative, ThreeDose Perioperative And 5-Day Full Course Antibiotics For Nonperforated Acute Appendicitis. Ann College Surg Hong Kong 2000; 5:19–20.
28. Paterson DL, Rossi F, Baquero F, Hsueh PR, Woods GL, SatishchandranV, Snyder TA, Harvey CM, Teppler H, Dinubile MJ, Chow JW. In vitro susceptibilities of aerobic and facultative Gram-negative bacilli isolated from patients with intra-abdominal infections worldwide: the 2003 Study for Monitoring Antimicrobial Resistance Trends (SMART). J Antimicrob Chemother 2005; 55:965-73.
29. Kusum M, Wongwanich S, Dhiraputra C, Pongpech P, Naenna P. Occurrence of extended-spectrum beta-lactamase in clinical isolates of Klebsiella pneumoniae in a University Hospital, Thailand. J Med Assoc Thai 2004; 87:1029-33.
30. Girlich D, Naas T, Leelaporn A, Poirel L, Fennewald M, Nordmann P. Nosocomial spread of the integron-located veb-1-like cassette encoding an extended-spectrum betalactamase in Pseudomonas aeruginosa in Thailand. Clin Infect Dis 2002; 34:603-11.
31. Girlich D, Poirel L, Leelaporn A, Karim A, Tribuddharat C, Fennewald M, Nordmann P. Molecular epidemiology of the integronlocated VEB-1 extended-spectrum beta-lactamase in nosocomial enterobacterial isolates in Bangkok, Thailand. J Clin Microbiol 2001; 39:175-182.
32. Biedenbach DJ, Johnson DM, Jones RN. In vitro evaluation of cefepime and other broadspectrum beta-lactams in eight medical centers in Thailand. The Thailand Antimicrobial Resistance Study Group. Diagn Microbiol Infect Dis 1999; 35:325-31.
33. Teng LJ, Hsueh PR, Tsai JC, Liaw SJ, Ho SW, Luh KT. High incidence of cefoxitin and clindamycin resistance among anaerobes in Taiwan. Antimicrob Agents Chemother 2002; 46:2908-13.
34. Coakley BA, Sussman ES, Wolfson TS, Bhagavath AS, Choi JJ, Ranasinghe NE, Lynn ET, Divino CM. Postoperative antibiotics correlate with worse outcomes after appendectomy for nonperforated appendicitis. J Am Coll Surg 2011; 213:778- 83.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License