IJCRR - 5(5), March, 2013
Pages: 144-149
Date of Publication: 22-Mar-2013
Print Article
Download XML Download PDF
COMPARISON OF SUPERVISED EXERCISE WITH AND WITHOUT MANUAL PHYSICAL THERAPY FOR PATIENTS WITH SHOULDER IMPINGEMENT SYNDROME
Author: Sunita R. Yemul
Category: Healthcare
Abstract:Study Design: A prospective randomized clinical trial. Background: Manual physical therapy combined with exercise is a commonly applied but currently unproven clinical treatment for impingement syndrome of the shoulder. Objective: To compare the effectiveness of manual physical therapy with and without supervised exercise program in shoulder impingement syndrome. Methods: Random assignment of sixty patients (29 male, 31 female) diagnosed with shoulder impingement syndrome was done to 1 of 2 treatment groups. The exercise group performed supervised flexibility and strengthening exercises. The manual therapy group performed the same program and received manual physical therapy treatment. Both groups received the selected intervention 12 times over 1- month. Outcome measures were pain, pain-free abduction range, strength of shoulder abductors, internal and external rotators and functional activities. Pre and posttreatment measures were taken. Results: The study result shows statistically significant pain reduction, increase in pain-free shoulder abduction and improvement in strength of shoulder abductors, external and internal rotators within the groups. The shoulder function score showed statistically significant improvement in manual therapy group while supervised exercise group although showed improvement but could not be proved statistically. Results of all the outcome measures in manual therapy group were statistically significant when compared to supervised exercise group. Conclusion: Manual therapy with supervised exercise program is more effective than supervised exercise program alone for reducing pain, enhancing pain-free abduction ROM, improving function and strength in patients with shoulder impingement syndrome.
Keywords: Shoulder impingement, manual therapy, supervised exercises
Full Text:
INTRODUCTION
Shoulder disorders are among the most common of all peripheral joint complaints. The cumulative incidence of shoulder problems in general medical practice was estimated to be 11.2/1000 patients per year.1 Kamkar et al. cited two common etiologies of shoulder pain as shoulder instability and impingement syndrome.2 The concept of subacromial impingement syndrome (SAIS) was introduced by Neer I.3 SAIS is one of the most common shoulder disorders in adults, with a high socioeconomic impact on working ability.4 SAIS represents mechanical compression of the rotator cuff, subacromial bursa, and biceps tendon against the anterior undersurface of the acromion and coracoacromial ligament, especially during elevation of the arm.3 Therapeutic exercise regimes are advocated torestore shoulder mobility and stability, by improving ROM and enhancing glenohumeral as well as scapulothoracic muscle function.5 Manual therapy techniques are commonly used by Physical Therapist to relieve pain and increase the mobility of joints.6 Faber E and colleagues in his systematic review reported that exercise combined with manual therapy is more effective than exercise alone and found many studies using range of motion and pain as outcome measures but functional limitations were less often used as an outcome measure in SAIS.7 However, there are less evidences comparing the effectiveness of manual physical therapy with supervised exercises and supervised exercises alone in patients of shoulder impingement syndrome. So, present study intended to compare the effectiveness of manual physical therapy with and without supervised exercise program in shoulder impingement syndrome.
MATERIAL AND METHODS
The present study is a Randomized Controlled Trial conducted in subacromial impingement syndrome patients between the age group of 18- 65 years in a physiotherapy set up. The SAIS patients coming to physiotherapy department referred from orthopedic OPD constituted the population of the study. A total number of 80 patients were screened using the following proforma out of which 60 (29 male and 31 female) met the inclusion criteria and accepted to participate were included in the study. To be included in the study patients were required to fulfill the following criteria: (1) pain during one of the two tests in category I (2) pain during one test from either category II or category III Category I: Impingement signs- Patient in standing position. 1. Passive overpressure at full shoulder flexion with the scapula stabilized. 2. Passive internal rotation at 90-degree shoulder flexion in the scapular plane and in progressive degrees of horizontal adduction. Category II: Active shoulder abduction-Patient standing against a wall. Category III: Resisted break tests for the following movements1. Abduction 2. Internal rotation 3. External rotation Subjects were excluded if they had any history of rotator cuff tear or adhesive capsulitis, shoulder dislocation, subluxation, or fracture, cervical radiculopathy and subject received Physical therapy or chiropractic treatment for the shoulder, neck or upper back in the last 6 month.
PROCEDURE
The approval of the institute’s ethics committee was taken prior to the commencement of the study. The purpose and methodology of the study was explained to the patients in a language they understood. A written consent in a language they understood was taken and patient had right to withdraw anytime from the study. The patients were randomly assigned into 2 treatment groups by the alternate method. Each group consisted of equal number of patients (30) Group A - Supervised exercise program. Group B - Supervised exercise program with manual therapy as an intervention. The treatment for supervised exercise group consisted of a standardized flexibility and strengthening program that was performed in the physiotherapy set up under the direct one-to-one supervision of a physical therapist. The flexibility program consisted of 2 stretching exercises, one for the anterior shoulder musculature and the other for the posterior shoulder capsule and surrounding musculature. Each stretch was held for 30 seconds and performed 3 times with a 10- second rest period between each stretch. There are 6 strengthening exercises, all of which are the essential ‘core exercises’ of shoulder rehabilitation program. Four of the strengthening exercises required the use of Theraband. They are made from latex, of Thera-Band Company. Each band was 3 inches (7.6 centimeters) wide and 5 feet (156 cm) long. These exercises included shoulder flexion, scaption, rowing, and horizontal extension-external rotation. For each of the Theraband exercises, a 10-repetition maximum was determined. The selection of colour of theraband was based on the therapist observation of shoulder movement quality and the patients’ responses for fatigue and pain. Deterioration in movement quality or pain exceeding a mild discomfort was avoided during all strengthening exercises by either reducing the level of resistance or modifying the ROM until the subject could progress. The level of theraband resistance was adjusted so for all subjects throughout the treatment process. Each band exercise was performed as 3 sets of 10 repetitions with a 60-second rest period between each set. The remaining 2 exercises, the seated press-up and the elbow push-up plus required a stable chair and a firm surface to lie on. Both exercises are performed to fatigue or for a maximum of 25 repetitions. The quality of all repetitions of each exercise was continuously monitored. Besides the supervised exercise program, the manual therapy group received manual therapy techniques applied to the specifically assessed pain and movement limitations at the glenohumeral joint. Patients received 12 manual therapy sessions, 3 sessions per week. Manual therapy program includes Maitland’s mobilization techniques comprising of passive physiological and accessory movements, muscle stretching, and soft tissue mobilization.8,9 Passive accessory or passive physiological Maitland mobilization grades I-IV were given accordingly. The oscillatory pressure of two to three oscillations per second was given. Each indicated technique was administered two to four times (30 seconds each). For situations where pain or muscle spasm preceded a sensation of resistance, grade I or II is applied and when pain receded, the end-feel became more resistant and less painful, grade III and IV pressure was applied. Postero-anterior, locking position and caudal glide for shoulder were given. Modification or progression of treatment on subsequent visits was contingent on findings in the reassessment process. Techniques also included soft tissue massage and muscle stretching particularly to the pectoralis minor, infraspinatus, teres minor, upper trapezius, sternocleidomastoid, and scalenes musculature. Cervical and thoracic postural exercises such as chin tucks were taught to patients in both the group. The treatment for both the groups was continued for 1 month. The patient’s were assessed for the following outcome measures at 1 st day pretreatment and 15th and 30th day posttreatment.
OUTCOME MEASURES
Overall pain intensity was measured by using Visual analogue scale. VAS is a reliable tool for measuring pain.10The functional assessment questionnaire (FAQ) was used to measure the functional activities of any shoulder disorders. Pain free abduction range (PFAR) of the patients was measured by the universal goniometer. MMT was used to measure the muscle strength of shoulder abductors, external and internal rotators. Kendall’s prescribed the 0-5 grading with plus and minus which is used in our study and other key symbols are given for statistical convenience.11
DATA ANALYSIS
The data collected is tabulated and analyzed using SPSS version 16 software. Demographics were done by using unpaired t test and chi square test. Between the two groups unpaired t test was used. A level of significance was set at p<0.05.
RESULTS
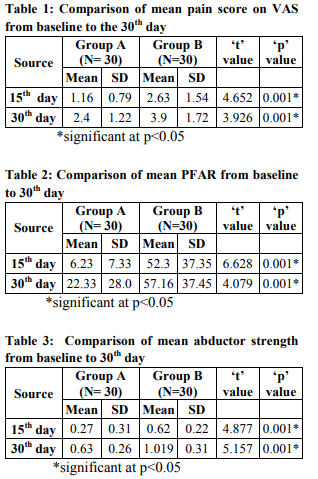
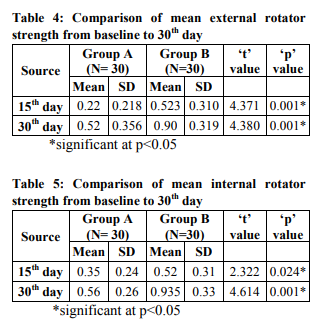
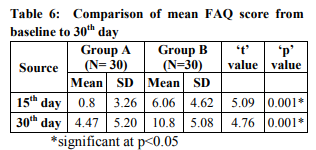
Age distribution was matching at baseline in both the groups when analyzed by unpaired t-test. The comparison of gender distribution of the subjects in both groups was statistically non significant using Pearson chi square test suggesting gender distribution is comparable in both the groups. Table 1 to 6 details the results of present study.
DISCUSSION
The study was conducted on 60 patients (29 male and 31 female) between the age group of 18 - 65 years. The study result shows statistically significant decrease in pain, increase in pain-free shoulder abduction and improvement in strength of shoulder abductors, external rotators and internal rotators within the groups. The shoulder function score showed statistically significant improvement in Group B while Group A although showed improvement but could not be proved statistically. Results of all the outcome measures in group B were statistically significant when compared to Group A. Bang and Deyle compared 52 subjects to 2 groups supervised exercise with manual therapy and supervised exercise only. The researchers measured pain, isometric force, and function. Although both groups showed improvement in pain, isometric force and function the subjects who received manual therapy showed greater gains than who did not receive manual therapy for all variables.5 Results of the present study are concurrent to this study. The standardized strengthening exercises designed were proved effective as ‘shoulder core’ exercises in an EMG analysis done by Hal Townsend12 and J. Bruce Moseley. 13 The two stretching exercises were included to stretch the capsule. Both groups received direct supervision of the strengthening and stretching program by the therapist. Devries has proposed that beginning strength has no physiologic meaning, but training status will determine the potential for strength gains. He suggests that untrained individuals gain strength at much greater rates than individuals with an established training program.14 The improvement in the strength observed in the supervised exercise group in the present study is in concurrence with the findings of the study mentioned here. According to Conroy and colleagues in their study the significant improvement in range of motion experienced by the experimental and control group was the result of improved strength and timing of the rotator cuff and deltoid muscle force coupling mechanism.15 The present study also found an improvement in the abduction ROM which might be due to improvement in strength and forcecoupling of muscle. Manual therapy group with supervised exercise program shows significant improvement than supervised exercise program alone. According to Wyke BD, joint mobilization is one method of enhancing the frequency of discharge from the mechanoreceptors, thereby diminishing the intensity of many types of pain.16 Conroy DE et al. in their study concluded the improvement in range of motion may be in part the product of many factors, such as neurophysiologic reduction in pain and associated muscle guarding, mechanical reduction in edema, improved rotator cuff and shoulder girdle strength.15 A vital component of the Maitland approach is that the treatment is based on constant assessment and reassessment, with subsequent individual modifications of treatment techniques.17 Subjects in the manual therapy group were frequently observed to have decreased pain and increased abduction ROM immediately following the application of manual therapy procedures. Conroy et al comments that functional limitations are assumed to be related to decreased mobility and pain associated with the condition. Improved mobility and pain would, therefore, be expected to lead to functional improvement.15 In the present study, group B improved in mobility and pain measure than group A resulting in greater improvement of shoulder function of the group B. In a study by G. Senbursa compared the conservative exercises with and without manual therapy in 40 SAIS patients. They concluded that both groups had significant improvement in pain but manual therapy group improved significantly in function and ROM while conservative group did not.18 This supports the present study as the improvement of function in group A was not statistically significant as compared to group B. Although both the groups showed statistically significant improvement on all the outcome measures, these improvements were more pronounced in Group B than Group A.
CONCLUSION
The result of the present study suggest that Manual therapy with supervised exercise program is more effective than supervised exercise program alone for reducing pain, enhancing painfree abduction ROM, improving function and strength in patients with shoulder impingement syndrome.
ACKNOWLEDGMENT
Authors acknowledge the great help received from the scholars whose articles cited and included in references of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. Authors are grateful to IJCRR editorial board members and IJCRR team of reviewers who have helped to bring quality to this manuscript.
References:
1. Vander Windt, D.A., Koes, B.W., Boeke, A.J., Devillé, W., De Jong, B.A. and Bouter, L.M. Shoulder disorders in general practice: Prognostic indicators of outcome. British Journal of General Practice.1996;46:519-523.
2. Kamkar A, Irrgang J, Whitney S. Nonoperative Management of Secondary Shoulder Impingement Syndrome. J Orthop Sports Phys Ther. 1993;17(5):212-24.
3. Neer CS II. Anterior acromioplasty for the chronic impingement syndrome in the shoulder. J Bone Joint Surg Am. 1972; 54:41–50.
4. Walther M, Werner A, Stahlschmidt T, Woelfel R, Gohlke F. The subacromial impingement syndrome of the shoulder treated by conventional physiotherapy, selftraining, and a shoulder brace: results of a prospective, randomized study. J Elbow Surg. 2004;13(4):417-23.
5. Bang MD, Deyle GD. Comparison of Supervised Exercise With and Without Physical Therapy for Patients With Shoulder Impingement Syndrome. J Orthop Sports Phys Ther. 2000;30(3):35-9.
6. Threlkeld AJ. The effects of manual therapy on connective tissue. Phys Ther. 1992;72:893-902
7. Faber E, Kuiper JI, Burdorf A, Miedema HS, Verhaar JA. Treatment of impingement syndrome: a systematic review of the effects on functional limitations and return to work. J Occup Rehabil. 2006;16(1):7-25
8. Maitland GD. Peripheral Manipulation. 3rd Boston, Mass: Butterworth Heinemann; 1991. pp. 1-128,221-89.
9. Maitland G, Hengeveld E, Banks K, English K. Maitland's Vertebral Manipulation. 6th ed. Boston, Mass: Butterworth-Heinemann; 2001.pp. 325–383.
10. Boonstra, Anne M, Preuper S, Henrica R, Reneman, Michiel F, et al. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. International Journal of Rehabilitation Research. 2008;31 (2) :165-9.
11. Kendall FP, McCreary EK, Provance PG. Muscles testing and function. 4th ed. Lippincott Williams and Wilkins;1997.
12. Hal Townsend. Electromyography analysis of the glenohumeral muscles during a baseball rehabilitation program. Am J Sports Med.1991;19(3):264-72.
13. J. Bruce Moseley. EMG analysis of the scapular muscles during a shoulder rehabilitation program. J Sports Med. 1992; 20 (2):128-34.
14. Devries HA. Physiology of Exercise. Dubuque: Wm C Brown Company; 1980: 393.
15. Conroy DE, Hayes KW. The effect of joint mobilization as a component of comprehensive treatment for primary shoulder impingement syndrome. JOSPT 1998;28(1):3 – 14.
16. Wyke BD: Neurological aspects of pain therapy: a review of some current concepts. In: Swerdlow M (ed), The Therapy of Pain, p 1. Lancaster, England: MTP Press Ltd, 1981
17. Henricus M Vermeulen, Piet M Rozing, Wim R Obermann, Saskia le Cessie and Thea PM Vliet Vlieland. Comparison of High-Grade and Low-Grade Mobilization Techniques in the Management of Adhesive Capsulitis of the Shoulder: Randomized Controlled Trial. Physical therapy. 2006;86(3):355-68.
18. Senbursa G, Baltac G, Ahmet. Comparison of conservative treatment with and without manual physical therapy for patients with shoulder impingement syndrome: a prospective, randomized clinical trial. Knee surgery sports traumatology Arthroscopic surgery. 2007;5(7):915- 21.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License