IJCRR - 5(5), March, 2013
Pages: 140-143
Date of Publication: 22-Mar-2013
Print Article
Download XML Download PDF
OSSIFICATION OF VERTEBRAL LIGAMENTS AND ITS JOINTS - A CASE REPORT
Author: Sujana M., Sharmada K.L., Sowmya S., Pushpaltha M.
Category: Healthcare
Abstract:Human Axial skeleton has drawn much interest for Medical Researchers because of the upright posture. The human vertebral column plays an important role in stability and weight transmission [1]. It is adapted to protect the spinal cord. Congenital or acquired anomalies are common in the vertebral column [1]. At the same time the vertebral column is the site for many orthopedic disorders which may be pathological or developmental, leading to instability, kyphosis, low back pain[1], scoliosis, Forestier's disease[4], Bechterew's disease[6], Ankylosing spondylitis[1] and myelopathy[3].
Keywords: vertebral column, osiffication, Anterior & Posterior longitudinal ligaments (ALL, PLL), Supraspinous ligament (SSL), Bechterew’s disease, Forestier’s disease.
Full Text:
INTRODUCTION
The vertebral canal houses the spinal cord. Abnormalities in any of features may be associated with neurological signs and symptoms which lead to compression of nerve roots and spinal cord [1]. The ligaments which hold the vertebrae are ALL, PLL, SSL and interspinous ligament (ISL). The adjacent vertebrae are held together by intervertebral disc [7]. The ALL is strong, broad fibrous band, covers and connects anterior aspects of bodies of vertebral and intervertebral disc, extends from anterior arch of atlas to pelvic surface of sacrum. The ALL helps to maintain stability and prevent hyperextension of vertebral column [7]. The PLL interconnects the vertebral bodies and intervertebral disc posteriorly with in the vertebral canal, which limits the flexion of vertebral column and resists the gravitational pull. The SSL is a strong fibrous cord, which connects apices of spinous processes from C7 to sacrum. The ISL is thin and membranous, interconnects the spinous processes from root to the apex of adjacent processes. These ligaments stabiles and limits flexion of spine. At the points of attachment to the tips fibrocartilage is developed in the ligaments leading to ossification or calcification of the ligaments. It may be due to trauma or genetic or any other factors [1]. Calcification and Ossification of vertebral ligaments are common phenomenon. The ligaments may calcify or ossify when they sustain increased tension, torn or involved in lesions of vertebral bone or joints [8]. Osteophytes, commonly referred as bone spurs or parrot beak are bony projections that formed along joint margins. It forms naturally on the back of the spine as a person ages and are a sign of degeneration, mechanical instability and disease (DISH).
OBSERVATION AND RESULT
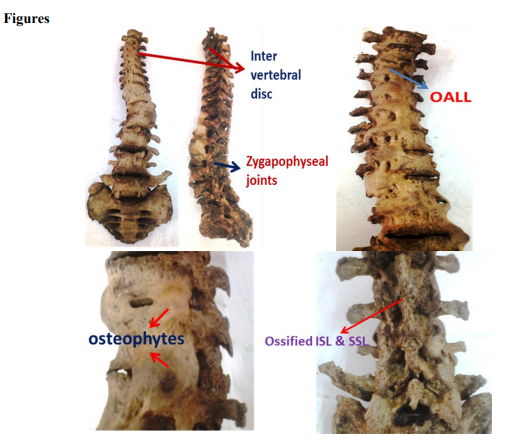
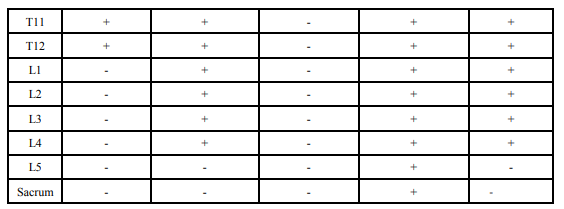
During routine osteology classes in BMCRI, Bangalore processed vertebrae were collected to explain to the students of I MBBS, we realized an abnormal column. It had ossification of vertebral ligaments (ALL, PLL, ISL, SSL), calcification of Zygapophyseal joints and osteophytes (Refer table and figures given below). Osteophytes present on the right side between T8-T9, T9-T10, L2-L3, L4-L5 And on the left side between T12-L1, L1-L2 and L3-L5.
DISCUSSION
The ossification of vertebral ligaments and zygopophyseal joints may lead to clinical signs and symptoms. These findings may result to conditions of Forestier’s disease, Bechterew’s disease[6]. OALL is diagnosed by plain lateral radiography and classified into 3 types: a. segmental, defined as partial or total ossification over a vertebral body without involving the disc space; b. continuous type showed ossification over many disc spaces as wellas the vertebral body; c. mixed type, combination of the segmental and continuous types[4]. OALL may be associated with spinal stenosis, precise neurological examination is critical. The most common symptoms of OALL are compression of esophagus and trachea. The DISH or Forestier’s disease as showing calcification or ossification along the anterior to anterolateral aspect of four contiguous vertebral bodies with relative preservation of the height of the intervertebral disc [4]. OPLL is an uncommon entity having a higher incidence in Japanese population. It is characterized by hyperplasia of cartilage cells with eventual endochondral ossification of PLL[5]. An abnormality in the N-propeptide of the COL 11A2 gene that related to type II collagen has been reported in patient with OPLL [2]. OPLL is more frequent in man than in women occuring in a ratio of 2:1[5]. The diagnosis of the disorder is usually established in the fifth to seventh decades of life [2.5]. The principle neurologic symptoms of OPLL divided into 3 groups: cord signs, manifested by dominant motor and sensory disturbances in the lower limb (56%); segmental signs, manifested by dominant motor and sensory disturbances in the upper limb (16%) and cervicobrachialgia, causing no obvious neurologic defects but associated with pain in the neck, shoulder and arm (28%) [5]. ISL, SSL ossification of a lumbar vertebrae can lead to compression of the cauda equina, which leading to abnormal bowel and bladder control, sensation of numbness in perineum and weakness in the thighs[1]. A strong association has been found that there is a genetic predisposition with AS. These patients have HLA –B27 positive in their laboratory findings. In certain races AS is related to Human Leucocyte Antingen(HLA) system which leads to ossification of all ligaments of vertebrae HLA complex gene located on short arm of chromose6[1]. In spondylosis the osteophtes are usually most common along the anterolateral aspect of the vertebral column; posterior excrescences are absent or of small size. In addition, osteophytes usually are triangular in shape, arising adjacent to the vertebral edge and extending in a horizontal direction [5]. The ossification of vertebral ligaments its intervertebral joints and discs leads to Bechterew’s disease in recent studies [6]. This disease begins at the age of 20-30. The main symptom is increasing of stiffness of the backbone and the restriction of thorax mobility at respiratory movements. Complications are the most dangerous for the affection of heart and aorta and patients have amyloidosis- the regeneration of kidneys leading to chronic renal insufficiency. The increasing of thorax mobility favors the development of pulmonary diseases [6].
CONCLUSION
Simple radiograph and MR Images may help in assessing normal or demonstrates the ossification of vertebral ligaments. It is said that both genetic and environmental (trauma) factors play a role in the pathogenesis of Forestier’s disease, Bechterew’s disease and Ankylosing Spondylitis [1,4,6]. The specimen obtained is rarely reported in the literature. The treatment for above is stem cells should be started at the onset of its first symptoms, before the ossification of all backbone and inflamed joints.

References:
1. S.Saritha, M.Preevan kumar, G.Supriya. Ossification of Interspinous and Suprespinous Ligaments of the Adult 5th Lumbar Vertebra and Its Clinical Significance- A Case Report. IOSR Journals,2012;1(5):27-28. www.iosrjournals.org
2. Haydar USUL, Ertugrul CAKIR, Erhan ARSLAN, Safak ERSOZ, Suleyman BAYKAL. Ossifying Fibroma of the Lumbar Spine- Case Report. Turkish Neurosurgey,2011;21(1):104-106.
3. Kazutoshi Hida, Shunsuke Yano, Yoshinobu Iwasaki. Considerations in the Treatment of Cervical Ossification of the Posterior Longitudinal Ligament. Clinical Neurosurgey,2008;55
4. J.Mizuno, H.Nakagawa, J.Song. Symptomatic Ossification of the Anterior Longitudinal Ligament with stenosis of the Cervical spine. J Bone Joint Surg Br,2005;87(10):1375-79
5. Brig Hariqbal Singh, Lt Col Vikram Khanna, Surg Lt Cdr Rajeev Sivasankar, Maj Ramesh Mothukuri. Ossification of Posterior Longitudinal Ligament.MJAFI 2004;60:284- 286.
6. Stammzellen, Hintergrundinfos, Und Aussichten. Bechterew’s disease. Stem cells,Neo Milenium.2007. Stammzellenmedizinede/en/bindegewebeerkrankungen/be chterew-krankheit.
7. Standaring S.Gray’s Anatomy, 38th editition, Newyork Churchill Livingstone.200O; 532- 536.
8. Albert Oppenheimer. Calcification and Ossification of Vertebral Ligaments. 1942; 38:160-173.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License