IJCRR - 5(6), March, 2013
Pages: 87-91
Date of Publication: 30-Mar-2013
Print Article
Download XML Download PDF
COMPARATIVE STUDY OF INTRATHECAL CLONIDINE AND INTRATHECAL BUPRENORPINE FOR POSTOPERATIVE ANALGESIA AFTER LOWER LIMB ORTHOPEDIC SURGERY
Author: Sapkal Pravin S., Kulkarni Kalyani D., Rajurkar Sampda S., Nandedkar Prerna D.
Category: Healthcare
Abstract:Objective: To evaluate and compare the efficacy, duration of post-operative analgesia and untoward effects of intrathecal Clonidine 60\?g and intrathecal Buprenorphine 60\?g used as additive adjuvants in spinal anesthesia for lower limb orthopaedic surgeries. Method: Total 80 patients, aged 20-60 yrs, belonging to ASA grade I and II undergoing elective or emergency lower limb orthopaedic surgery scheduled to last less than 180 minutes and fit to receive spinal analgesia were randomly allocated into two groups. Group C received intrathecal 0.5% heavy Bupivacaine 3.0 ml with Clonidine 60\?g and Group B received intrathecal 0.5%. Heavy Bupivacaine 3.0 ml with Buprenorphine 60\?g. Duration of subarachnoid block, total analgesia, effective analgesia, number of rescue analgesics and any untoward effects were assessed and compared in both groups. Results: Both groups were comparable in demographic data. The difference in the duration of subarachnoid block in both groups is statistically significant. The duration of total analgesia in both groups is statistically comparable. Effective analgesia in Clonidine group was statistically longer than Buprenorphine group. The nausea was noted in 17.5% of patients in Buprenorphine group and 7.5% patients in Clonidine group. Vomiting was present in 5% of patients in Buprenorphine group while none of the patient in Clonidine group had vomiting. Conclusion: This study concludes that intrathecal Clonidine 60\?g significantly prolongs the duration of spinal anesthesia and quality of analgesia was acceptable to patients in both groups though VAS assessment was better in Buprenorphine group. Hence we suggest that combination of low dose intrathecal \a2 agonist and opioid would give better analgesia & might reduce incidence of untoward effects.
Keywords: Effective analgesia, subarachnoid block, ?2 agonist, opoid.
Full Text:
INTRODUCTION
Severe acute postoperative pain itself can easily hinder early physiotherapy, which is the most important factor for successful postoperative knee rehabilitation especially following arthroscopic surgeries {1}. Buprenorphine is common & potent opioid which can be safely used intrathecally {2}. But such opioids are not devoid of side effects may be minor like pruritus, somnolence or may be distressing like nausea & vomiting or respiratory depression {3}. Clonidine an α2 agonist is another drug, which when used intrathecally gives good analgesia & is claimed to have no side effects like opioids {4}. But, Clonidine intrathecally may cause bradycardia, somnolence, and hypotension {1}. So we have decided to evaluate effects of intrathecal clonidine and compare it with intrathecal Buprenorphine in elective lower limb orthopedic surgeries.
MATERIALS AND METHODS
This was a prospective study of 80 patients who were randomly enrolled and allocated into either group after written and informed consent.
Inclusion criteria:
American Society of Anesthesiologist (A.S.A.) grade I & II patients, aged 20-60yrs, undergoing lower limb orthopedic surgery emergency or elective scheduled to last less than 180 minutes, and willing to participate in study.
Exclusion criteria:
Patient refusal, patient using α adrenergic receptor antagonist for any reason, patient receiving ACE inhibitors /β blockers, Dysrrhythmias on ECG, morbidly obese patients, contraindication to subarachnoid block, general or epidural anesthesia given in addition to subarachnoid block.
Preoperatively detailed medical, surgical history, allergies were noted. Preoperative detailed general & systemic examination was done and vitals recorded and necessary investigations were done. Demographic data like age, weight (kg), height (cm) obtained for each case. The patients were familiarized with the 10 cm visual analogue scale (V.A.S) for pain during the pre-anesthetic visit. Patients were kept fasting for 6-8hrs prior to anesthesia. After shifting the patients to operation theatre, baseline monitoring of E.C.G, noninvasive blood pressure, oxygen saturation, and respiratory rate were recorded. A 20 Gauge i.v line was established. All patients were preloaded with 10ml/kg of lactated Ringer solution over 15-20 minutes. The patients were randomly assigned to one of the study groups. The study drugs were prepared by an anesthetist not involved in patient assessment. After strict aseptic precautions a midline lumbar puncture was performed with a 26 gauge Quinke needle at the L3-4 interspace with patient in the sitting position. Intrathecal drugs were injected with the needle bevel pointing caudally and over a period of 30 seconds as follows: Group B: 3.0 ml of 0.5% Hyperbaric Bupivacaine + Buprenorphine 60 μg. Group C: 3.0 ml of 0.5% Hyperbaric Bupivacaine + Clonidine 60 μg. The haemodynamic parameters i.e. heart rate, blood pressure, respiratory rate and SpO2 were recorded just before the block and then every 5 minutes after the intrathecal injection until the end of the surgery and then post-operatively every 2hrs until 24 hrs. The level of sensory analgesia, degree of motor blockade and sedation score were recorded every 5 minutes until 30 minutes after the intrathecal injection. The level of sensory analgesia was assessed using 25 gauge short bevel needle and recorded as analgesia to loss of sensation to pin prick. Motor Blockade was determined according to the Modified Bromage Scale {5}. Sedation score was analyzed every 2 hrly during postoperative period for 24hrs.Sedation was analyzed as follows:- Regular intra-operative monitoring was done. Duration of anesthesia was recorded as time interval from intrathecal injection to regression of sensory block below L1. Intraoperative hypotension was defined as a fall of mean arterial pressure (M.A.P.) to less than 20% of baseline and was treated with rapid infusion of 200 ml of Lactated Ringer solution and / or 3 mg aliquots of injection mephenteramine intravenously. Bradycardia i.e.–heart rate less 50 / minute was treated with intravenous atropine sulphate with increments of 0.3 mg. No additional analgesic was given during intraoperative period.
Postoperative Evaluation:
The evaluation started immediately post-operatively. Following data were collected: pulse, NIBP, RR every 2hrly up to 24hrs. Assessment of analgesia by VAS every 1hr up to first dose of rescue analgesia & thereafter every 2 hrly & additionally if patient complained of pain, up to 24hrs. Assessment of data was done as:
1) Duration of subarachnoid block: Time from intrathecal injection up to regression of sensation (pinprick,) at L1 dermatome.
2) Total analgesia i.e. time from subarachnoid injection to first report of pain i.e. VAS≥1.
3) Effective analgesia i.e. time from subarachnoid injection to first parenteral rescue analgesia at VAS ≥4.
4) Presence and time of occurrence of any untoward effects like nausea, vomiting, pruritus, respiratory depression (i.e. RR<10/min at rest), bradycardia, dryness of mouth were noted. Nausea, vomiting treated with inj. Ondansetron 4 mg i.v. Bradycardia was treated with inj Atropine 0.6 mg i.v. stat and repeated if required.
After 24hrs, usual post operative care followed. When patient complained pain and demanded for additional analgesia i.e. VAS≥4, IV Tramadol 100 mg bolus was given slowly. The frequency of doses and time of such rescue analgesia were noted up to 24 hrs.
STATISTICAL ANALYSIS
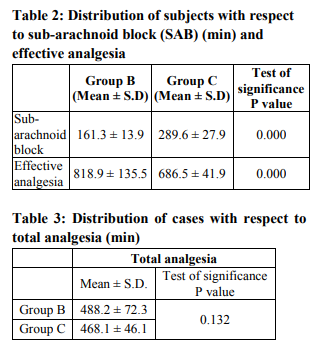
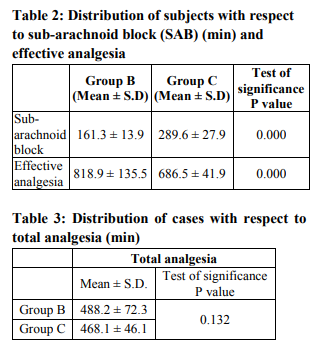
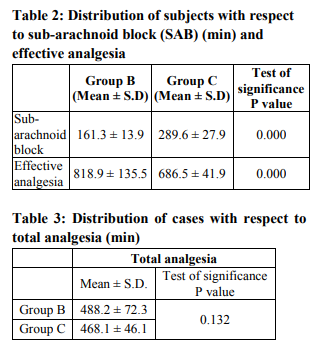
All values are reported as mean ± SD. Unpaired two?tailed Student‘t’ test was used to assess the significance of the differences in values of the parameters in cases and controls. Differences were considered statistically significant at a probability value P 0.05) both groups were found to be comparable with respect to age (yrs), weight (kgs), height (cms). Distribution of subjects with respect to subarachnoid block (SAB) (min) and effective analgesia in both the groups is in table- 2. By using Unpaired T-test (P-value < 0.05), therefore there is significant difference between both the groups with respect to sub-archonaid block (SAB) and effective analgesia. Distribution of cases with respect to total analgesia (min) in both the groups shown in table- 3. P-value > 0.05 in Unpaired T-test proves that both groups are comparable with respect to total analgesia (min.) The nausea was noted in 17.5% of patients in Buprenorphine group and 7.5% patients in Clonidine group. Vomiting was present in 5% of patients in Buprenorphine group while none of the patient in Clonidine group had vomiting. Other side effects noticed in Clonidine group were hypotension in 2.5% patients, bradycardia in 5% of patients and dryness of mouth in 10% of patients in Clonidine group. Somnolence was noticed slightly higher in Buprenorphine group i.e. 7.5% while, 2.5% in Clonidine group.
DISCUSSION
In the present study it is found that intrathecal Clonidine 60µg significantly prolongs the duration of spinal anaesthesia. Intrathecal Buprenorphine 60µg gives adequate analgesia up to 818.9 ± 135 min to which is significantly longer than that of intrathecal clonidine i.e. 686.5 ± 41.9 min. Similar finding was seen in Forgarthy DJ et.al{7}, Bonnet F et.al {8}, Sites BD et.al {9} and Gordh T {10}. In the present study intrathecal clonidine shown nausea, hypotension, bradycardia and dryness of mouth, While buprenorphine group shown nausea, vomiting and somnolence as side efffect. Eisenach J et.al[{11} found that Clonidine produces its antinociceptive, cardiovascular, and sedative effects by actions at multiple sites. Segal IS et.al {12} found that these effects depend upon site of administration while Filos KS et.al {13} proved that these depend upon dose and concomitant administration of other drugs. Study suggests that combination of two or more drugs from different group (e.g. Opioid and α 2 agonist) can give better analgesia and less chance of side effects.
CONCLUSION
Intrathecal Clonidine 60µg significantly prolongs the duration of spinal anesthesia. Intrathecal Buprenorphine 60µg gives adequate analgesia upto 818.9 ± 135min mins to whichsignificantly longer than that of intrathecal clonidine i.e. 686.5 ± 41.9 min. Quality of analgesia was acceptable to patients in both groups though VAS assessment was better in Buprenorphine group. We further suggest that combination of low dose intrathecal alpha 2 agonist and opioid would give better analgesia & might reduce incidence of untoward effects.
ACKNOWLEDGEMENT
Authors acknowledge the great help received from the scholars whose articles cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. Authors are grateful to IJCRR editorial board members and IJCRR team of reviewers who have helped to bring quality to this manuscript.

References:
1. Eisenach J, De Kock M, Klimscha W. Alpha2- Adrenergic agonists for regional anesthesia: a Clinical review of clonidine (1984-1995). Anesthesiology 1996; 85:655- 74.
2. Verma RS, Patodiv, et al. Post operative pain relief with intrathecal buprenorphine. Ind Jour of Anaesthesia 1991; 89 : 32-3
3. Boas RA, Villiger JW. Clinical actions of fentanyl and buprenorphine. Br J Anaesth 1985; 57: 192–6.
4. Gradhe RP, Wig J, Yaddanapudi L N: Evaluation of Bupivacaine-Clonidine for unilateral spinal anaesthesia in lower limb orthopedic surgery.J Anas clin pharmacol 2008; 24(2):155-8.
5. Bromage PR.A comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesia. Acta Anaesthesiol Scand 1965; 16 (Suppl): 55-69
6. IBM SPSS Statistics [computer program].Version 19.0.0. Somers (NY): IBM coporation;2010
7. Forgarthy DJ, Caranine UA, Milligan KR. Comparison of the analgesic effects of intrathecal clonidine and intrathecal morphine after spinal anaesthesia in patients undergoing total hip replacement. Br. J. Anesthesia, 1993;71: 661-4.
8. Bonnet F. Buisson VB, Francois Y, et al . Effects of oral and subarachnoid clonidine on spin Capogna G, Celleno D, Tagariello V, Loffreda-Mancinelli C. Intrathecal buprenorphine for postoperative analgesia in the elderly patient. Anaesthesia 1988; 43: 128
9. Sites BD, Christopher R, Biggs R, Beach ML, Wiley C. Intrathecal clonidine added to a bupivacaine-morphine spinal improves postoperative analgesia following total knee arthroplasty. Indian J Anesth 2002; 96: 918.
10. Gordh T Jr. Epidural clonidine for treatment of postoperative pain after thoracoscopy. A double blind placebo-controlled study. Acta Anesthesiol Scand. 1988;32:702-9.
11. Eisenach J, Detweller D, Hood D. Hemodynamic and analgesic actions of epidurally administered Clonidine. Anesthesiology 1993; 78: 277-87.
12. Segal IS, Jarvis DJ, Duncan SR, White PF, Maze M. Clinical efficacy of oraltransdermal Clonidine combinations during
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License